Introduction: The Education-Centered Medical Home (ECMH) is a longitudinal clerkship that emphasizes continuity and quality improvement in primary care. We aimed to evaluate our ECMH’s ability to improve type 2 diabetes mellitus (T2DM) care through a systematic chart audit and care planning process. The effect of this intervention was measured by adherence to process and outcome measures.
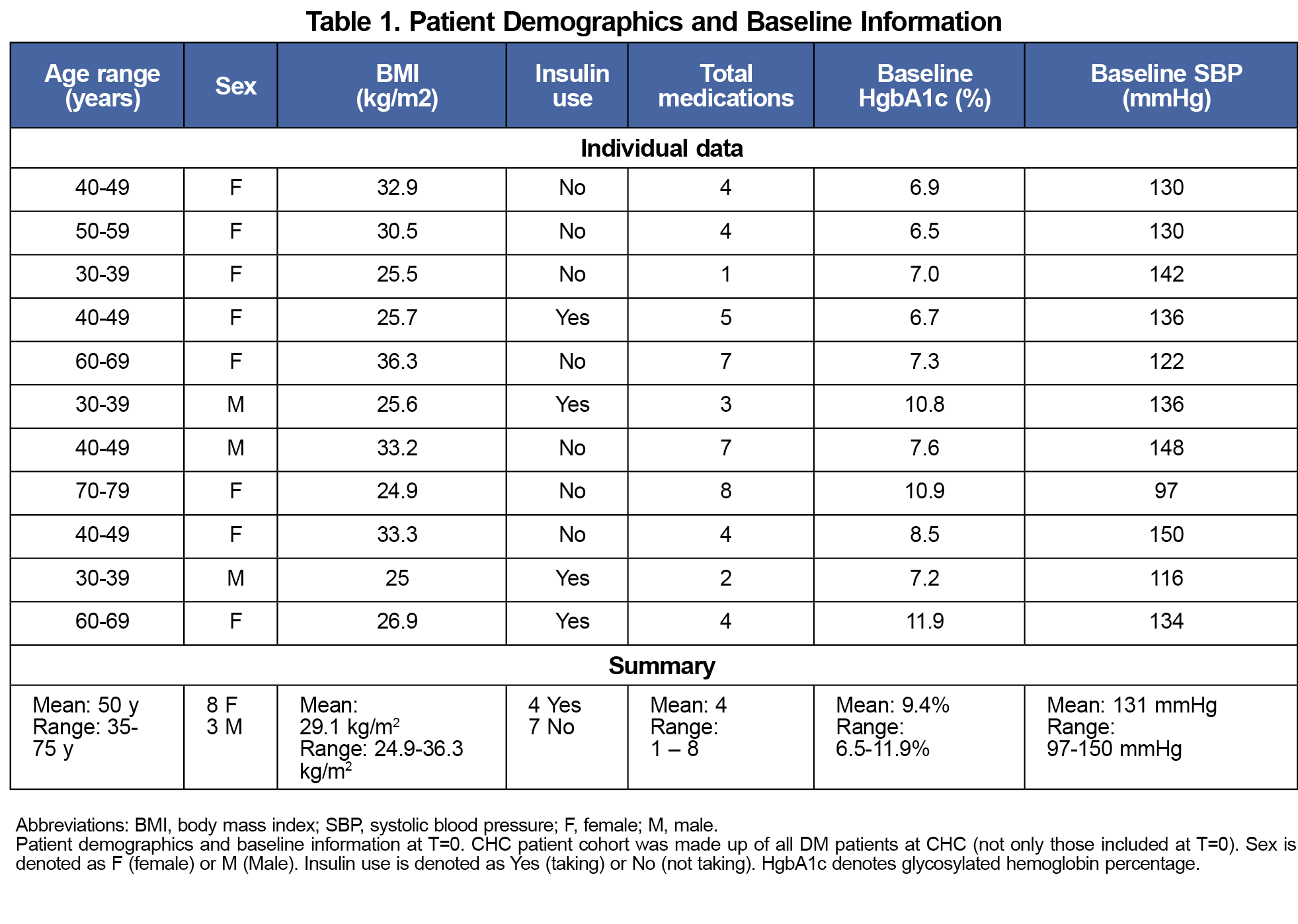
Methods: From November 2015 to March 2017, medical students were educated on and performed monthly chart audits of guideline-based quality metrics: hemoglobin A1c systolic blood pressure; lipid and microalbuminuria evaluation; annual ophthalmic and foot examinations; flu, hepatitis, and pneumonia vaccination; and statin therapy. Patients were included if they had a diagnosis of T2DM and were seen by the ECMH clinic before and after the audits started. Students shared audit logs, using them to plan patient appointments. We assessed changes in proportion of patients meeting each guideline with Fisher’s exact test.
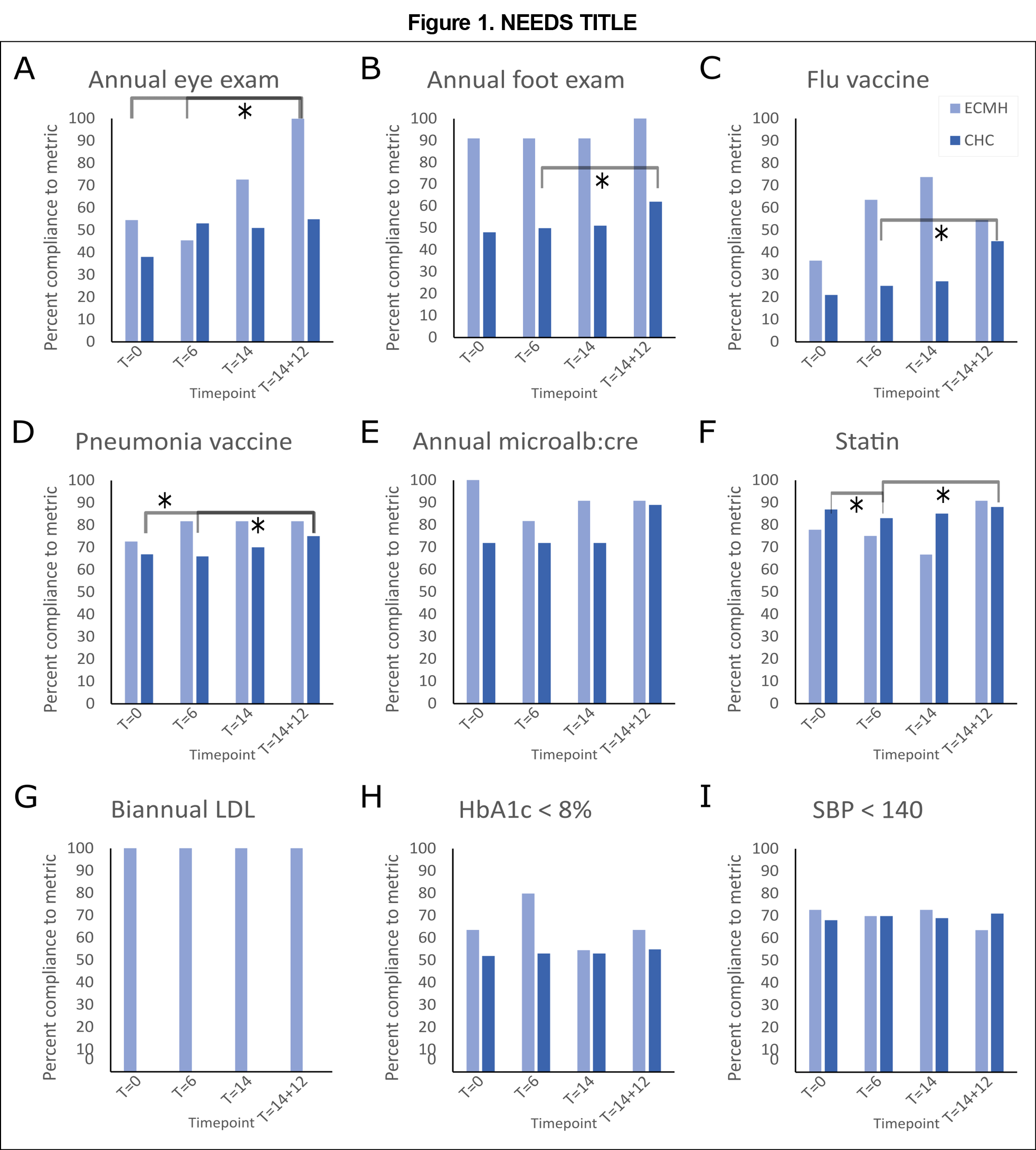
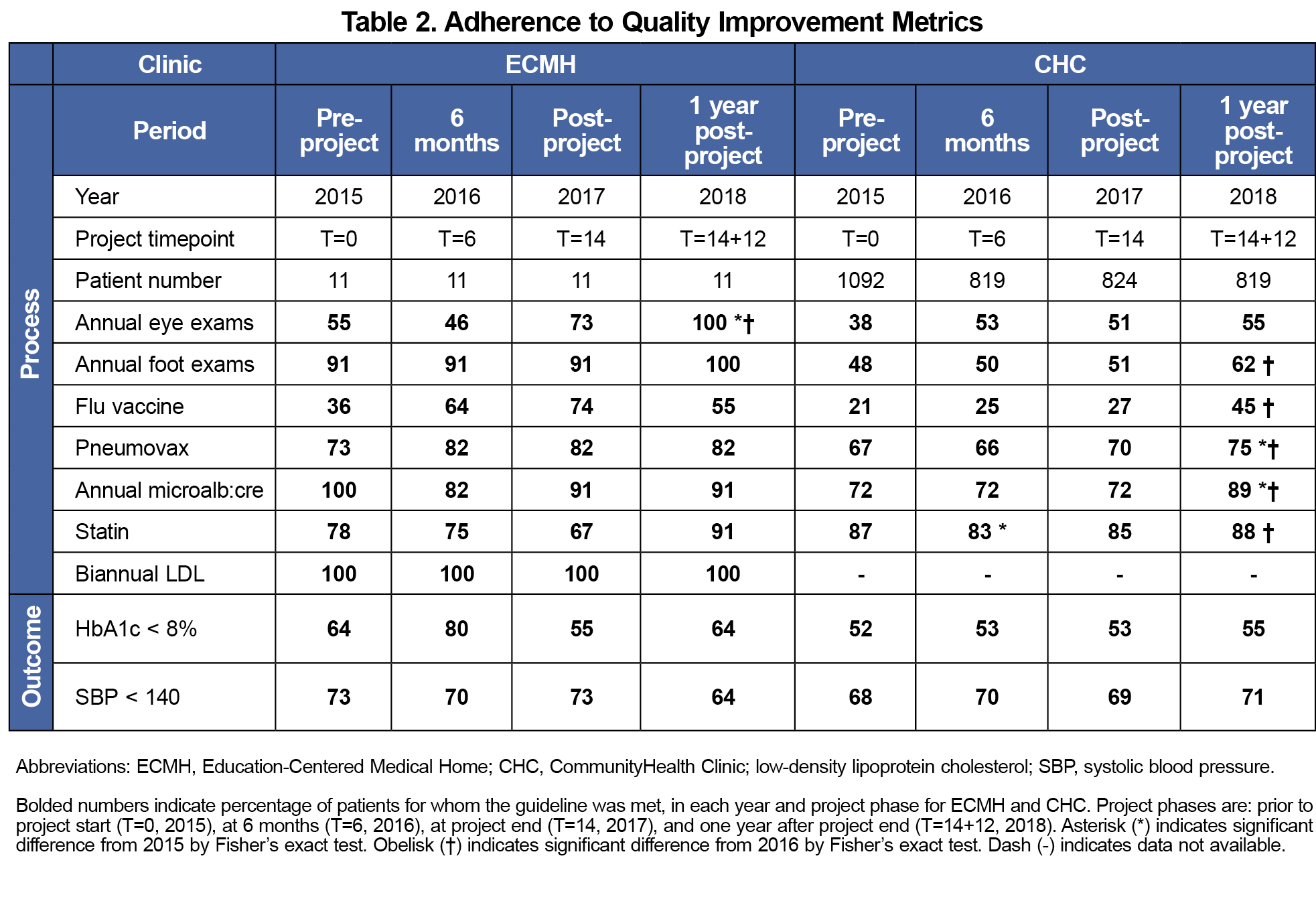
Results: The project included 11 patients with T2DM. ECMH adherence to the annual eye exam increased significantly 1 year postintervention, compared to preintervention (73% vs 55%; P=.03) and 6 months (73% vs 46%, P=.01).
Conclusion: The metric with significant improvement during the chart audit, annual eye exam, is a process measure requiring advance planning. This small study suggests that a formal, regular audit process can improve student adherence to evidence-based care guidelines, particularly for tasks that require advance planning or action by the care team outside the day of a patient visit.
The Education-Centered Medical Home (ECMH) is a longitudinal clinical clerkship that emphasizes continuity and quality improvement via a consistent primary care experience throughout students’ medical education.1 Prior studies within a student-volunteer free clinic (SVFC) at CommunityHealth Chicago (CHC) demonstrated that ECMH provides patients comparable or higher rates of age-appropriate screening tests2,3 than the host clinic. Moreover, a targeted quality improvement intervention within ECMH increased HIV screening.3
This study aimed to evaluate our ECMH’s ability to improve type 2 diabetes mellitus (T2DM) care. Students and faculty established a chart audit and care planning process, aiming to increase knowledge of and attention to evidence-based T2DM care guidelines. Based on retrospective studies demonstrating quality improvement in T2DM care delivered by SVFCs to underserved patient populations4,5 as well as preliminary work6-8 we hypothesized that this would enhance longitudinal care provided to T2DM patients.
Throughout 14 months, medical students performed monthly chart audits on patients who had a diagnosis of T2DM, and who were seen in ECMH before and after the chart audit process was initiated. Each patient’s chart was audited by the same student or pair of students (initially 15 students). This study was determined by Northwestern University Feinberg School of Medicine’s Institutional Review Board to constitute quality improvement activity, not human subjects research (IRB #STU00203637).
Quality metrics were based on American Diabetes Association recommendations9: biannual lipid testing, annual microalbuminuria evaluation, ophthalmic and foot examinations, flu and pneumonia vaccination, statin therapy, hemoglobin A1c (HbA1c) level <8%, and systolic blood pressure (SBP) <140. HbA1c and SBP were considered “outcome metrics” because they refer to patient outcomes; all others were considered “process metrics” because they characterize an action taken by the clinical team. Eye exams require advance planning (referral about 2 months before the exam).
Students were educated on evidence supporting these quality metrics through a project summary. Chart audits consisted of reviewing prior notes, lab results, and medication lists to verify adherence to each quality metric. This process was established by faculty mentors and three student quality improvement chiefs, and shared with the group in written form at the outset of the project. Data were captured in a shared, deidentified spreadsheet accessible by ECMH students and faculty (not patients). Students developed personalized care plans for patients based on audit logs, including scheduling patient visits at least every 6 months, planning for tests at upcoming visits, and calling patients to follow up on medication adherence and care plans. After the first 6 months, we conducted a plan-do-study-act analysis10 and the process was streamlined to include phone calls as specified in the care plan, rather than monthly (appointment reminders and refill requests were not affected by the project). We obtained CHC adherence retrospectively through clinic records.
We aggregated quality metrics and data on demographics, body mass index (BMI), insulin use, and medication that were collected prior to project start (T=0, 2015), at 6 months (T=6, 2016), at project end (T=14, 2017), and 1 year after project end (T=14+12, 2018). Percentage adherence at different time points was compared with Fisher’s Exact test. We used linear regression modeling to assess the relationship between outcome measures and number of visits or audit logs. A 0.5% change in HbA1c was considered clinically meaningful.10,11
Eleven patients were in the ECMH cohort, with baseline characteristics shown in Table 1. Ten patients were interviewed through an interpreter. Eighty-one percent of audit logs were completed as planned (9-17 logs per patient) and 39 patient calls were made (at least one per patient). Patients averaged six visits between T=0 and T=14+12, every 6 months on average. ECMH adherence to annual eye exam increased significantly at T=14+12, compared to T=0 (73% vs 55%, P=.03) and T=6 (73% vs 46%, P= .01, Figure 1A). There were no other significant changes in ECMH adherence (Figure 1B-I; Table 2).
At T=14, the ECMH cohort had a mean HbA1c of 8.55% (5.9–10.6%), BMI 34.05 kg/m2 (23 – 36.3 kg/m2), and systolic blood pressure 127mmHg (110-140mmHg). Five patients had a clinically meaningful absolute decrease in HbA1c from T=0 and two had an increase. At T=14+12, the ECMH cohort had a mean HbA1c of 9.05% (5.5%–11.7%), BMI 28.8 kg/m2 (22.6 kg/m2–34 kg/m2), and systolic blood pressure 134mmHg (110-200 mmHg). Six patients had a clinically meaningful absolute decrease and three had an increase in HbA1c from T=0. There was no significant linear relationship between number of visits or number of logs and either HbA1c or SBP change.
This student-developed project succeeded in attaining increased ECMH adherence to diabetic eye exam in a complex patient population. This may have been because regular chart reviews helped students refer patients for eye exam appointments proactively. This aligns with previous work,3 where establishment of the ECMH clinic (without a targeted intervention) improved some performance metrics but did not improve screening rates for colon or breast cancer, both of which require advance planning. However, for most metrics there were no significant improvements, and students did not always complete assigned project tasks, possibly related to the effort involved.
This study has several important limitations. The patient cohort is a small and heterogeneous subgroup of patients with T2DM at CHC. Additionally, for foot exam, microalbuminuria, and low-density lipoprotein cholesterol screening, performance over 90% at baseline decreased the potential impact of the intervention. Finally, during the study period the CHC experienced some process changes, including flu vaccine and medication availability.
Nevertheless, this work suggests that a student-led quality performance chart review is feasible, and could be used to improve performance on quality measures requiring proactive steps by the care team prior to the patient’s appointment. Other SVFCs could apply this chart review approach to screening steps, such as FIT testing, mammography, low-dose CT and abdominal aortic imaging, that need to be initiated far in advance of being performed. Focusing effort on process measures that rely on advance planning is likely to maximize participation and impact.
Acknowledgments
The authors acknowledge the efforts of the CommunityHealth Clinic staff and prior members of the clinic, particularly Dr Olga Alexeeva, Dr William Gibb, Dr Jackson Herzog, Dr Abigail Russi, Dr Smitha Sarma, and Dr Andrea Baumgartner, who laid the foundation for the project described in this study.
Financial support: For the project reported in this study, author M.A. received funding support from Northwestern University (F30HL140910 and T32GM008152).
Presentations:
Content from this study was previously presented as follows:
- Aristova M, Alexeeva O, Gibb W, Herzog J, Russi A, Sarma S, Tschoe M, Baumgartner A. “A Student-Developed Longitudinal Project to Improve Diabetes Care”. Poster presentation at the Feinberg School of Medicine Lewis Landsberg Research Day, Chicago, IL. April 2018.
- Herzog J, Russi A, Sarma S, Tschoe M, Baumgartner A. “Impact of a Longitudinal Medical Student Education-Centered Medical Home on Quality Metrics.” Poster presentation at the Feinberg School of Medicine Lewis Landsberg Research Day, Chicago, IL. April 2017.
- Herzog J, Russi A, Sarma S, Tschoe M, Baumgartner A. “Impact of a Longitudinal Medical Student Education-Centered Medical Home on Quality Metrics.” Poster presentation at AAMC Integrating Quality Meeting, Rosemont, IL. June 2017.
References
- Henschen BL, Liss DT, Golden BP, et al. continuity with patients, preceptors, and peers improves primary care training: a randomized medical education trial. Acad Med. 2020;95(3):425-434. doi:10.1097/ACM.0000000000003045
- Mesa AS, Tschoe M. Comparison of quality metrics in an education-centered medical home with local and national benchmarks. Med Educ Online. 2022;27(1):2073806. doi:10.1080/10872981.2022.2073806
- Russi AE, Bhaumik S, Herzog JJ, Tschoe M, Baumgartner AC. Impact of an education-centered medical home on quality at a student-volunteer free clinic. Med Educ Online. 2018;23(1):1505401. doi:10.1080/10872981.2018.1505401
- Gorrindo P, Peltz A, Ladner TR. Medical students as health educators at a student-run free clinic. Acad Med. 2014. 89(4):625-631. doi:10.1097/ACM.0000000000000164
- Butala NM, Chang H, Horwitz LI, Bartlett M, Ellis P. Improving quality of preventive care at a student-run free clinic. PLoS One. 2013;8(11):e81441. doi:10.1371/journal.pone.0081441
- Herzog J, Russi A, Sarma S, Tschoe M, Baumgartner A. “Impact of a Longitudinal Medical Student Education-Centered Medical Home on Quality Metrics.” Poster presentation at the Feinberg School of Medicine Lewis Landsberg Research Day, Chicago, IL. April 2017.
- Herzog J, Russi A, Sarma S, Tschoe M, Baumgartner A. “Impact of a Longitudinal Medical Student Education-Centered Medical Home on Quality Metrics.” Poster presentation at AAMC Integrating Quality Meeting, Rosemont, IL. June 2017.
- Aristova M, Olga Alexeeva O, Gibb W, Herzog J, Russi A, Sarma S, Tschoe M, Baumgartner A. “A Student-Developed Longitudinal Project to Improve Diabetes Care”. Poster presentation at the Feinberg School of Medicine Lewis Landsberg Research Day, Chicago, IL. April 2018.
- American Diabetes Association Professional Practice Committee. Draznin B, Aroda VR, Bakris G, Benson G, Brown FM, Freeman R, Green J, Huang E, Isaacs D, Kahan S, Leon J, Lyons SK, Peters AL, Prahalad P, Reusch JEB, Young-Hyman D. 6. Glycemic targets: standards of medical care in diabetes-2022. Diabetes Care. 2022;45(suppl 1):S83-S96. doi:10.2337/dc22-S006
- Taylor MJ, McNicholas C, Nicolay C, Darzi A, Bell D, Reed JE. Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Qual Saf. 2014;23(4):290-298. doi:10.1136/bmjqs-2013-001862
- Little RR, Rohlfing CL. The long and winding road to optimal HbA1c measurement. Clin Chim Acta. 2013;418:63-71. doi:10.1016/j.cca.2012.12.026



There are no comments for this article.