Introduction: Increasing student participation within the classroom can improve student engagement, the classroom environment, and student learning, and can provide for more diverse perspectives on the content. Think-pair-share (TPS) is an instructional strategy that can be used to promote and support student participation and enhance learning. Our study aimed to investigate the use of this strategy in early medical education.
Methods: Using content analysis of video recordings, equity mapping software, and student surveys, we examined the implementation of TPS in three different small groups of first-year medical students. We looked for increased student participation, equity in the distribution of student participation, and quality of discussion as evidence of TPS’s effectiveness in promoting student learning.
Results: TPS increased student participation and improved the quality of discussion. Additionally, students indicated TPS positively affected their learning, with the “thinking” and “pairing” time being especially important.
Conclusions: In utilizing TPS as an instructional strategy, medical educators can provide a structure that promotes a more equitable distribution of student participation, increased student interaction, and in-depth collaborative dialogue that enhance the overall learning experience.
Increasing student participation in collaborative dialogue can improve student engagement and provide opportunities for more diverse perspectives.1-5 Hearing student thoughts can also help instructors identify students’ level of understanding of material and adjust their instruction accordingly.6 Having a structure, such as think-pair-share (TPS), that promotes and scaffolds student discussion can be beneficial to the overall learning experience.2
TPS, a cooperative learning structure developed in K-12 education,7 involves three stages. First, students are given a set amount of time for individual thought on a given prompt. Then, they discuss their ideas and check their understanding with a partner. Finally, students engage in a whole-group discussion. While a few studies have begun to examine the effectiveness of TPS in health professions education, finding that TPS promotes clinical learning8 and enhances critical thinking,9 the utilization of this teaching strategy in early medical education has not been formally studied.
We conducted our study of the implementation of TPS with first-year students in a public, midwestern medical school whose program includes case-based learning, clinical experiences, and large- and small-group discussions. Approximately 200 demographically diverse students enter the program each year. After obtaining exemption from our institutional review board and informed consent from all participants, we implemented and studied TPS in three postclinic groups (PCGs). Led by a faculty physician, these compulsory groups met twice weekly throughout the first year. They were composed of seven to eight students who were intentionally mixed based upon MCAT scores, clinical experience, diversity measures (eg, gender, ethnicity), and certificate program. In the PCGs, students debriefed their clinical experiences and faculty covered content that consisted of patient cases focused on chief complaints and concerns and integrated basic, social, and clinical sciences. The faculty physician led each PCG session using a prepared slide presentation, asking individual students to read and respond to their respective slide in a round-robin fashion.
The three faculty physicians who volunteered to participate in this study were briefed on the TPS strategy. Then they identified two slides where they would utilize TPS in each of two PCG sessions. They video recorded these six sessions, which were then transcribed.
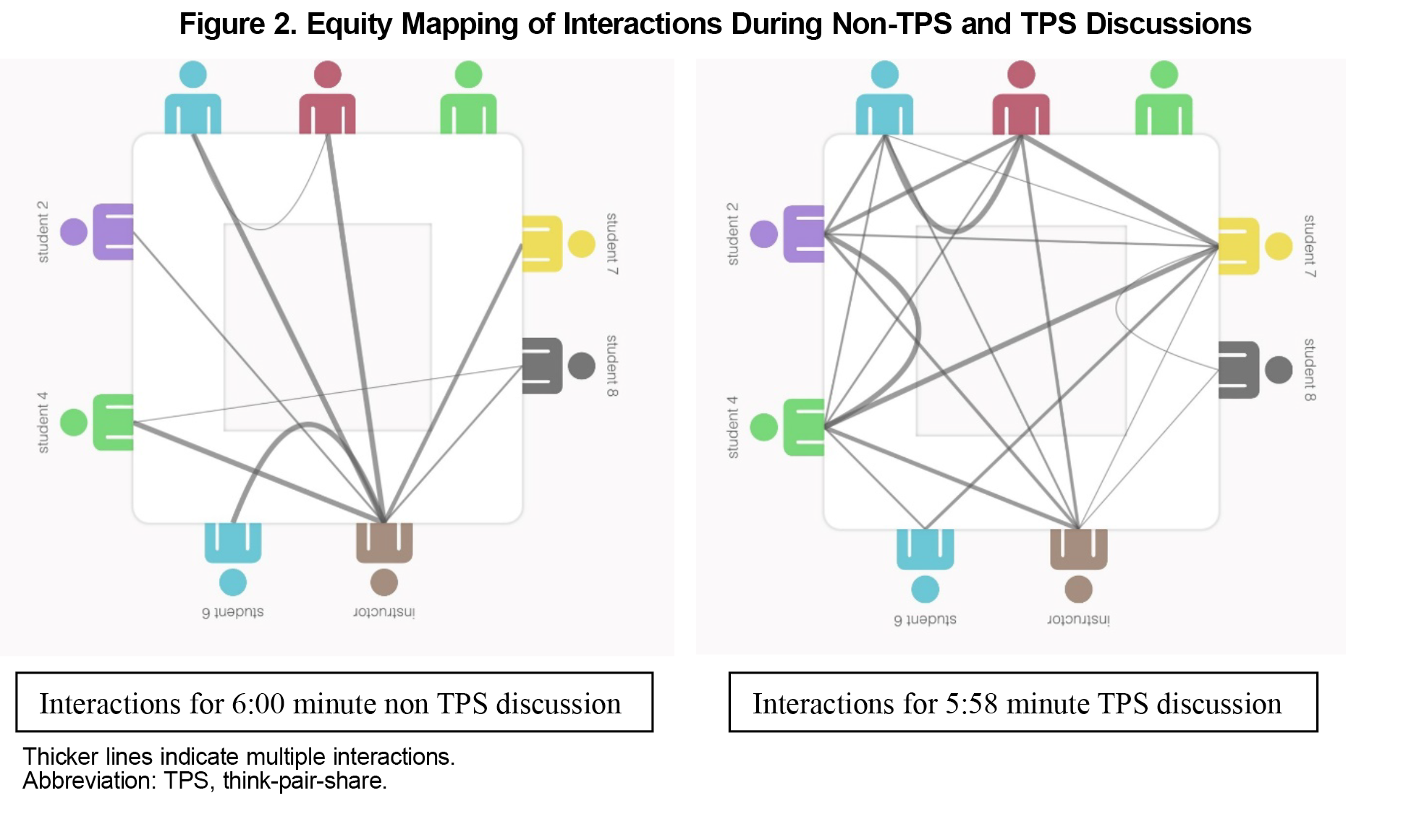
Using the videos and transcripts, the researchers collaboratively analyzed segments where TPS was implemented and segments where TPS was not implemented. We employed content analysis, coding for instances and types of talk (eg, prompting, joining, responding). Additionally, one of the researchers utilized equity mapping software10 to chart the instances of participation and interactions of the students and faculty to examine student participation patterns.11 We used the software to produce quantitative data for instances of participation and talk time for each individual as well as a visual representation of group interactions (Figure 2). Finally, we asked students to complete two informal, anonymous surveys12 to gather their honest opinions about TPS. Although not required, all 23 students chose to respond.
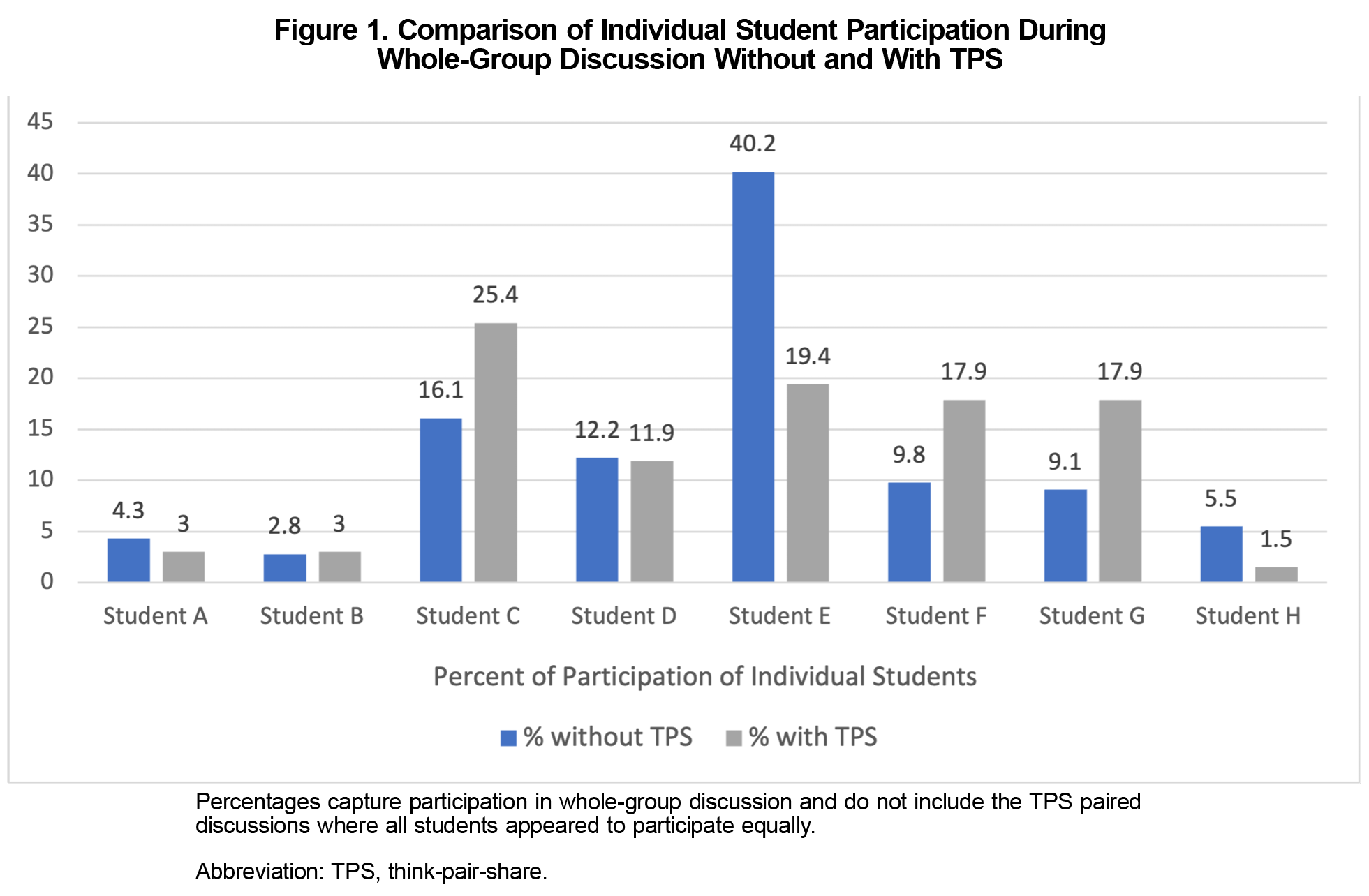
Our analysis of the data revealed the use of TPS positively influenced student participation and the quality of whole group discussion. We found a more equitable distribution of participation among students (Figure 1). Generally, students who participated less in non TPS group discussion were more vocal during the whole group “share” time when TPS was implemented. Students who tended to dominate discussion were less dominant during the TPS share time, allowing space for their peers to share their thinking. Importantly, while a few students participated very little in whole-group discussion (with or without TPS), we observed these same students actively engaging in discussion during the “pair” portion of TPS. All students shared ideas, discussed content, and asked questions, regardless of their partner.
Through our analysis of the videos, we also found that the discussions that took place during the share time of TPS were different in quality. The students were much more likely to have collaborative dialogue about the material rather than just one student responding to a slide or an instructor’s prompt. Representative of our data, equity maps for two 6-minute discussion segments within the same group (Figure 2), show considerably more student-to-student interactions than instructor-student-instructor interactions when TPS was utilized. Only two student-to-student interactions occurred during the non-TPS discussion whereas over 30 occurred during the TPS share time. During these interactions, we observed students building upon one anothers’ responses, asking clarifying questions of their peers, and answering those questions rather than deferring to the faculty physician.
The increased participation and improved quality of discussion were likely due to two factors: (1) the students were given time to think before responding; and (2) the students had opportunities to check their thinking and ask questions in pairs. Student responses on the surveys support these conclusions. Think time was deemed helpful by almost all students (91.7%). Multiple students commented that it gave them time to gather their thoughts.
Many students (72.7%) also indicated the partner discussion was helpful, largely because it increased their understanding of the content and confidence in speaking in the whole group. One student noted that they usually refrain from entering conversations due to others talking so much. They shared, “[in a] group full of extroverts, I appreciated the think-pair-share…. Pairing makes it low-stakes in terms of saying things incorrectly: I can fact check with my partner.” Another student commented, “I can share my ideas comfortably with one classmate before speaking with others.” Yet another student noted, “It helped to have someone to double agree/fix errors in understanding.” All these students noted that the opportunity to pair with a peer promoted their learning. Notably, nowhere in the videos we analyzed, other than during TPS, were students specifically given time to think and/or confer with a partner before responding.
In our study, using TPS as an instructional strategy increased student participation and interaction, promoted more equitable distribution of participation, and improved the quality of discussion. Thus, TPS proved to be an accessible instructional strategy that medical educators can utilize to enhance the learning experience. Due to a small sample size, further research using a larger sample size could be used to confirm these results and provide additional insight into the nuances of implementation.
Acknowledgments
Both authors participated in the research design and manuscript drafting. Dr Guenther was the lead author of the manuscript. Dr Abbott was the lead researcher of the project. Both authors thank Dr Marie Cole and Dr Jim Mayle for their contributions to this study.
Financial Support: No funding was received for conducting this study or preparation of this manuscript.
Presentations: Some of the content of this manuscript was presented by the authors at the STFM Conference on Medical Student Education in January 2022.
References
- Johnson DW, Johnson RT, Smith KA. Cooperative learning: improving university instruction by basing practice on validated theory. J on Excellence in University Teach.2014;25:1-26.
- Lange C, Costley J, Han SL. Informal cooperative learning in small groups: the effect of scaffolding on participation. Issues Educ Res. 2016;26:260-279.
- Rocca KA. Student participation in the college classroom: an extended multidisciplinary literature review. Communications Ed. 2010;59:185-213.
- Teaching Works. Eliciting and interpreting individual students’ thinking. Accessed August 7, 2022. https://library.teachingworks.org/curriculum-resources/teaching-practices/eliciting-and-interpreting/
- Webb NM. The teacher’s role in promoting collaborative dialogue in the classroom. Br J Educ Psychol. 2009;79(Pt 1):1-28. doi:10.1348/000709908X380772
- Ritchhart R, Church M, Morrison K. Making Thinking Visible.Jossey-Bass; 2011.
- Lyman F. The responsive classroom discussion. In: Anderson AS, ed. Mainstreaming Digest.University of Maryland College of Education; 1981:109-113.
- Ganatra S, Doblanko T, Rasmussen K, et al. Perceived effectiveness and applicability of Think-Pair-Share including Storytelling (TPS-S) to enhance clinical learning. Teach Learn Med. 2021;33(2):184-195. doi:10.1080/10401334.2020.1811094
- Kaddoura M. Think Pair Share: A teaching learning strategy to enhance students’ critical thinking. Educ Res Q. 2013;36:3-24.
- Equity maps description. Equity Maps. Accessed July 14, 2023. https://equitymaps.com/app-description/
- Reinholz DL, Shah N. Equity analytics: A methodological approach for quantifying participation patterns in mathematics classroom discourse. J Res Math Educ. 2018;49(2):140-177. doi:10.5951/jresematheduc.49.2.0140
- Abbott CM. Think Pair Share Student Survey Questions. STFM Resource Library. Accessed January 29, 2024. https://resourcelibrary.stfm.org/viewdocument/think-pair-share-student-survey-que?CommunityKey=2751b51d-483f-45e2-81de-4faced0a290a&tab=librarydocuments



There are no comments for this article.