Background and Objectives: Program director (PD) tenure, continuity, and stability may enhance residency program quality, yet many PDs do not stay long in their positions. No prior study has taken a comprehensive census of departing PDs to determine reasons for leaving the role. This study aimed to survey all exiting family medicine (FM) PDs to identify decision factors contributing to their departure.
Methods: From October 2021 to October 2022, we sent a web-based exit survey to all departing FM PDs. The survey asked departing PDs to rate the strength of 36 factors in the decision to exit the PD role in terms of job satisfaction, accomplishments, career choices, workload, preparation, expectations, and support. We used the Fisher exact test to assess all 36 decision factors and PD characteristics for significant associations with shorter or longer PD tenures.
Results: PDs submitted 73 surveys out of 109 invitations (67.0% response). We analyzed 68 with complete data. The median PD tenure was 5.6 years (mean 6.9 years). Most respondents (66/68, 97.1%) identified three or more strong factors in their decision to leave. The strongest factors reflected stable residency programs, an established succession plan, a desire for more personal/family time, and a sense that the time was right. PDs with tenures longer than 3 years were more likely to have completed the National Institute for Program Director Development (P=.001).
Conclusions: PDs leave the position for multiple reasons, often positive, and not necessarily due to lack of support and preparation. Further exploration of decision factors may inform strategies to support PDs in their positions.
Program director (PD) tenure, continuity, and stability may enhance residency program quality.1-4 Mastering the complexities of residency education takes time and institutional support,4 yet many PDs do not stay long in their positions.5-7 Family medicine (FM) and internal medicine studies have found that PDs report stressors from administrative duties, clinical load, family obligations, teaching responsibilities, and research demands, but the role of burnout in PD tenure is unclear.8-11 Specific factors related to PD tenure are not well-known. Importantly, PDs indicate positives that contribute to retention.12-15
Initial qualitative research findings indicate that family medicine PDs leave due to combinations of factors, most often out of a desire to pursue new career opportunities rather than dissatisfaction with the PD job.16 Continuous program development, strong internal and external support, and rewards of the position help sustain PDs in the role.14 No prior study has taken a comprehensive census of departing PDs to determine their reason for leaving the role. As a follow-up to our prior qualitative study,16 we surveyed all exiting FM PDs to identify (a) important decision factors contributing to their departure, and (b) factors associated with PD tenure length.
To all departing FM PDs, we sent a rolling exit survey with questions based on prior studies by the Association of Family Medicine Residency Directors (AFMRD)/American Academy of Family Physicians (AAFP) National Research Network14 and the Association of Program Directors of Internal Medicine.10,17,18 The survey was piloted with former PDs, resulting in a 51-item survey that included 36 statements rating the strength of each factor in the decision to exit the PD role (using a 5-point, Likert-type scale). Decision factors included statements about workload, program successes and supports, preparation for the role, and how PDs would like to spend their time. The full list of decision factor statements is available in the STFM Resource Library.19 The AAFP Institutional Review Board approved this study.
From September 2021 to September 2022, AFMRD staff assembled lists of departing PDs. Departing PDs were emailed a survey link to an online survey in REDCap (Research Electronic Data Capture).20, 21 Up to three follow-up emails to nonresponders were sent 1 week apart. Anonymous surveys were completed between October 2021 and October 2022.
We used basic descriptive statistics to describe the respondent sample. We used the Fisher exact test to assess all 36 decision factors and PD characteristics for significant associations with shorter or longer PD tenures.
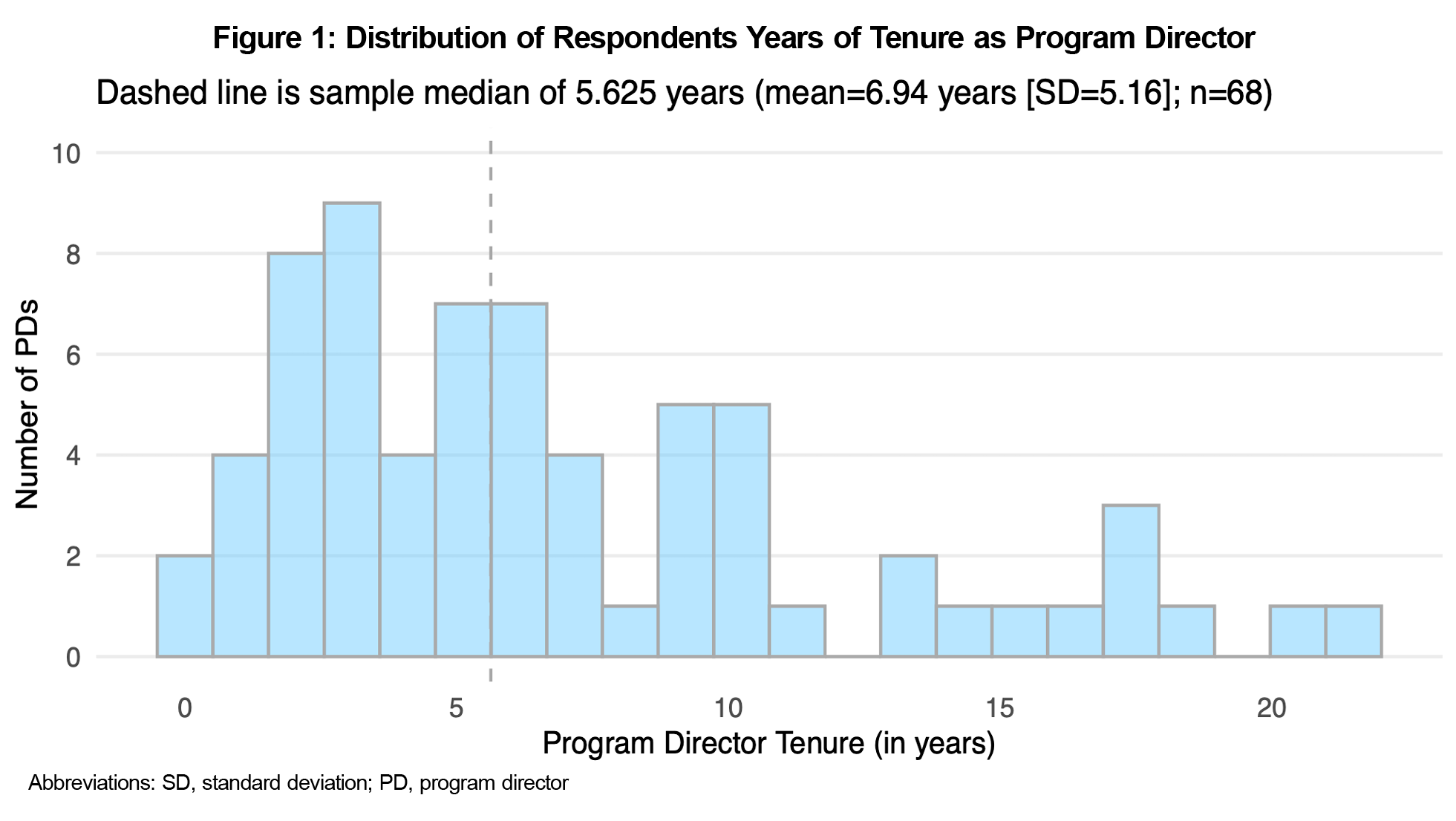
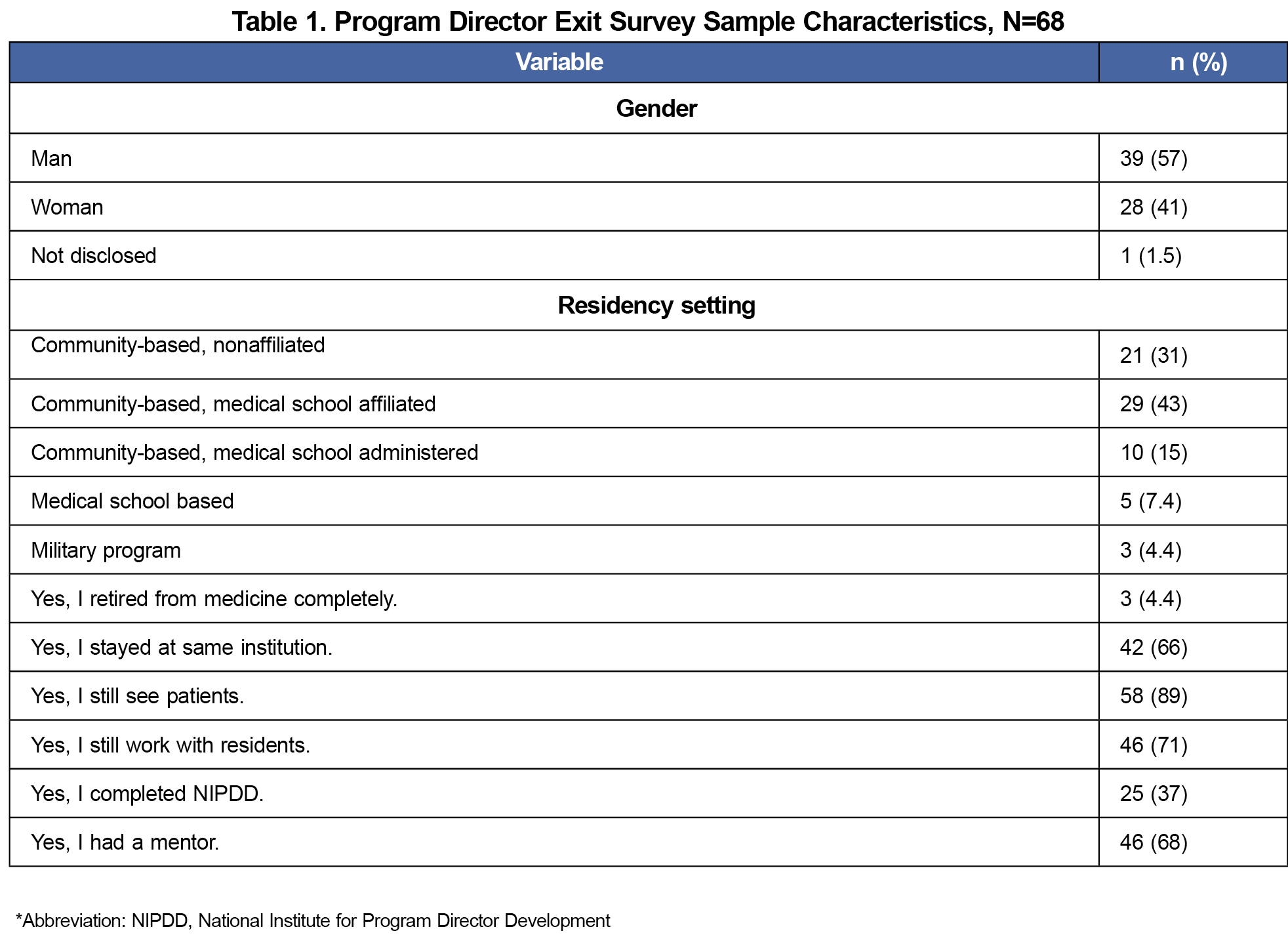
After removing duplicate and invalid email addresses, 109 unique invitations were sent. Seventy-three (73/109) surveys were submitted (67.0%). Removing five incomplete surveys yielded a final response rate of 62.3% (68/109). Respondent characteristics are shown in Figure 1 and Table 1.
Factors in Decisions to Leave
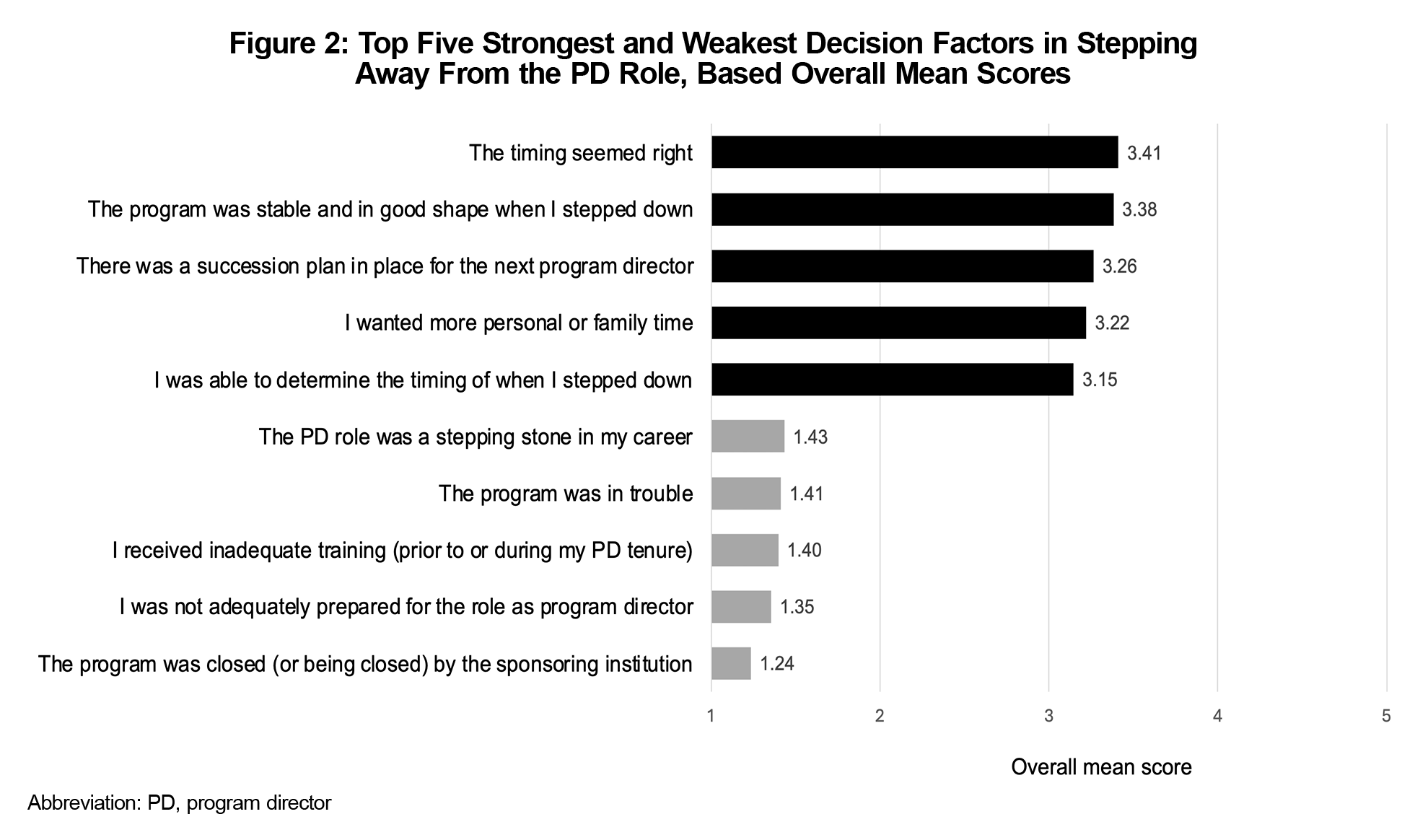
Almost all respondents (66/68, 97.1%) identified three or more strong or very strong factors in their decision to leave. We computed the mean score for each decision factor using all available responses for each item. Six items were missing just one response (missing completely at random) with no other missing decision factor data. The strongest factors reflected stable residency programs, an established succession plan, a desire for more personal/family time, and a sense that the time was right (Figure 2). The weakest factors—those with fewest strong or very strong factor ratings—related to programs that were in trouble or closed, or PDs who felt inadequately trained or unprepared for the role.
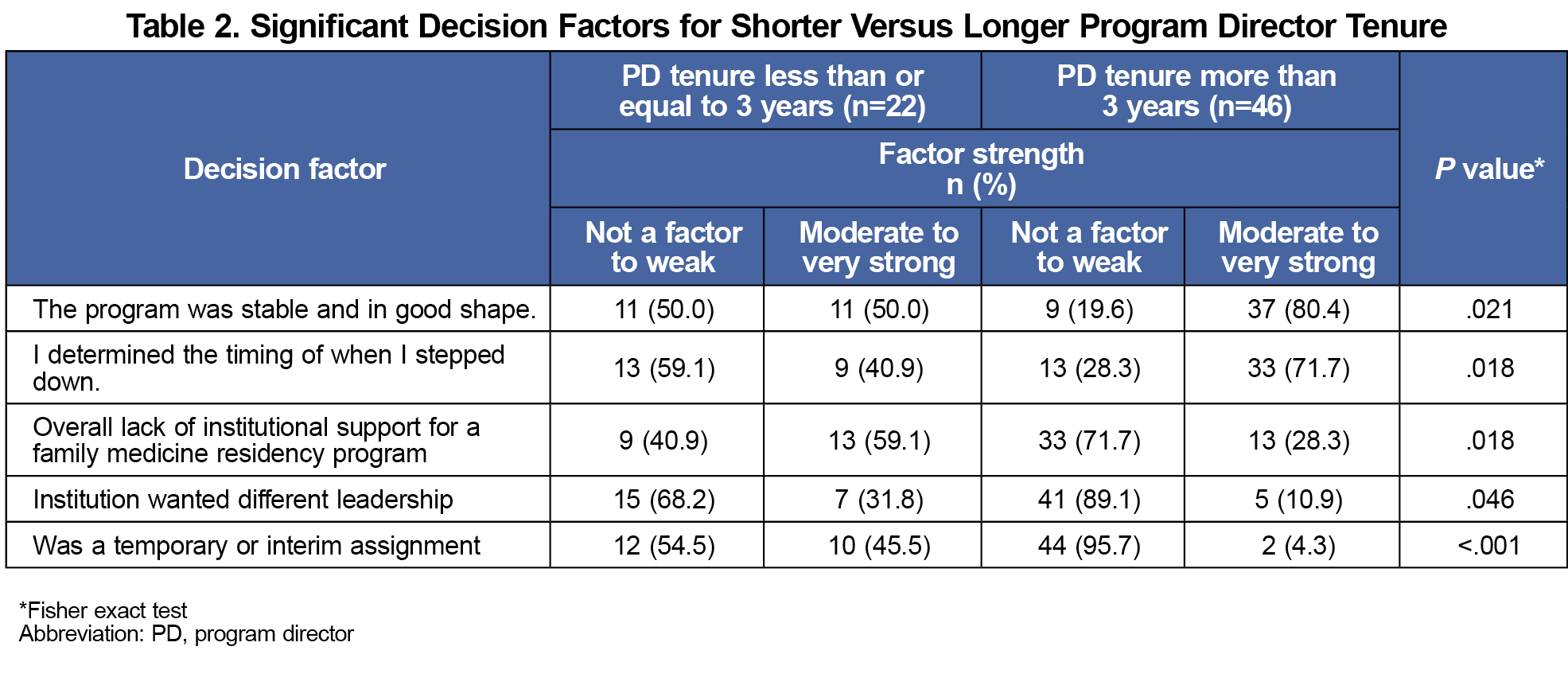
Our prior qualitative study did not include any PDs who departed within 3 years.16 The current survey data allowed examination of shorter tenures. PD tenure was recoded into two categories of less than or equal to 3 years versus greater than 3 years. We used the Fisher exact test to compare each decision factor (collapsed into two categories—moderate/strong/very strong factor vs weak/not a factor) by PD tenure. Just five factors differed significantly by tenure category (Table 2). Additionally, PDs with tenures longer than 3 years were more likely to have completed the National Institute for Program Director Development (NIPDD; P=.001). Gender (P=.298) or having a mentor (P=.591) were not significantly associated with tenure length.
With a larger sample of respondents, these results confirm previous qualitative research findings: PDs step away for multiple reasons; departure decisions often include positive reasons (eg, stable programs, succession plans); and decisions are not due only to lack of support or administrative burden.16 Most respondents (64/68; 94%) indicated that lacking preparedness or training were not strong factors in their decision. Despite a steep learning curve,11 we found that departing PDs felt prepared for their positions.
Completing the NIPDD and having a stable, supported residency program may keep PDs in the role longer and allow them to plan their exits. The NIPDD, a 9-month fellowship operated by AFMRD, emphasizes leadership and personnel management skills, accreditation standards, and financial acumen.22 This study is the first to demonstrate that NIPDD completion is associated with longer PD tenure, contrary to a 2015 report indicating longer tenure for PDs who had not completed the NIPPD.23 Our results suggest that the current NIPPD curriculum prepares FM PDs to strategically build their program while empowering them to face challenges.
This survey and our prior work provide insight into the types of institutional support needed to retain PDs: providing resources to support staffing and faculty, understanding Accreditation Council for Graduate Medical Education program requirements for FM, and ensuring that institutional leaders understand the critical importance of alignment of FM program and institutional goals. A strength of this study is that we attempted to gather data from all departing program directors. The response rate was high. Our prior qualitative study did not include program directors who departed within 3 years.16 This census fills that gap, providing important information about PDs who depart after a brief tenure. While others have studied PDs who say they may leave their positions in the next year,11,24 ours is the first study to gather data from PDs who actually left.
The generalizability of these findings is limited by our small nonrandom sample, which may have been underpowered to detect other significant associations between decision factors and years in the PD role. The results are descriptive only and did not assess for potential confounders.
Individual factors (eg, choosing the timing of departing the role, NIPDD training), program factors (eg, succession planning/preparation), and institutional support for an FM residency program relate to PD retention and departure. Exploration of these factors may inform strategies to support PDs, FM residency programs, and their home institutions in maintaining stable programs.
Acknowledgments
The authors express their sincere thanks to Elizabeth W. Staton, MSTC, at the University of Colorado Department of Family Medicine, for her assistance editing this manuscript in preparation for submission.
References
- Bowen JL, Leff LE, Smith LG, Wolfsthal SD. Beyond the mystique of prestige: measuring the quality of residency programs. Am J Med. 1999;106(5):493-498.
- Hoekzema GS, Maxwell L, Gravel JW Jr, Mills WW, Geiger W. The residency performance index: an effort at residency quality assessment and improvement in family medicine. J Grad Med Educ. 2014;6(4):756-759. doi:10.4300/JGME-D-13-00355.1
- Pololi LH, Evans AT, Civian JT, Shea S, Brennan RT. Assessing the culture of residency using the c - change resident survey: validity evidence in 34 U.S. residency programs. J Gen Intern Med. 2017;32(7):783-789. doi:10.1007/s11606-017-4038-6
- Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Family Medicine.ACGME; 2023.
- Barton LL, Friedman AD. Stress and the residency program director. Arch Pediatr Adolesc Med. 1994;148(1):101-103. doi:10.1001/archpedi.1994.02170010103024
- Mitchell K, Maxwell L, Bhuyan N, et al. Program director turnover. Ann Fam Med. 2014;12(5):482-483. doi:10.1370/afm.1703
- Accreditation Council for Graduate Medical Education. Data Resource Book: Academic Year 2021-2022.ACGME; 2022.
- De Oliveira GS Jr, Almeida MD, Ahmad S, Fitzgerald PC, McCarthy RJ. Anesthesiology residency program director burnout. J Clin Anesth. 2011;23(3):176-182. doi:10.1016/j.jclinane.2011.02.001
- Porter M, Hagan H, Klassen R, Yang Y, Seehusen DA, Carek PJ. Burnout and resiliency among family medicine program directors. Fam Med. 2018;50(2):106-112. doi:10.22454/FamMed.2018.836595
- Beasley BW, Kern DE, Kolodner K. Job turnover and its correlates among residency program directors in internal medicine: a three-year cohort study. Acad Med. 2001;76(11):1,127-1,135. doi:10.1097/00001888-200111000-00017
- O’Connor AB, Halvorsen AJ, Cmar JM, et al. Internal medicine residency program director burnout and program director turnover: results of a national survey. Am J Med. 2019;132(2):252-261. doi:10.1016/j.amjmed.2018.10.020
- Kendall MC. Burnout in program directors: we still need more answers. Fam Med. 2018;50(6):481. doi:10.22454/FamMed.2018.755139
- Kane GC. Program director satisfaction revisited: an alternate view. Am J Med. 2010;123(3):E15. doi:10.1016/j.amjmed.2009.07.032
- Fernald DH, Hester CM, Brown SR. “We’ve really built something”: why family medicine program directors stay in their positions—a qualitative study. J Grad Med Educ. 2022;14(4):451-457. doi:10.4300/JGME-D-21-01160.1
- Yager J, Anzia JM, Bernstein CA, et al. What sustains residency program directors: social and interpersonal factors that foster recruitment and support retention. Acad Med. 2022;97(12):1,742-1,745. doi:10.1097/ACM.0000000000004887
- Fernald D, Hester CM, Brown SR. Why family medicine program directors leave their position. Fam Med. 2021;53(5):347-354. doi:10.22454/FamMed.2021.746153
- Hinchey KT, McDonald FS, Beasley BW. Sources of satisfaction: a second administration of the program director satisfaction survey. Am J Med. 2009;122(2):196-201. doi:10.1016/j.amjmed.2008.10.022
- Beasley BW, Kern DE, Howard DM, Kolodner K. A job-satisfaction measure for internal medicine residency program directors. Acad Med. 1999;74(3):263-270. doi:10.1097/00001888-199903000-00017
- Fernald DH, Hester CM, Brown S. AFMRD program director exit survey decision factors and rating scale. Society of Teachers of Family Medicine Resource Library; 2024. https://connect.stfm.org/viewdocument/afmrd-exit-survey-decision-factor-s?CommunityKey=90cceb35-312d-4bba-b27a-695f2da1f418&tab=librarydocuments
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi:10.1016/j.jbi.2008.08.010
- Harris PA, Taylor R, Minor BL, et al; REDCap Consortium. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi:10.1016/j.jbi.2019.103208
- Pugno PA, Dornfest FD, Kahn NB Jr, Avant R. The national institute for program director development: a school for program directors. J Am Board Fam Pract. 2002;15(3):209-213.
- Carek PJ, Mims LD, Conry CM, Maxwell L, Greenwood V, Pugno PA. Program director participation in a leadership and management skills fellowship and characteristics of program quality. Fam Med. 2015;47(7):536-540. https://www.stfm.org/familymedicine/vol47issue7/Carek536
- Khesroh E, Butt M, Kalantari A, et al. The use of emotional intelligence skills in combating burnout among residency and fellowship program directors. BMC Med Educ. 2022;22(1):127. doi:10.1186/s12909-022-03187-z