Background: Group medical visits (GMV) have been shown to improve metrics in patients with type 2 diabetes mellitus (DM). Overlook Family Medicine, a teaching residency program, anticipated that medical residents trained in the GMV model of care by interdisciplinary team members may improve cholesterol, HbA1C, BMI, and blood pressure in patients. The objective of this study was to compare metrics between group 1: GMV patients with DM whose primary care provider (PCP) was an attending physician/nurse practitioner (NP) and group 2: GMV patients with DM whose PCP was a family medicine (FM) medical resident receiving GMV training. We seek to provide guidance on implementation of GMV in residency teaching practices.
Methods: We performed a retrospective analysis to evaluate total cholesterol, LDL, HDL, TG, BMI, HbA1C, and BP in GMV patients between 2015-2018. We used a t test to compare outcomes between the two groups. Diabetes training was provided to family medicine residents by an interdisciplinary team.
Results: There were 113 patients enrolled in the study: 53 in group 1 and 60 in group 2. There was a statistically significant decrease in LDL and triglycerides, and an increase in HDL in group 2 (P<.05). There was a clinically significant decrease in HbA1C in group 2 (-0.56, P=.0622).
Conclusion: Sustainability of GMV can be achieved with a champion diabetes education specialist. Interdisciplinary team members are integral in training residents and addressing patients’ barriers. GMV training should be incorporated into family medicine residency programs to improve metrics for patients with diabetes. FM residents who received interdisciplinary training had improved metrics in GMV patients compared to patients whose providers did not. Therefore, GMV training should be incorporated into family medicine residency programs to improve metrics for patients with diabetes.
Group medical visits (GMV) have been shown to improve quality metrics in patients with type 2 diabetes mellitus (DM), empower patients to facilitate diabetes self-management, and develop fellowship among patients.1,2 GMV in family medicine (FM) residency programs have not been well evaluated. A previous study surveyed FM program directors to determine whether GMV were offered. Although 79.2% of those surveyed agreed that training FM residents in the GMV model of care is important, only 59% (137/252) of program directors reported that GMV were offered. Challenges cited included a lack of expertise and time among faculty to implement GMV.3 Addressing challenges related to sustaining GMV has not been adequately discussed.4–6
Overlook Family Medicine (OFM), a teaching residency program, incorporated GMV in 2013. We anticipated an improvement in total cholesterol (TC), LDL, HDL, triglycerides (TG), body mass index (BMI), hemoglobin A1C (HbA1C), and blood pressure (BP) in GMV patients managed by FM residents trained in the GMV model of care. The objective of this study was to compare metrics between group 1: GMV patients with type 2 DM whose primary care provider (PCP) was an attending physician/nurse practitioner (NP), and group 2: GMV patients with type 2 DM whose PCP was a FM resident trained by interdisciplinary team members. We sought to provide guidance on implementation of GMV to improve metrics in patients with type 2 DM in residency teaching practices.
We conducted a retrospective study in adults with type 2 DM with a HbA1C ≥ 6.5%, who were enrolled in GMV from 2015 to 2018. A total of 25 GMV were offered in English and six in Spanish. Patients attended GMV according to their preferred language. Adults who attended at least one GMV were included. The baseline data included HbA1C, TC, LDL, HDL, and TG. BP and BMI were taken at each GMV. Metrics were compared between group 1 and group 2. Endpoint data were 0-6 months after the last GMV attended. GMV were held in the evening on weekdays at OFM. Approximately five patients attended each GMV, which did not replace the diabetes office visit. The patients’ PCP was identified by the electronic medical record.
Two FM residents attended each GMV and moderated the “Know Your Numbers” GMV. A nutritionist, pharmacist, physical therapist, and yoga instructor moderated their topics. Attending physicians did not moderate GMV, however one attending and NP were present at each GMV. Diabetes care education was provided to medical residents by a clinical pharmacist, NP/Certified Diabetes Care and Education Specialist (CDCES), and a behaviorist during monthly conferences. Topics included diabetes self-management education, nutrition, pharmacotherapy, and motivational interviewing. PCPs recruited their patients and high-risk patients were identified using population health registries. Minitab v17 software was utilized to analyze data using a t test and Kolmogorov-Smirnov (K-S) determined distribution.
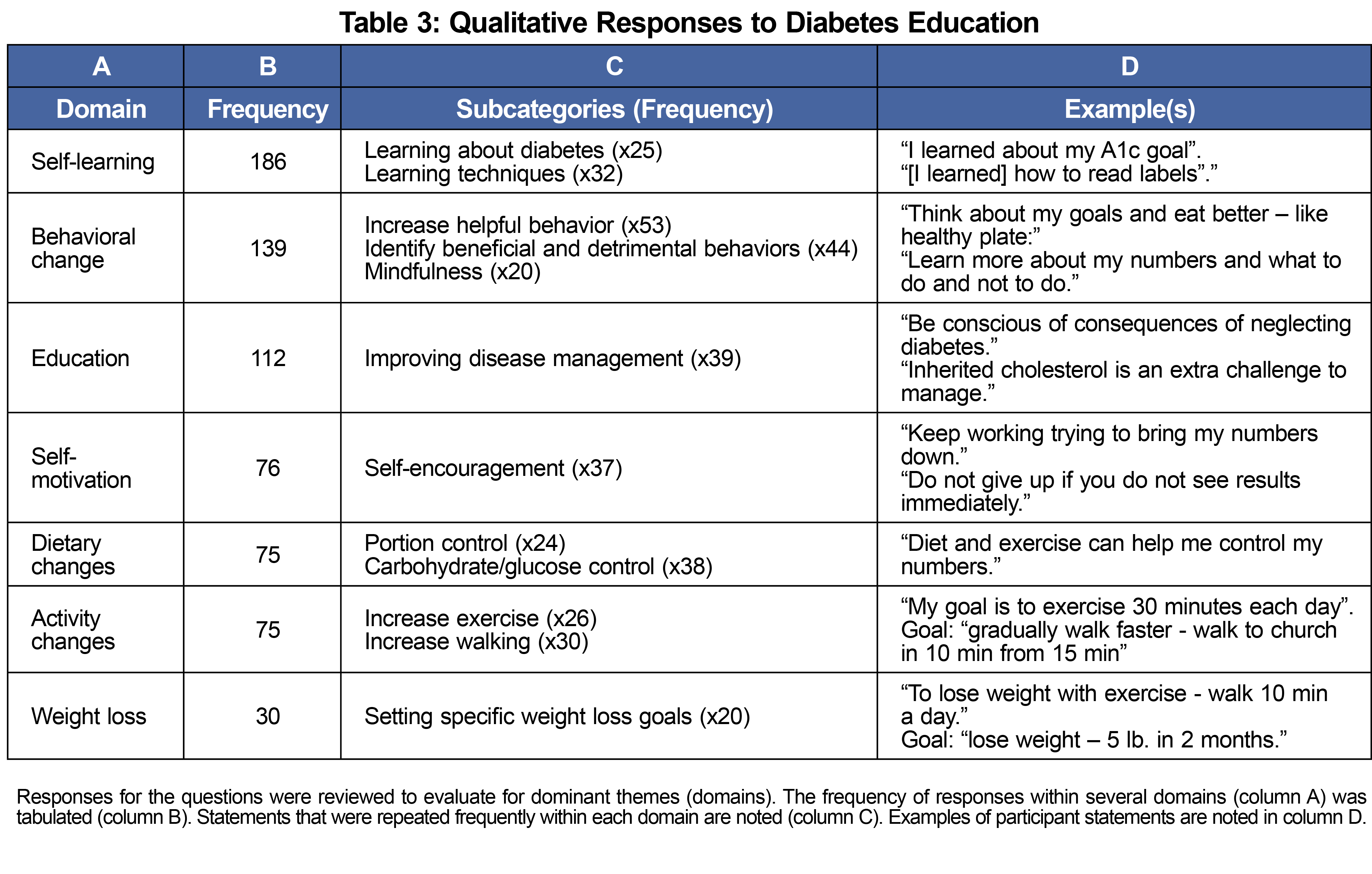
A survey generated by the NP/CDCES was administered to patients to assess patient-perceived value on a scale of 1 to 5, lowest to highest. Questions asked included “Was the topic useful?”, “Was the speaker knowledgeable?”, and “Was the program well-organized?" Patients listed two learned concepts and set two goals. We analyzed qualitative responses using a modified version of the consensual qualitative research method. The study was granted an exemption by Atlantic Health System’s institutional review board.
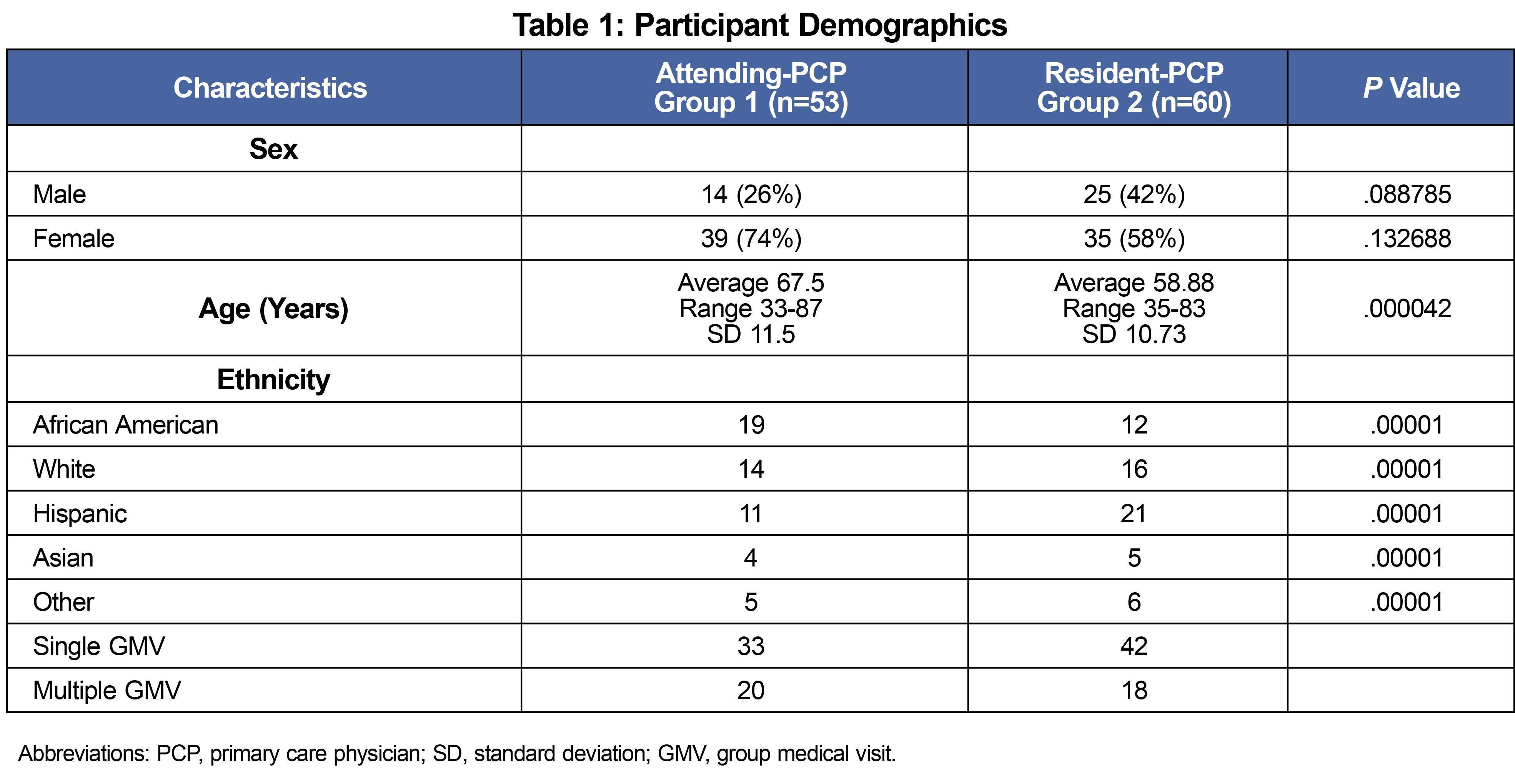
One hundred-eighteen patients participated in GMV and 113 were enrolled. Five were excluded due to relocation (1), prediabetes (3), and incomplete data (1). There were 53 patients in group 1 and 60 patients in group 2. There was a significant difference in ethnic groups represented in group 2 (Table 1). The average age in group 1 (67.5) was higher than in group 2 (58.9).
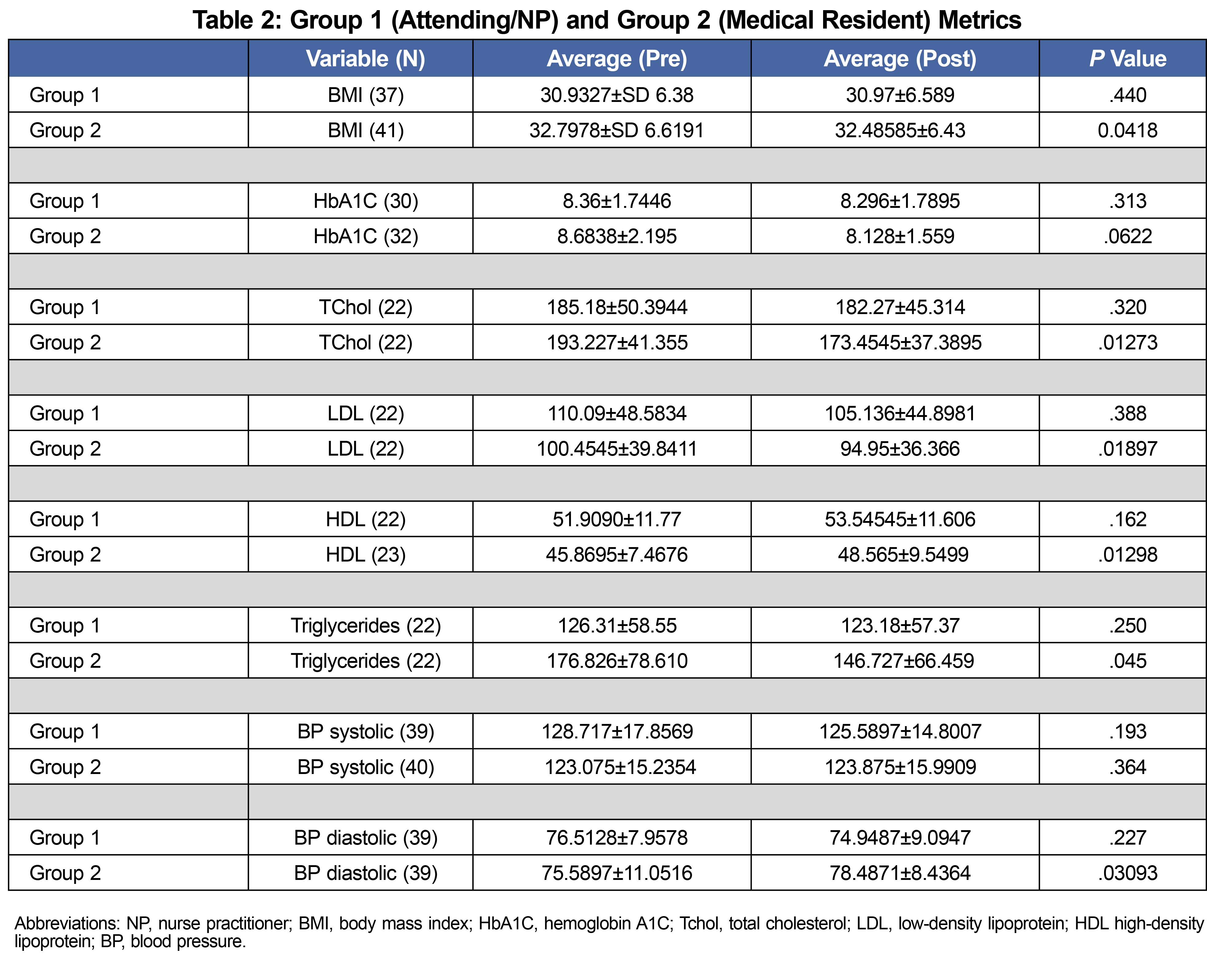
In group 1 there were no statistically significant changes in the metrics evaluated (Table 2). Group 2 had a reduction in TG: 176.8 mg/dl to 146.7 mg/dl, and LDL: 100.45 mg/dl to 94.45 mg/dl, and an increase in HDL: 45.8 mg/dl to 48.5 mg/dl (P<.05). There was a clinically significant decrease in HbA1C in Group 2: 8.68% to 8.128% (P=.0622; Table 2).
All 113 participants completed a qualitative survey at the conclusion of the GMV. In both groups, most participants reported goals which reflected skill acquisition, and measurable behavioral changes (Table 3).
GMV patients receiving care from FM residents had improved LDL, TG, HDL, and HbA1C. The difference in metrics between the groups may be attributed to the team-based diabetes education received by FM residents. Residents trained in the GMV model of care may have gained additional perspectives of the complexity of patient experience and confidence in their ability to teach and communicate.7 The mean baseline HbA1c was lower in group 1 and the average age of patients was greater. Consequently, group 1 patients may have had less stringent HbA1C goals. Study limitations were that insurance status and language preference was not retrievable and some patients attended multiple GMV (n=39), while others attended a single GMV(n=74). However, the number of patients attending multiple GMV was similar in both groups (Table 1). Patient scheduling conflicts, insurance status, and lack of follow-up obtaining labs posed challenges. Consequently, an office-based community health worker (CHW) contacted patients with HbA1C ≥9% to screen for barriers. Approximately 50% of these patients preferred Spanish as a primary language and 35% were uninsured. Previous literature cited communication and scheduling as barriers to resident participation in GMV.5 Therefore, evening office hours were replaced with the GMV to ensure participation. Residents invited their patients, which facilitated continuity and contributed to participant willingness to express goals.
Next steps include offering more GMV in Spanish, drawing labs at the GMV, and addressing SDOH. Sustainability and consistent resident training can be achieved with a champion NP/CDCES who ensures that GMV are a center wide initiative.8
This study demonstrates the impact of comprehensive, team-based care within a FM residency program that addresses the needs of the patient community.9 FM residents who cofacilitated GMV and received interdisciplinary training had improved metrics in patients compared to patients whose providers did not. Therefore, we recommend GMV training as an adjunct for diabetes care in FM residency programs.
Acknowledgments
Presentations: Demographic data for patients involved in this study were presented at the 2019 STFM Annual Spring Conference in Toronto, Ontario, Canada.
References
- Housden L, Wong ST, Dawes M. Effectiveness of group medical visits for improving diabetes care: a systematic review and meta-analysis. CMAJ. 2013;185(13):E635-E644. doi:10.1503/cmaj.130053
- Kirsh SR, Aron DC, Johnson KD, et al. A realist review of shared medical appointments: How, for whom, and under what circumstances do they work? BMC Health Serv Res. 2017;17(1):113. doi:10.1186/s12913-017-2064-z
- Strickland C, Sandberg JC, Davis SW, Weaver SP. Group medical visit training in family medicine residency: a 2015 CERA program directors survey. Fam Med. 2019;51(4):319-325. doi:10.22454/FamMed.2019.316336
- Housden LM, Wong ST. Using group medical visits with those who have diabetes: examining the evidence. Curr Diab Rep. 2016;16(12):134. doi:10.1007/s11892-016-0817-4
- Wheelock C, Savageau JA, Silk H, Lee S. Improving the health of diabetic patients through resident-initiated group visits. Fam Med. 2009;41(2):116-119. Accessed June 22, 2022. https://pubmed.ncbi.nlm.nih.gov/19184689/
- Cunningham AT, Delgado DJ, Jackson JD, et al. Evaluation of an ongoing diabetes group medical visit in a family medicine practice. J Am Board Fam Med. 2018;31(2):279-281. doi:10.3122/jabfm.2018.02.170373
- Kirsh SR, Schaub K, Aron DC. Shared medical appointments: a potential venue for education in interprofessional care. Qual Manag Health Care. 2009;18(3):217-224. doi:10.1097/QMH.0b013e3181aea27d
- Watts SA, Gee J, O’Day ME, et al. Nurse practitioner-led multidisciplinary teams to improve chronic illness care: the unique strengths of nurse practitioners applied to shared medical appointments/group visits. J Am Acad Nurse Pract. 2009;21(3):167-172. doi:10.1111/j.1745-7599.2008.00379.x
- Kahn NB Jr. Redesigning family medicine training to meet the emerging health care needs of patients and communities: be the change we wish to see. Fam Med. 2021;53(7):499-505. doi:10.22454/FamMed.2021.897904