Introduction: Point-of-care ultrasound (POCUS) is increasingly being employed in family medicine. Residency tracks can be an effective way to increase mastery in a specific subdiscipline for interested residents, but no studies exist on the implementation of a POCUS track in family medicine. We address this gap in the literature by assessing POCUS use by POCUS track residents compared to non-POCUS track residents and faculty in an academic family medicine department.
Methods: We performed a retrospective review of all POCUS scans completed in the first year after implementation of a family medicine residency POCUS track. Scans were analyzed by two reviewers. We compared scan volume and type between POCUS track residents, non-POCUS track residents, and faculty. A blinded quality analysis was performed on each group of scans.
Results: A total of 572 scans were completed on 536 patients over 1 year. POCUS track residents scanned significantly more than non-POCUS track residents (mean difference of 72.2, CI 59.1 to 85.4; P<.0001). The most common scan types across groups were musculoskeletal and soft tissue. POCUS track residents showed statistically improved scan quality in all scan types, while non-POCUS track residents showed statistical improvement only in soft tissue, shoulder, and abdominal aortic aneurysm scans.
Conclusions: This is the first longitudinal study of a novel academic family medicine residency POCUS track. Participation in a POCUS track can increase the number, variety, and quality of scans performed. Our curriculum can be a model for family medicine residency programs that wish to provide robust POCUS training.
Point-of-care ultrasound (POCUS), the bedside acquisition and interpretation of ultrasound images, has become a focus in family medicine training.1,2 In 2016, the American Academy of Family Physicians endorsed expansion of POCUS training, which spurred family medicine residencies (FMR) to expand POCUS training programs.2 The percentage of FMRs reporting an established POCUS curriculum grew from 2% in 2014 to 32% in 2021.3,4 In a 2021 survey, 81% of surveyed department chairs reported having at least one POCUS-trained faculty member.3,4 Training requirements also have shifted. Currently, the Accreditation Council for Graduate Medical Education’s Program Requirements for Graduate Medical Education in Family Medicine states, “Residents should have experience in using point-of-care ultrasound in clinical care.”5 Despite the rapid development of training programs, little published data exists on the impact of these training programs.
Prior studies describe POCUS training as workshops, rotations, or obstetrical uses; no data exists for POCUS tracks within FMRs.6-12 No data is available on the volume and types of scans performed in FMRs. This is important data both for determining training curriculum outcomes and for credentialing purposes, because credentialing typically depends on a specific number of scans performed.
The objective of this study was to describe the implementation and outcomes of a yearlong longitudinal POCUS track for family medicine residents at a single, large Midwestern academic medical center. We focused on scan types and scan volume performed by POCUS track versus non-POCUS track residents at two outpatient residency continuity clinics.
In 2021, three third-year family medicine residents participated in a yearlong inaugural residency POCUS track. This included seven POCUS simulation sessions (2-4 hours each); use of elective time to perform POCUS scans with a goal of 150 educational (ie, nonbillable) patient scans per track resident; and approximately 130 hours performing educational scans. Non-POCUS track residents received monthly didactics along with POCUS track residents and had equal opportunity to perform educational scans in the clinic. Non-POCUS track residents participated in quarterly hour-long ultrasound didactics and biannual simulation center sessions (8 hours).
Educational scans were performed at outpatient family medicine clinics using Mindray TE7 or GE Logiq ultrasounds. The scans were stored on middleware software called Qpath. The ultrasound fellowship-trained faculty member performed a quality review on all images to provide learners feedback.
An institutional review board exempted our retrospective review of all scans from July 1, 2021, through June 30, 2022, which was performed independently by two reviewers. Scan type was determined by a combination of image or video annotation, if available, and independent reviewer image interpretation. Consensus on scan type was reached. Scan performers were categorized as POCUS track resident, non-POCUS track resident, faculty, or unknown. One faculty member had completed a sports medicine fellowship, but otherwise all other faculty were learners themselves. Scans from the ultrasound fellowship-trained faculty member were excluded from analysis. Scans were included for review if a minimum of one image or video clip was available for interpretation. We compared the number of scans performed by POCUS track and non-POCUS track residents using Microsoft Excel to complete unpaired t tests and compute difference of means.
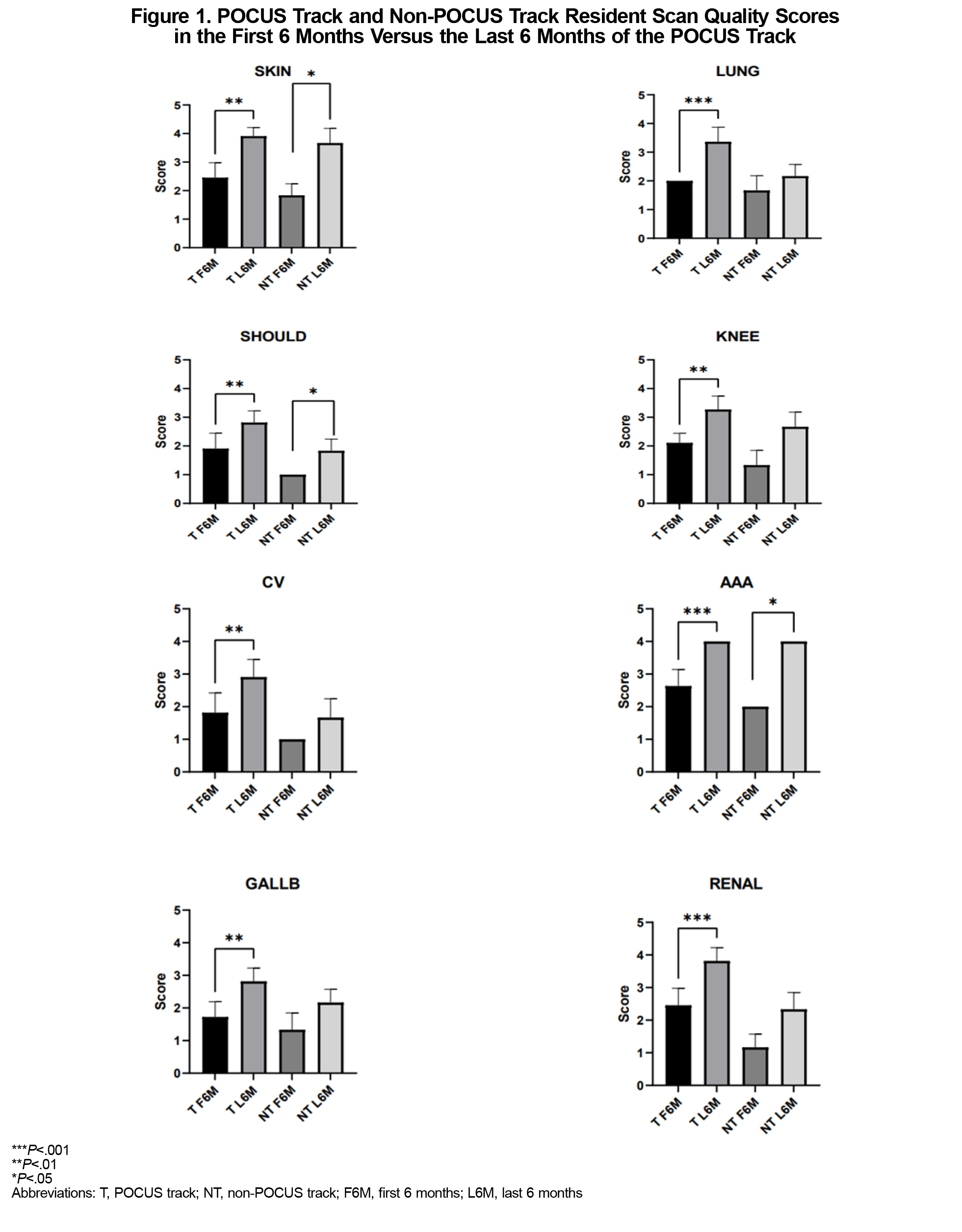
Quality guidelines were established for each scan type, and a retrospective scan quality analysis was performed by two blinded reviewers.13 Scan quality in the first 6 months was compared to the last 6 months for both POCUS track and non-POCUS track residents. Quality review was nonparametric, so a Mann-Whitney analysis was used.
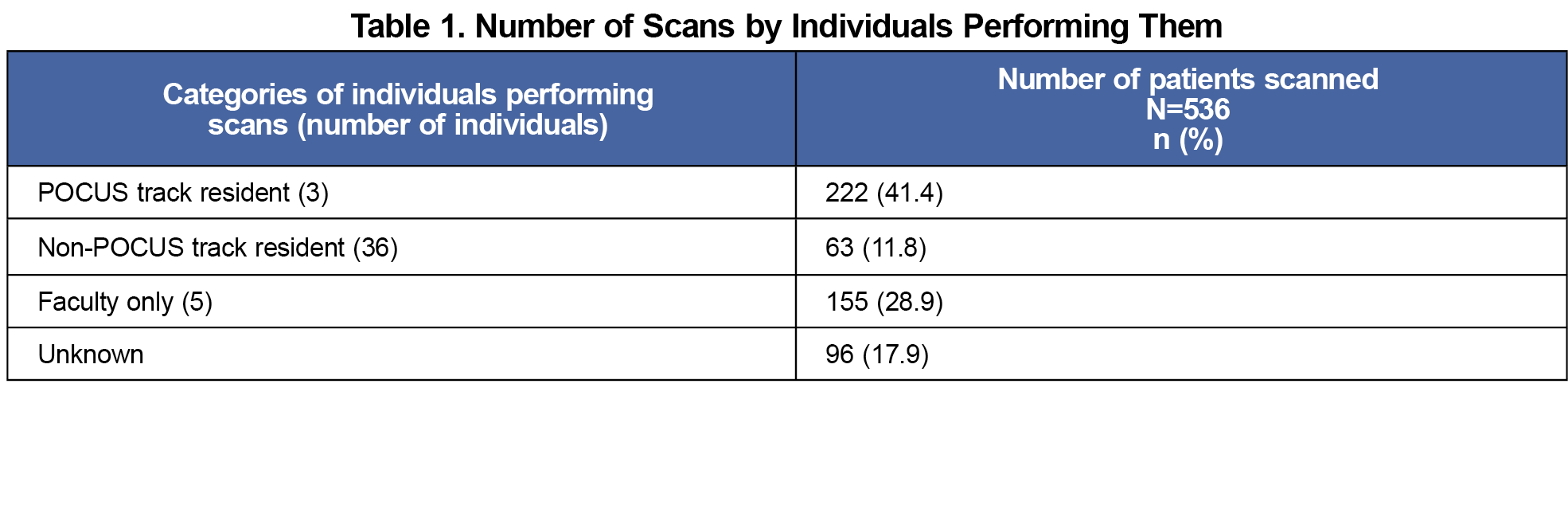
A total of 536 patients received POCUS scans from July 2021 through June 2022 (Table 1). POCUS track residents performed 239 scans on 222 patients (some patients had multiple scan types completed in the same scanning encounter). Non-POCUS track residents (n=36) performed 69 scans on 63 patients.
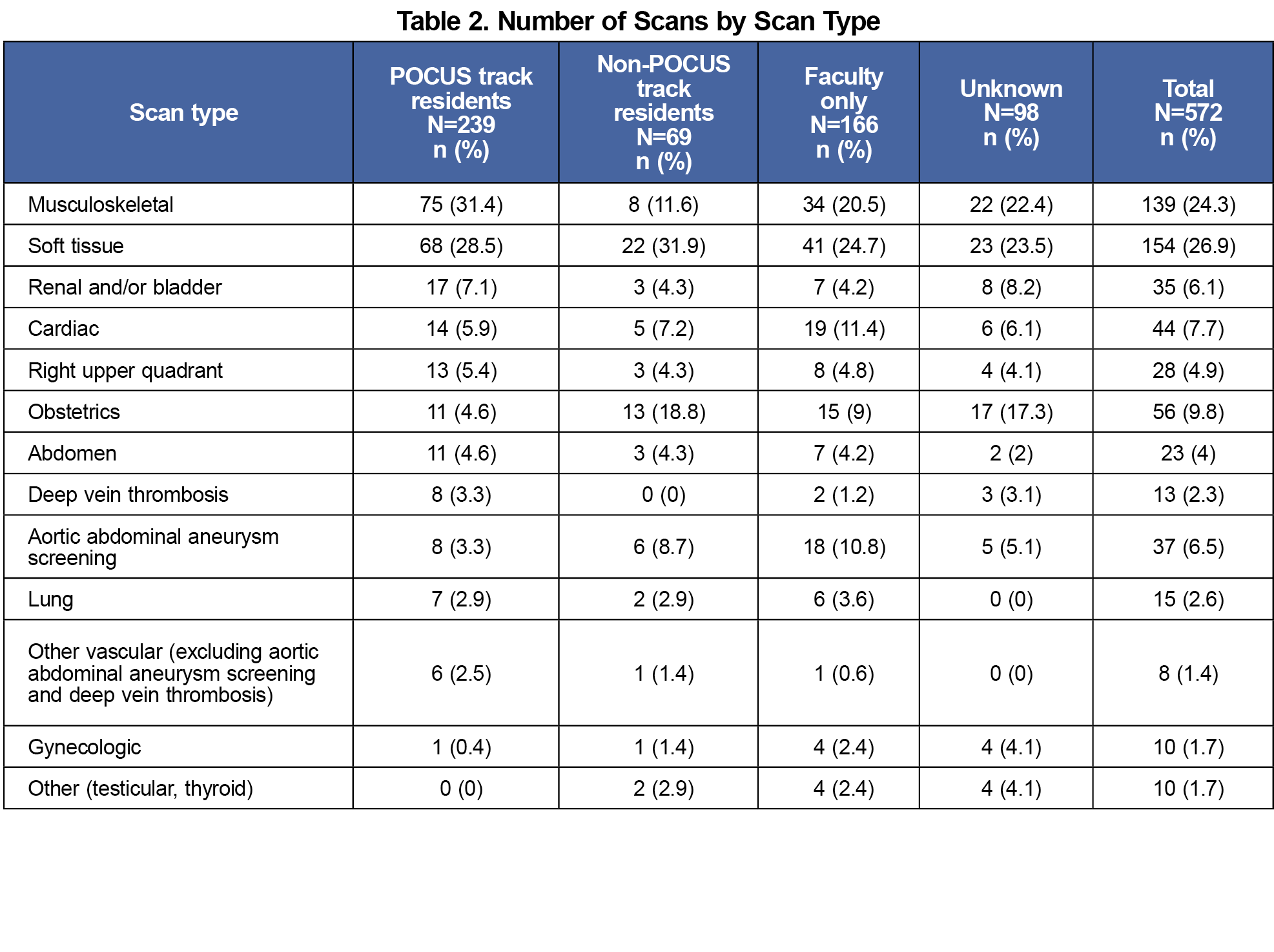
The most common scans for POCUS track residents were musculoskeletal (31.4%), soft tissue (28.5%), and renal (7.1%; Table 2). The most common scans for non-POCUS track residents were soft tissue (31.9%), obstetrics (18.8%), and musculoskeletal (11.6%).
The POCUS track residents scanned more patients than their non-POCUS track peers (222 vs 63). We identified a significant difference between the mean number of patients scanned on average by the POCUS track residents compared to non-POCUS track residents (mean difference of 72.2, CI 59.1 to 85.4; P<.0001). In total, 41.4% of all scans during the track year were performed by the POCUS track residents. Non-POCUS track residents performed 11.8% of scans.
A randomized, blinded quality review showed overall improvement in scan quality in all scan types when comparing both time periods. A Mann-Whitney test comparing quality between time periods showed improvements in all scan types for POCUS track residents, but significant statistical improvement in only soft tissue (P=.0022), shoulder (P=.152), and abdominal aortic aneurysm (P=.0022) scans for non-POCUS track residents (Figure 1).
To our knowledge, this is the first study describing a longitudinal POCUS track in a family medicine residency. Our data shows that POCUS track residents obtained both larger scan volume and improved scan quality compared to their non-POCUS track peers. All POCUS track residents fell short of the goal of 150 patient scans each. The barriers involved with implementing a novel program include use of new technology, comfort performing educational scans, and patient hesitancy.
This study had limitations. The scan performer could not be identified in 96 scans; although we suspect the majority were performed by POCUS track residents, we cannot be sure. This failure likely reflects the common challenges regarding novel technology implementation faced by programs establishing POCUS curricula. Improved workflow between ultrasound machine, electronic health record, and middleware should lead to improved scan documentation in our program. Quality analysis was based on retrospectively selected criteria, no universally agreed upon analysis criteria exists.
Residents participating in a POCUS track performed significantly more scans than their non-POCUS track peers. POCUS track residents’ scan quality improved most with implementation of our program. A POCUS track is a useful strategy for promoting POCUS utilization in FMRs and preparing graduates for a future in primary care that is likely to make POCUS a central aspect of its practice. Further studies should focus on FMR POCUS track learning outcomes and addressing barriers to POCUS use in family medicine.
Acknowledgments
Presentation: This study was presented in poster format with preliminary data at the North American Primary Care Research Group 50th Annual Meeting, November 18–22, 2022, Phoenix, Arizona.
References
- American College of Emergency Physicians. Ultrasound guidelines: emergency, point-of-care and clinical ultrasound guidelines in medicine. Ann Emerg Med. 2017;69(5):e27-e54. doi:10.1016/j.annemergmed.2016.08.457
- American Academy of Family Physicians. Resolution no. 602 (New York E): increase point of care ultrasound (POCUS) education in family medicine. 2016.https://www.aafp.org/about/governance/congress-delegates/2016/resolutions/newyork-e.mem.html.
- Capizzano JN, O’Dwyer MC, Furst W, et al. Current state of point-of-care ultrasound use within family medicine. J Am Board Fam Med. 2022;35(4):809-813. doi:10.3122/jabfm.2022.04.220019
- Hall JWW, Holman H, Barreto TW, et al. Point-of-care ultrasound in family medicine residencies 5-year update: a CERA study. Fam Med. 2020;52(7):505-511. doi:10.22454/FamMed.2020.223648
- Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Family Medicine. 2023. https://www.acgme.org/globalassets/pfassets/programrequirements/120_familymedicine_2023.pdf
- Bornemann P. Assessment of a novel point-of-care ultrasound curriculum’s effect on competency measures in family medicine graduate medical education. J Ultrasound Med. 2017;36(6):1,205-1,211. doi:10.7863/ultra.16.05002
- Wong F, Franco Z, Phelan MB, Lam C, David A. Development of a pilot family medicine hand-carried ultrasound course. WMJ. 2013;112(6):257-261.
- Dresang LT, Rodney WM, Dees J. Teaching prenatal ultrasound to family medicine residents. Fam Med. 2004;36(2):98-107. https://www.stfm.org/familymedicine/vol36issue2/Dresang98
- Smith CB, Sakornbut EL, Dickinson LC, Bullock GL. Quantification of training in obstetrical ultrasound: a study of family practice residents. J Clin Ultrasound. 1991;19(8):479-483. doi:10.1002/jcu.1870190805
- Hahn RG, Roi LD, Ornstein SM, et al. Obstetric ultrasound training for family physicians. results from a multi-site study. J Fam Pract. 1988;26(5):553-558.
- Sorensen B, Hunskaar S. Point-of-care ultrasound in primary care: a systematic review of generalist performed point-of-care ultrasound in unselected populations. Ultrasound J. 2019;11(1):31. doi:10.1186/s13089-019-0145-4
- Andersen CA, Holden S, Vela J, Rathleff MS, Jensen MB. Point-of-care ultrasound in general practice: a systematic review. Ann Fam Med. 2019;17(1):61-69. doi:10.1370/afm.2330
- Beduhn B, Capizzano N. Quality Guidelines for First Year POCUS. STFM Resource Library. https://resourcelibrary.stfm.org



There are no comments for this article.