Point-of-care ultrasound (POCUS) is an important diagnostic, clinical, and procedural tool that improves quality of care and positively impacts patient safety.1 POCUS is used to answer specific clinical questions and is often at the front line of imaging modalities due to its lack of ionizing radiation and relatively low cost.2 POCUS also provides a dynamic approach to teaching anatomy and physiology, enhancement of physical exam skills, and provides real-time feedback during the evaluation of various pathologies, which aids in medical decision making.1-5 In the last 10 years, the use of POCUS has risen dramatically, due in large part to mounting evidence that it is both an effective tool in clinical practice and part of an active learning model for medical students.6,7 Previous studies have detailed the implementation and evolution of POCUS as part of the medical student curriculum at medical schools in the United States. They concluded that integrated ultrasound curriculum is an effective active learning tool that can be applied to numerous clinical settings and can be effectively implemented into a competency-based model of medical education.1,6 Medical students have reported that ultrasound education enhanced their ability to learn anatomy and the physical exam.2,8,9,10 Furthermore, there are numerous opportunities to incorporate POCUS into undergraduate medical education, including within flipped classrooms, clinical skills examinations, and small-group clinical cases.1,2,5,6 Our study evaluated students’ perceptions of the benefits of POCUS and looked for improvement in musculoskeletal exam skills.
RESEARCH BRIEF
Using Ultrasound to Augment Exam Skills Among Clerkship Students
David Embers, MD | Nicole T. Yedlinsky, MD
PRiMER. 2023;7:39.
Published: 11/27/2023 | DOI: 10.22454/PRiMER.2023.183911
Introduction: Point-of-care ultrasound (POCUS) is becoming more common as a diagnostic and clinical tool. Some medical schools have incorporated POCUS training in their curriculum. A family medicine clerkship during the third year of undergraduate medical education is appropriate for incorporating musculoskeletal (MSK) education. Musculoskeletal ultrasound (MSKUS) is a potential tool for augmenting this teaching.
Methods: Third-year undergraduate family medicine clerkship students were given prework related to ultrasound physics, terminology, and sonographic appearance of MSK structures. This was followed by a 2-hour session in the first week of their clerkship covering the shoulder and knee MSK exams, and incorporated hands-on scanning. Students practiced MSK exams during their 8-week clerkship and POCUS was available in clinic. They were administered a postsession survey to rate the MSKUS curriculum. Objective, structured clinical exam (OSCE) testing, including performance evaluation of the knee examination during the final clerkship week, was compared to prior-year OSCE scores.
Results: Third-year medical students felt the use of MSKUS was helpful and enhanced overall understanding of MSK exams. We did not see an improvement in OSCE scores. Students reported a desire for more POCUS training.
Conclusion: POCUS is a powerful tool within the clinical and academic setting. We were able to develop a curriculum using MSKUS to augment teaching the shoulder and knee exams to third-year family medicine clerkship students. While we did not see an improvement in OSCE scores evaluating the performance of a knee exam, students reported greater understanding of the exams with the MSKUS instruction added. Students desire more POCUS training in the undergraduate medical curriculum.
Participants and Intervention
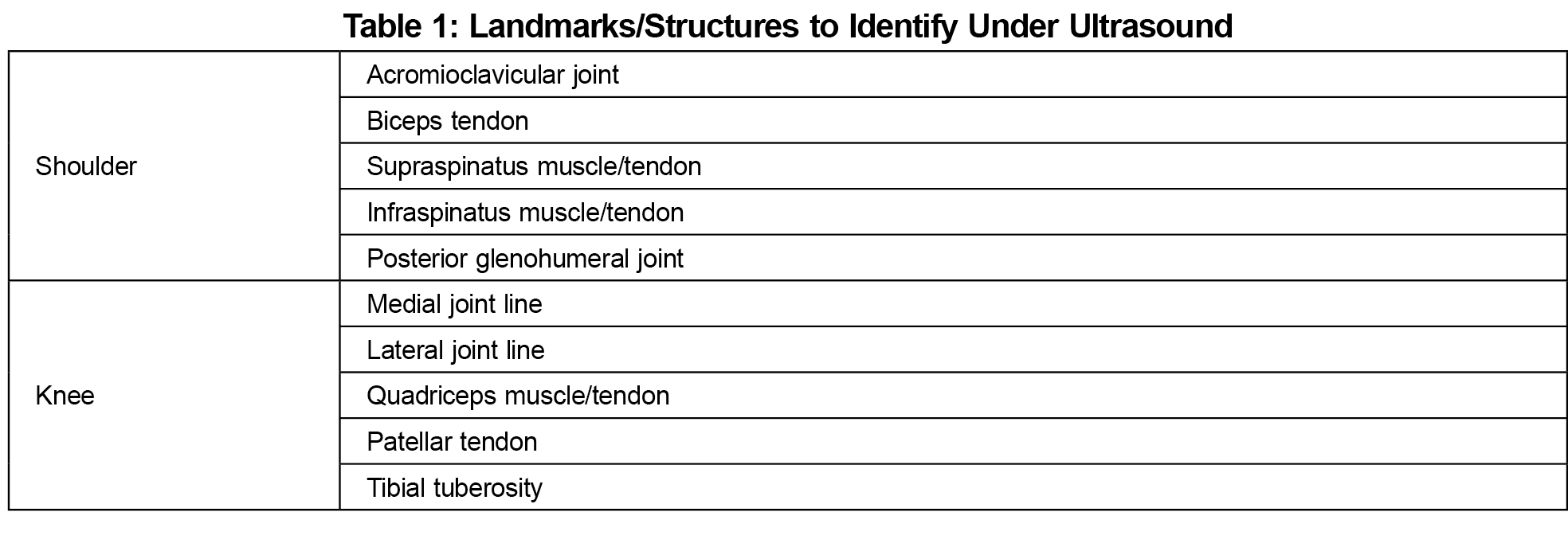
Our study included third-year family medicine clerkship students from academic years 2019-2020 and 2020-2021 at the University of Kansas School of Medicine. The 2019 and 2020 classes each consisted of 103 students on the Kansas City campus. These classes had an average age of 23.5 and 23.6 years at time of matriculation, respectively. The 2019 class was 51% male, 49% female. The 2020 class was 49% male, 51% female. The family medicine clerkship was required for all students. Students were given 30-minute prework videos covering ultrasound physics and terminology, and sonographic appearance of musculoskeletal (MSK) structures. All students then participated in a 2-hour session, during the first week of their clerkship, that taught the shoulder and knee exams by incorporating hands-on ultrasonography of the relevant anatomy (Table 1) by sports medicine and ultrasound-trained faculty. The students were divided into small groups to practice using handheld ultrasound devices.
Evaluation and Statistical Analysis
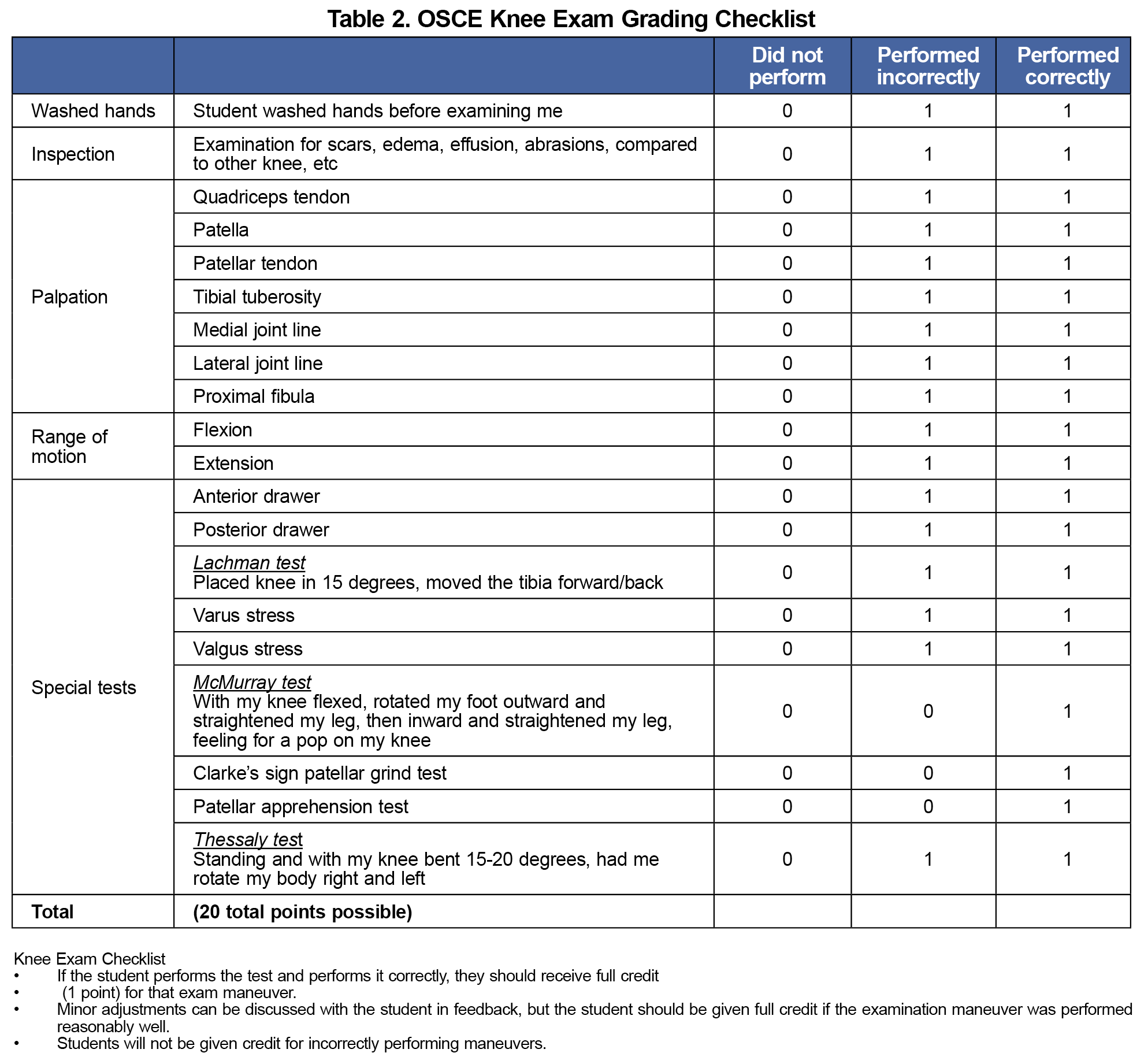
We evaluated the intervention at Kirkpatrick Levels 1 (reaction) and 2 (learning).11, 12 First, we administered an ultrasound curriculum evaluation to the students using a 5-point scale (strongly agree, agree, neutral, disagree, strongly disagree). Second, to evaluate learning, the students were tested using an objective structured clinical examination (OSCE) assessment during the final week of their 8-week family medicine clerkship. This included a performance evaluation of the knee examination (Table 2) but did not require competency in ultrasonography. We compared OSCE score distribution of students in the 2020-2021 academic year (which included ultrasonography-augmented instruction) to the 2019-2020 academic year (which lacked US-augmented instruction) using the Wilcoxon rank-sum test. The University of Kansas Medical Center Institutional Review Board approved this project.
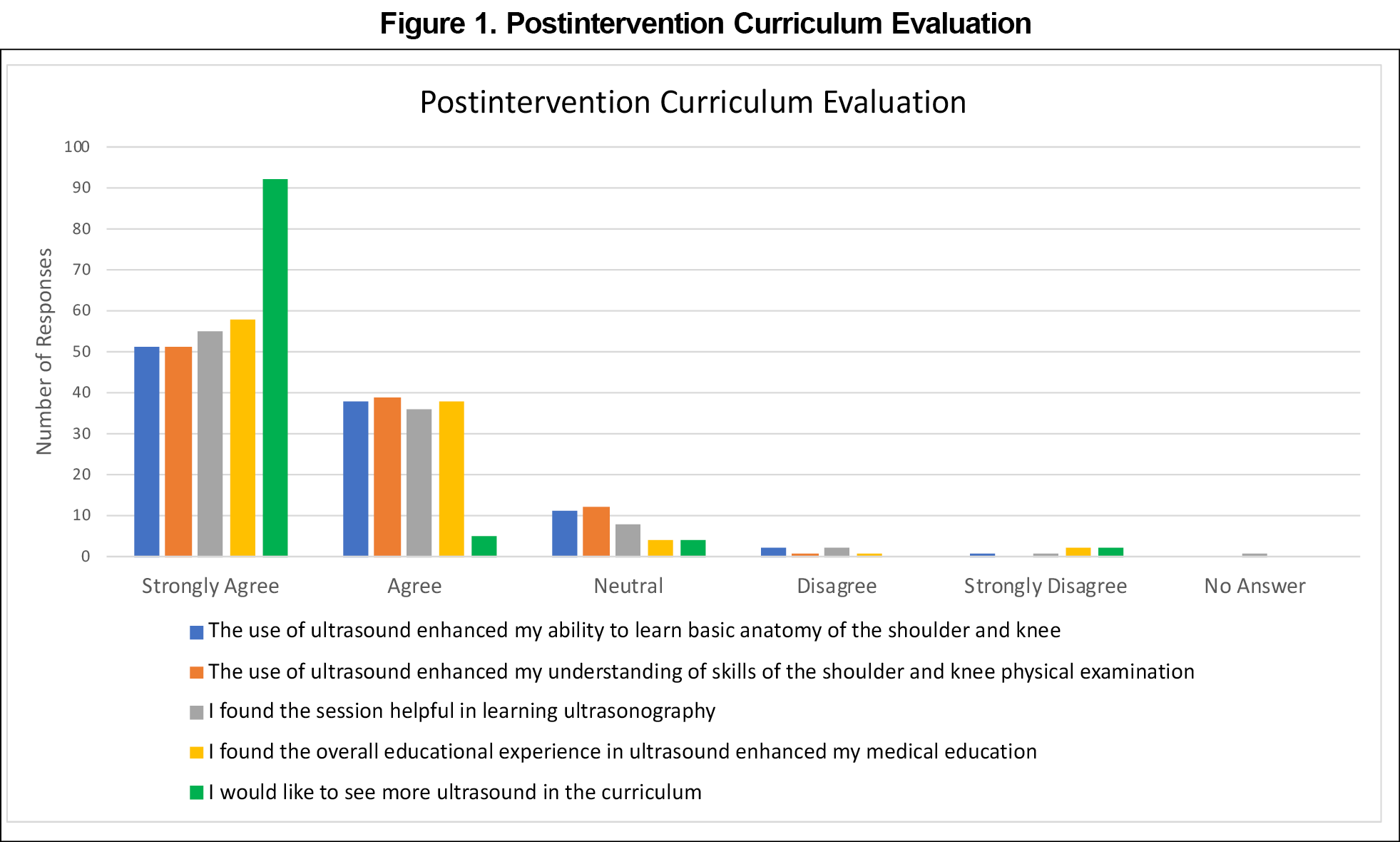
All 103 eligible students participated. Students felt that ultrasonography enhanced their ability to learn shoulder and knee anatomy (87% agree/strongly agree; Figure 1) and perform the relevant physical exams (88%). Most students found the session helpful in learning ultrasonography (90%). Most students agreed the ultrasound guided educational experience enhanced their medical education (95%) and almost all students wanted more inclusion of ultrasonography in the clerkship curriculum (95%).
Nevertheless, we failed to find evidence that this intervention improved clinical exam skills at 8 weeks. In 2019-2020, the mean OSCE score was 17.02 out of 20 (SD 1.77). For 2020-2021, after the intervention, the mean OSCE score was 16.64 (SD 2.51). This difference was not statistically significant (Wilcoxon P=.606).
Musculoskeletal concerns are a common condition in primary care and the family medicine clerkship is uniquely suited to teaching musculoskeletal exams. Despite its well-studied benefits for many specialties and applications, POCUS training in undergraduate medical education is limited by time and resources.2,6,9 Our study shows that integrating ultrasound education into medical clerkships is of significant interest to undergraduate medical students. This finding confirms results from studies at other institutions.8,10
In our study, however, POCUS-augmented teaching did not improve OSCE scores measured at 8 weeks posttraining. This was surprising because others have found that ultrasound-enhanced curricula do lead to increased learning.1,4,6,9 We speculate that the lack of effects at Kirkpatrick level 2 in our study might have been from slight curricular changes from year to year. Additionally, it is possible the specific knowledge being tested on the OSCE did not fully reflect the depth and breadth of information added when anatomy and exam skills were supplemented by ultrasound. These hypotheses should be considered in future studies.
Our study has limitations. This was a year-to-year data comparison study where other curricular changes may have impacted participant performance. Additionally, our study was at least partly performed during the COVID-19 pandemic, a variable that likely had an impact. A randomized study utilizing a control group compared to a group with additional ultrasound education from the same academic year would have controlled some of these variables. Additionally, this was a single-center study that would benefit from expansion to a multicenter study.
Although our study focused on musculoskeletal exam education, applications for POCUS are numerous.4,5 Further studies comparing curricula focused on other organ systems, clinical settings, or diagnostic criteria are needed. The challenge educators face is the implementation of a streamlined curriculum that benefits learners and efficiently enhances their medical education.1,2,9 Barriers such as access to ultrasound machines, standardized testing practices, and qualified faculty to teach image acquisition and interpretation remain.2,5,9
Acknowledgments
Financial Support: This work was funded by a MAITF Grant. It utilized the REDCap electronic management data system at the University of Kansas Medical Center which was supported by a CTSA grant from NCATS awarded to the University of Kansas for Frontiers: University of Kansas Clinical and Translational Science Institute (# UL1TR002366).
References
- Hoppmann RA, Rao VV, Bell F, et al. The evolution of an integrated ultrasound curriculum (iUSC) for medical students: 9-year experience. Crit Ultrasound J. 2015;7(1):18. doi:10.1186/s13089-015-0035-3
- So S, Patel RM, Orebaugh SL. Ultrasound imaging in medical student education: impact on learning anatomy and physical diagnosis. Anat Sci Educ. 2017;10(2):176-189. doi:10.1002/ase.1630
- Walrod BJ, Schroeder A, Conroy MJ, et al. Does ultrasound-enhanced instruction of musculoskeletal anatomy improve physical examination skills of first-year medical students? J Ultrasound Med. 2018;37(1):225-232. doi:10.1002/jum.14322
- Arora S, Cheung AC, Tarique U, Agarwal A, Firdouse M, Ailon J. First-year medical students use of ultrasound or physical examination to diagnose hepatomegaly and ascites: a randomized controlled trial. J Ultrasound. 2017;20(3):199-204. doi:10.1007/s40477-017-0261-6
- Flick D. Bedside ultrasound education in primary care. J Ultrasound Med. 2016;35(7):1369-1371. doi:10.7863/ultra.15.08073
- Kondrashova T, Kondrashov P. Integration of ultrasonography into the undergraduate medical curriculum: seven years of experience. Mo Med. 2018;115(1):38-43.
- Hall JW, Holman H, Bornemann P, et al. Point of care ultrasound in family medicine residency programs: a cera study. Fam Med. 2015;47(9):706-711. PMID:26473563
- Tarique U, Tang B, Singh M, Kulasegaram KM, Ailon J. ultrasound curricula in undergraduate medical education: a scoping review. J Ultrasound Med. 2018;37(1):69-82. doi:10.1002/jum.14333
- Haidar DA, Kessler R, Khanna NK, et al. Association of a longitudinal, preclinical ultrasound curriculum with medical student performance. BMC Med Educ. 2022;22(1):50. doi:10.1186/s12909-022-03108-0
- Ferderber ML, Vann K, Tzaras A, Hadadi N, Gilbird RM. Evaluation of a musculoskeletal ultrasound workshop in the family medicine clerkship. Fam Med. 2022;54(1):54-57. doi:10.22454/FamMed.2022.378370
- Kirkpatrick model. Poorvu Center for Teaching and Learning. January 10, 2019. Accessed January 27, 2023. https://poorvucenter.yale.edu/Kirkpatrick
- MindTools. Kirkpatrick’s Model. Accessed January 23, 2023. https://www.mindtools.com/ak1yhhs/kirkpatricks-four-level-training-evaluation-model
Lead Author
David Embers, MD
Affiliations: Department of Family Medicine and Community Health, University of Kansas Medical Center, Kansas City, KS
Co-Authors
Nicole T. Yedlinsky, MD - Department of Family Medicine and Community Health, University of Kansas Medical Center, Kansas City, KS
Corresponding Author
Nicole T. Yedlinsky, MD
Correspondence: Department of Family Medicine and Community Health, University of Kansas Medical Center, 3901 Rainbow Blvd, MS 4010, Kansas City, KS
Email: nyedlinsky@kumc.edu
Fetching other articles... 
Loading the comment form... 
Submitting your comment... 


There are no comments for this article.