Introduction: Food insecurity (FI) is defined as a lack of access to enough food for an active, healthy life. We sought to determine how a longitudinal FI screening curriculum impacts medical students’ knowledge, attitudes, and behavior in screening for FI.
Methods: This was a prospective, single-institution study. The curriculum consisted of three components completed over 3 years. We administered a survey to the intervention cohort before and after the curriculum and analyzed their written reflections. We also evaluated whether students screened for FI during an objective structured clinical exam (OSCE) and compared their performance to a control cohort, which did not receive the curriculum.
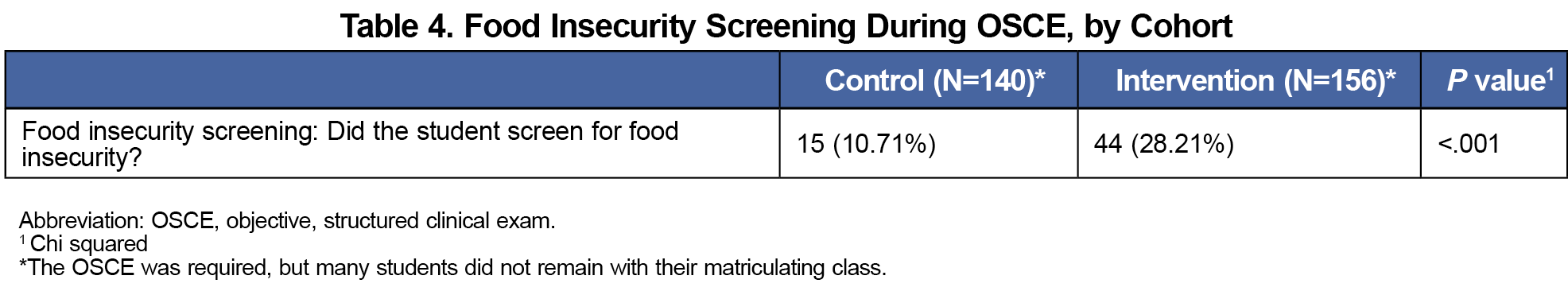
Results: Preintervention, students felt screening for FI was important for physicians to do with their patients, but most felt uncomfortable addressing it in clinical settings. Postintervention, there was a statistically significant increase in mean scores for knowledge questions (45.24% vs 74.74%, P<.001, pre- and postintervention, respectively). Students also felt more confident in their abilities to screen and follow up about FI. Additionally, compared to the control cohort, the intervention cohort screened for FI more often during their OSCE (28.21% vs 10.71%, P<.001).
Conclusion: A longitudinal curriculum using minimal curricular time can improve students’ knowledge, attitudes, and behavior when screening for FI. Students who received the curriculum were more likely to recognize the need for and perform FI screening. Based on these findings, we anticipate that the curriculum will increase the likelihood of students identifying, screening for, and intervening in cases of FI in future clinical encounters.
In 2021, 13.5 million US households (10.2%) were food insecure.1 Food insecurity (FI) is defined as a lack of access to enough food for an active, healthy life.2 The social and structural determinants of health (SDOH), including FI, are major contributors to chronic illnesses in the United States.3 FI is also associated with higher health care utilization, higher health care costs, and adverse health outcomes, especially for children.4–6
There is a growing interest in training health professionals to screen for the SDOH, including FI.7 The American Academy of Pediatrics recommends universal screening for FI8; other organizations plan to consider modifiable SDOH9 in their recommended screenings. Yet, most medical schools do not have an FI screening curriculum; existing programs are primarily for residents and attending physicians.10–12 Given the high prevalence of FI in Washington, DC13 where our medical students train, we designed a longitudinal curriculum to address this gap.
The curriculum is a novel attempt to explicitly teach FI screening to medical students. Our study objective was to determine whether participation in this FI screening curriculum improves students’ knowledge, self-efficacy, and behavior in screening for and intervening in cases of FI.
Design and Setting
This was a prospective, single-institution study at a midsized, private medical school in the US mid-Atlantic region. Participants included students from the classes of 2022 (intervention cohort) and 2021 (control cohort).
Educational Intervention
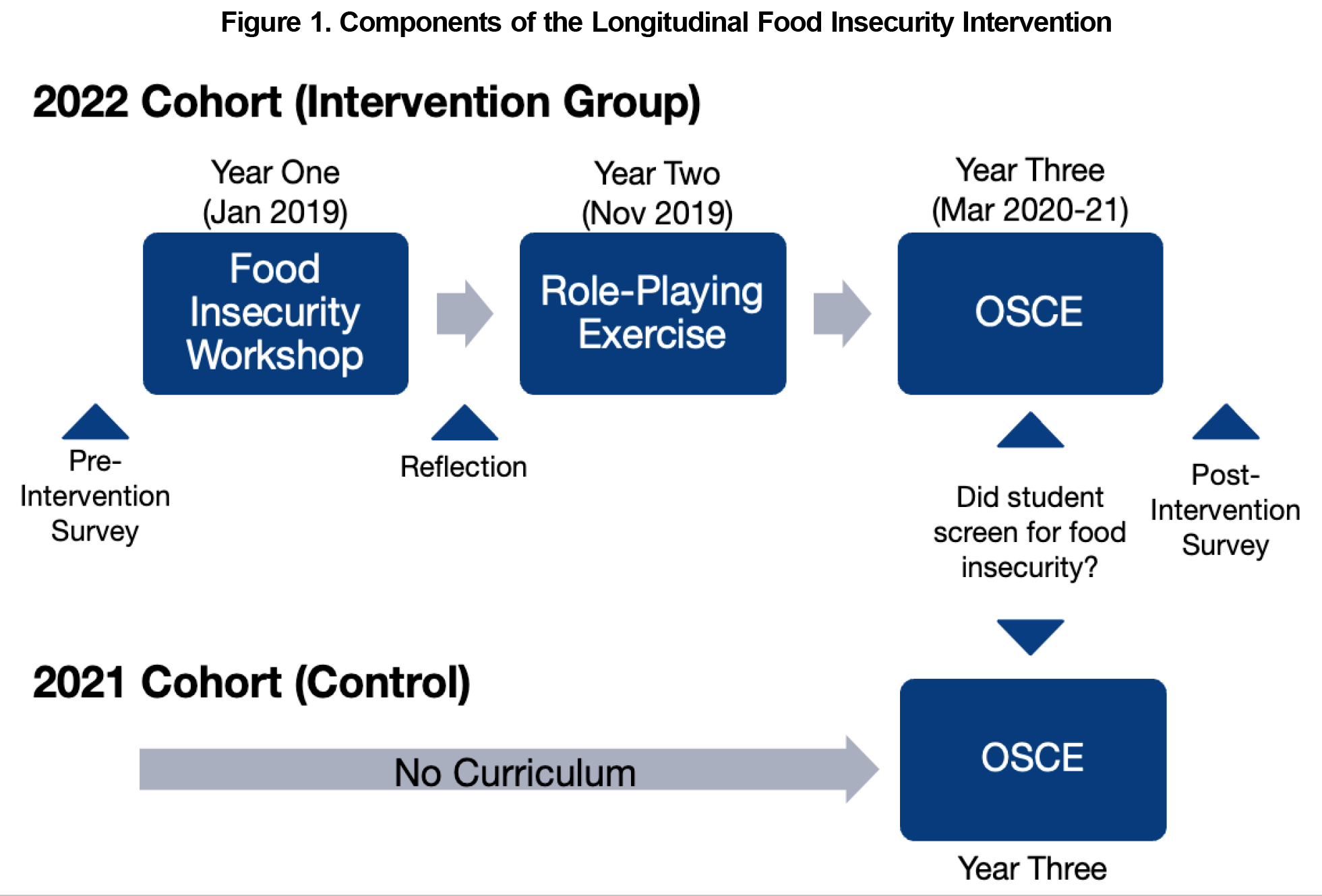
The longitudinal FI curriculum (“curriculum”) was introduced during the first year of medical school. It included three components completed over 3 years (Figure 1).
Year 1. We presented information on FI screening during a 2-hour workshop and distributed the Food Insecurity Screening Informational Pocket Card. Students were then paired to practice screening, using scenarios based on real clinical encounters. The 10-item Qualtrics survey and the Pocket Card can be found in the STFM Resource Library.14
Year 2. The curriculum was reinforced with a similar 20-minute FI screening role-playing exercise.
Year 3. Students participated in an existing objective structured clinical exam (OSCE) with a patient with poorly-controlled diabetes. The patient had recently struggled with FI but did not present with specific complaints of FI.
Procedures and Measures
During Year 1, students were emailed an informed consent script to participate in the study. We then administered a 10-item survey via Qualtrics. In Year 3, students completed the same survey, postintervention.
Five items assessed students’ FI knowledge using multiple-choice questions and were scored as correct or incorrect. Five items also assessed students’ attitudes using a 5-point Likert scale (1=strongly disagree to 5=strongly agree); we calculated the percentage of respondents who agreed or strongly agreed.
Furthermore, intervention students submitted written reflections on the following prompts after the workshop:
- What went well?
- What was challenging?
- What questions or insights did this exercise raise for you?
Both the intervention cohort and a historical control cohort completed the OSCE, which remained unchanged between years. The historical control group had not participated in the FI curriculum. Standardized patients scored “yes” or “no” on one OSCE checklist item, “Did the student screen for FI?”
Data Analysis
We calculated descriptive statistics for intervention students’ pre- and postintervention survey responses. Categorical variables were reported as count and frequency; continuous data were reported as mean and standard deviation. We used Wilcoxon Signed-Rank and McNemar tests to compare the paired pre- and postdata. We did not perform multiple testing corrections. We performed comparison of successful OSCE screening between intervention and control groups using the χ2 test. Incomplete data in pre/post knowledge questions with at least one answer were considered incorrect. If none were answered, it was considered missing data and was excluded from analysis. Significance was defined as P<.05. SAS v9.4 was used for all analyses.
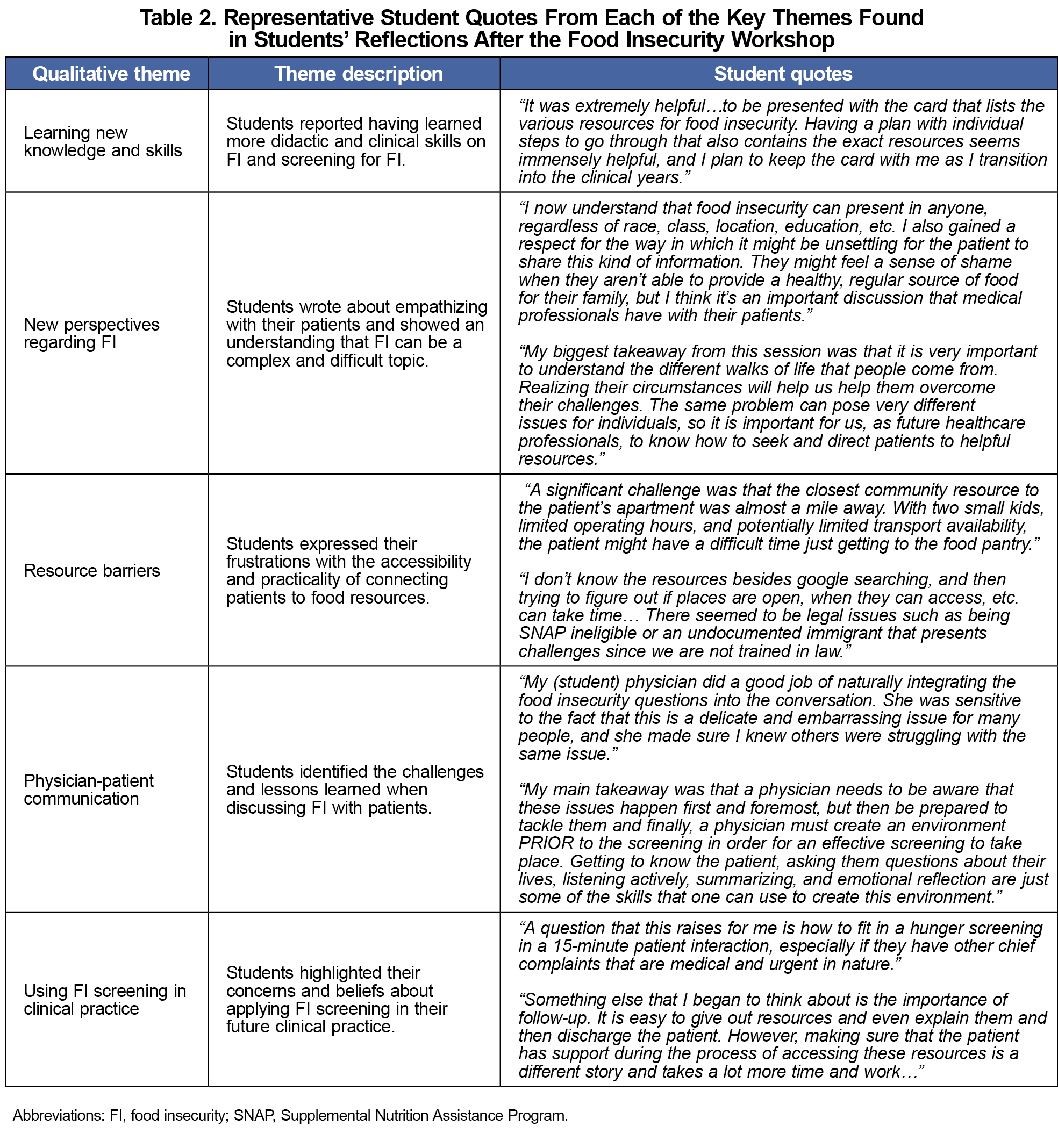
We qualitatively analyzed postworkshop reflections to determine predominant themes. Two researchers not involved in the intervention independently completed the data coding and analysis using the software data management program, Ethnograph v6 (Qualis Research, Colorado Springs, CO). They developed a coding dictionary based on the reflection questions asked as part of the assessment in the FI workshop in year 1 and identified emerging themes through review of the data. After independently coding the data, the coded text was extracted to populate an analysis grid to support and finalize themes.
This study (#20181123) was determined to be exempt from review by our institutional review board.
Of the 204 students who received the intervention, 61 (30.0%) completed both pre- and postintervention surveys, and 137 (67.5%) submitted reflections. Four observations were missing for the postsurvey knowledge questions and seven were missing for postsurvey attitude questions. The OSCE was completed by 156 and 140 students in the intervention, and control cohorts, respectively.
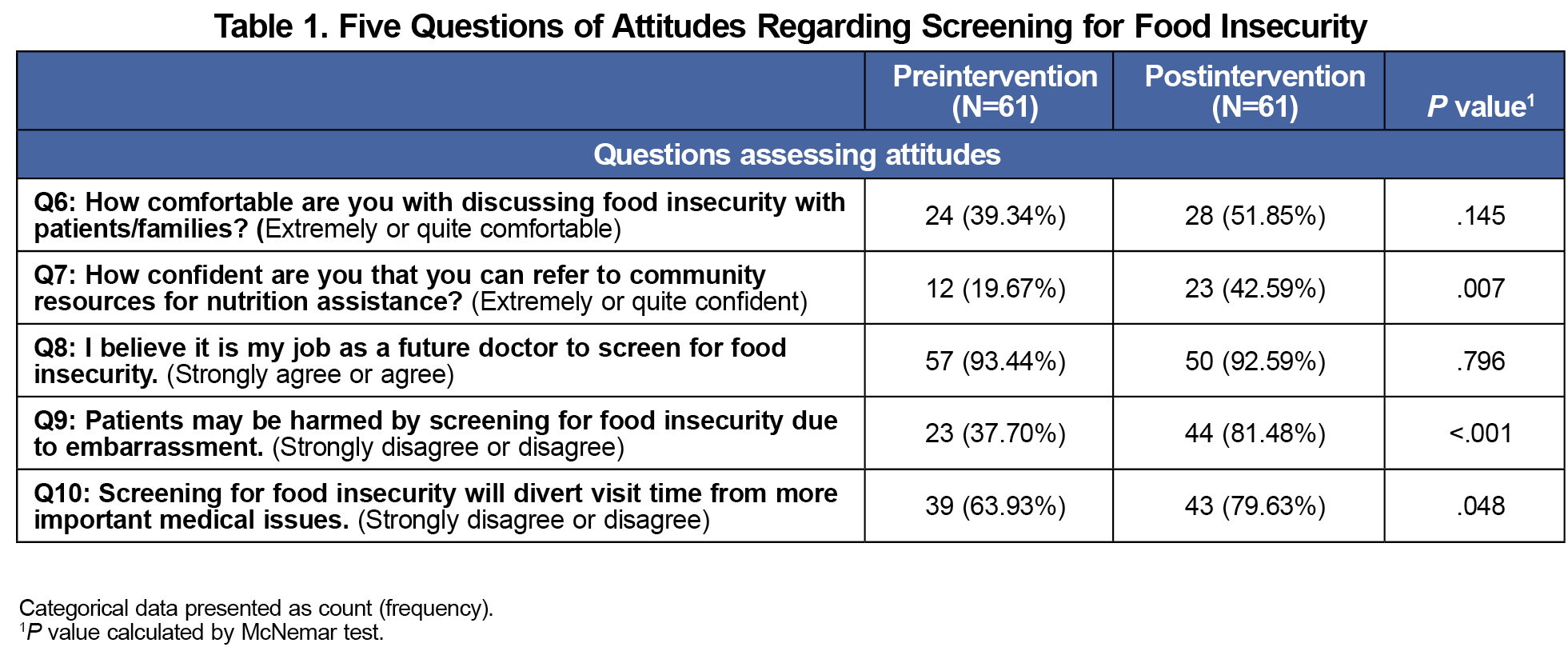
When considering preintervention attitudes, only 24 (39.34%) students agreed/strongly agreed that they were comfortable discussing FI with patients; even fewer (12, 19.67%) agreed/strongly agreed they were confident referring to community resources. However, 57 (93.44%) students agreed/strongly agreed that screening for FI was important for physicians to do with their patients. Some students (23, 37.70%) disagreed/strongly disagreed that their patients would be harmed by screening due to embarrassment and 39 (63.93%) students disagreed/strongly disagreed their screening will divert visit time from more important medical issues (Table 1).
In terms of outcomes, students were significantly more likely to feel extremely or quite confident in referring patients to community resources for nutrition assistance at postintervention compared to preintervention (19.67% vs 42.59%, respectively). They were also significantly more likely to strongly disagree or disagree to “patients may be harmed by screening for food insecurity due to embarrassment” (37.70% vs 81.48%) and “screening for food insecurity will divert visit time from more important medical issues” (63.93% vs 79.63%; Table 1).
Qualitative results were determined based on students' reflections after the workshop. Five salient themes supported students’ preintervention attitudes:
- Learning New Knowledge and Skills
- New Perspectives Regarding FI
- Resource Barriers
- Physician-Patient Communication
- Using FI Screening in Clinical Practice.
Explanation of the themes and representative quotes are shown in Table 2.
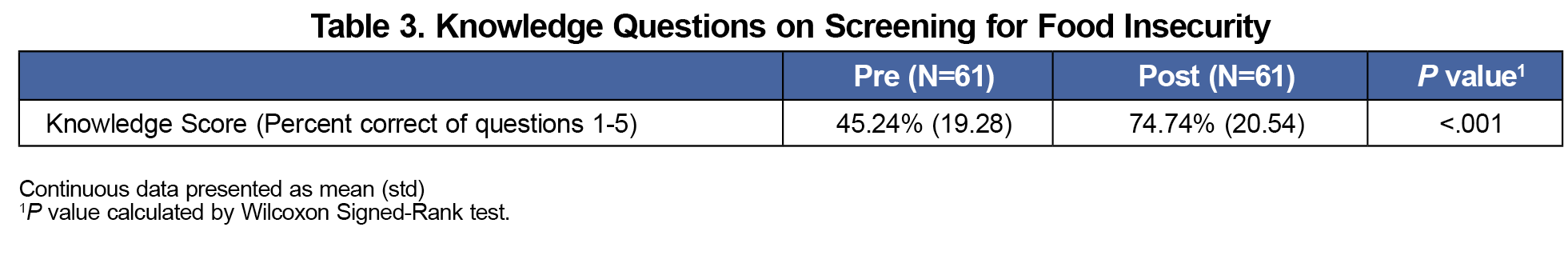
Regarding knowledge questions, students showed a statistically significant increase in mean percent scores pre- and postintervention (45.24% vs 74.74%, P<.001; Table 3). In their behaviors, students in the intervention cohort were significantly more likely than the control cohort to screen for FI (28.2% vs 10.7%, P<0.001; Table 4).
Our curriculum added less than 3 hours of curricular time and improved students’ knowledge. Moreover, students who participated in the curriculum were more likely than students who had not participated to both recognize the need and screen for FI. This is particularly significant as the standardized patient did not present with specific complaints of FI, so students were not explicitly prompted.
Our study was limited to one intervention cohort at one institution. The number of students who completed both the pre-and postintervention surveys was low. Student behavior was assessed using simulated patients in one case. The results may therefore not be generalizable across different student populations within or outside our institution, in other health profession educational settings, or in practice.
A longitudinal curriculum can improve students’ knowledge, self-efficacy, and behavior in screening for FI. Reinforcing knowledge and skills for behavior change may require minimal additional curricular time if integrated into the existing curriculum.
Acknowledgments
The authors thank Jack Penner, MD, and Richard Waldhorn, MD, who coauthored the curricular grant; Riva Desai, MD, Yadhu Dhital, MD; Stephen Kane, MD; Sahaj Patel, MD; Derrick Arthur-Cudjoe; and Margaret Eshleman, MEd, for curricular development and support; and the Georgetown University School of Medicine Class of 2022 for their participation in this curriculum and study.
Financial support: This curriculum was supported by a grant for curricular innovation from the Georgetown University School of Medicine.
Presentations: “Screening for, and Intervening in, Food Insecurity: A Curriculum for Health Professionals”; presented at the Association for Prevention Teaching and Research (APTR)’s Annual Conference on March 29, 2022.
References
- Coleman-Jensen A, Rabbitt M, Gregory C, Singh A. Household Food Security in the United States in 2021.Economic Research Service; 2022.
- Food Security in the U.S. United States Department of Agriculture Economic Research Service. Accessed March 16, 2023. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-u-s/
- Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010;140(2):304-310. doi:10.3945/jn.109.112573
- Gundersen C, Ziliak JP. Food insecurity and health outcomes. Health Aff (Millwood). 2015;34(11):1830-1839. doi:10.1377/hlthaff.2015.0645
- Berkowitz SA, Basu S, Gundersen C, Seligman HK. State-level and county-level estimates of health care costs associated with food insecurity. Prev Chronic Dis. 2019;16:E90. doi:10.5888/pcd16.180549
- Thomas MMC, Miller DP, Morrissey TW. Food insecurity and child health. Pediatrics. 2019;144(4):e20190397. doi:10.1542/peds.2019-0397
- Doobay-Persaud A, Adler MD, Bartell TR, et al. Teaching the social determinants of health in undergraduate medical education: a scoping review. J Gen Intern Med. 2019;34(5):720-730. doi:10.1007/s11606-019-04876-0
- Gitterman BA, Chilton LA, Cotton WH, et al. Promoting food security for all children. Pediatrics. 2015;136(5):e1431-e1438. doi:10.1542/peds.2015-3301
- Davidson KW, Kemper AR, Doubeni CA, et al. developing primary care-based recommendations for social determinants of health: methods of the u.s. preventive services task force. Ann Intern Med. 2020;173(6):461-467. doi:10.7326/M20-0730
- Smith S, Malinak D, Chang J, Schultz A, Brownell K. Addressing food insecurity in family medicine and medical education. Fam Med. 2017;49(10):765-771.
- Stenmark SH, Steiner JF, Marpadga S, Debor M, Underhill K, Seligman H. lessons learned from implementation of the food insecurity screening and referral program at kaiser permanente colorado. Perm J. 2018;22(4S):18-093. doi:10.7812/TPP/18-093
- Ghouse A, Gunther W, Sebastian M. Evaluation of a COVID-influenced curriculum to address food insecurity in a detroit family medicine residency clinic. Spartan Med Res J. 2020;5(2):17649. doi:10.51894/001c.17649
- DC Food Policy Council. The Road Ahead.Update on Food Access & Food Security in the District of Columbia; 2021.
- Shitama Jarris Y, Chang H, Kureshi S, et al. Longitudinal Food Insecurity Screening Curriculum for Medical Students. STFM Resource Library. Accessed February 6, 2024. https://resourcelibrary.stfm.org/viewdocument/longitudinal-food-insecurity-screen?CommunityKey=2751b51d-483f-45e2-81de-4faced0a290a&tab=librarydocuments



There are no comments for this article.