Introduction: Little is known about how frequently family medicine (FM) clerkship directors remediate faculty with student mistreatment concerns and their comfort level in performing the remediations. In this exploratory study, we investigated factors associated with the number of faculty remediated for student mistreatment concerns by FM clerkship directors and the comfort level of FM clerkship directors in remediating these faculty.
Methods: Data were collected as part of the 2022 Council of Academic Family Medicine Educational Research Alliance (CERA) survey of FM clerkship directors. FM clerkship directors provided responses on how frequently they remediated faculty with mistreatment concerns and their comfort level in performing remediations.
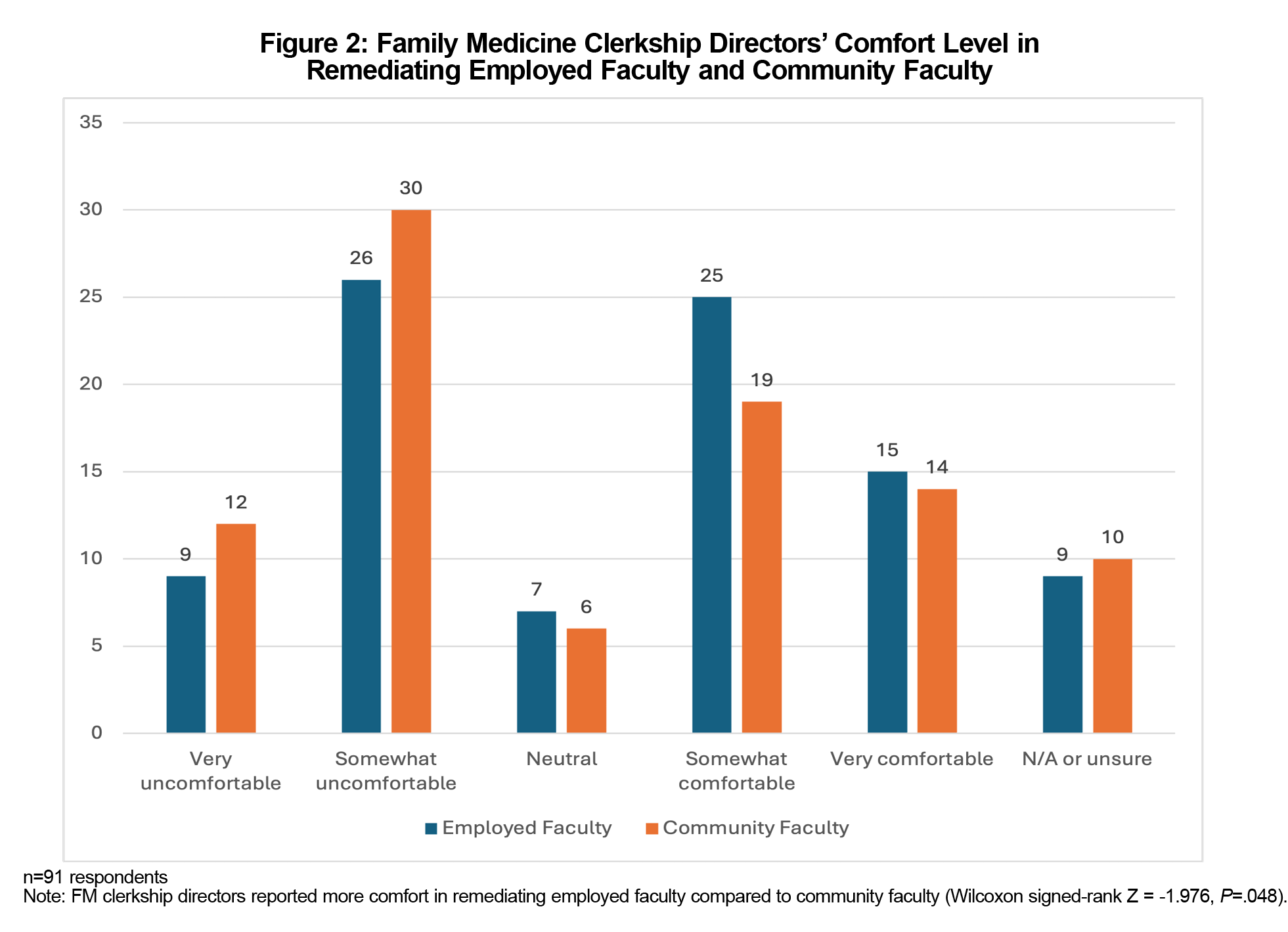
Results: Ninety-four of 159 FM clerkship directors (59.1%) responded to the survey. FM clerkship directors remediated more community faculty than employed faculty (P<.001). FM clerkship directors at schools where a larger percentage of students spent at least half of their rotation with a community faculty (P=.002) or where there were a higher percentage of paid community faculty (P=.004) were more likely to have remediated community faculty. FM clerkship directors reported more comfort in remediating employed faculty compared to community faculty (P=.048). FM clerkship directors with access to a formal mechanism for remediation (P=.016) or having a better adequacy in number of precepting sites (P=.041) reported higher comfort levels in remediating community faculty.
Conclusions: Our study identified factors associated with remediating family medicine clerkship faculty with mistreatment concerns. Additional research is needed to determine the most effective strategies to remediate faculty with mistreatment concerns.
Mistreatment of learners “occurs when behavior shows disrespect for the dignity of others and unreasonably interferes with the learning process.”1 Despite persistent efforts by medical schools to address mistreatment,2,3 students continue to frequently report mistreatment such as embarrassment, humiliation, and offensive sexist remarks on the 2023 Association of American Colleges (AAMC) Graduation Questionnaire.4 Learners may suffer posttraumatic stress symptoms, burnout, and suicidal thoughts due to mistreatment.5-10 While mistreatment less likely occurs on family medicine (FM) clerkships,4,11-12 Clerkship directors must still be prepared to handle mistreatment concerns. We previously investigated FM clerkship directors’ general handling of mistreatment concerns and found that FM clerkship directors frequently are the primary investigators of mistreatment concerns on their clerkship. We also investigated the process deciding whether to discontinue using a faculty preceptor due to a mistreatment concern and found that FM clerkship directors were active participants in this process.13
There are situations in which it is appropriate for the FM clerkship director to offer remediation to a faculty preceptor. In our previous study, we did not investigate the remediation of faculty with mistreatment concerns and acknowledge the necessity for further study on this topic. The question of whether successful remediation of a faculty preceptor can lead to a resumption of teaching requires further study, as there is “a paucity of evidence to guide best practices of remediation in medical education.”14 A few general reports14-16 and a few reports on remediating faculty in a similar situation, namely those with professionalism concerns,17,18 are available. A previous study identified common challenges with preceptor sites and explored the association of a system to remediate “teachers or clinical sites with performance issues” with the identification and retention of clinical sites.19 However, that report and others do not specifically address remediation of faculty with mistreatment concerns.
In our study, we investigated how often FM clerkship directors remediated faculty with mistreatment concerns and their comfort level in performing the remediations. We hypothesized that there are differences in the number of employed faculty and community faculty remediated by FM clerkship directors and in their comfort level in remediating these two groups. We sought to understand any factors associated with the differences.
Our study analyzed data obtained as part of the 2022 Council of Academic Family Medicine Educational Research Alliance (CERA) Family Medicine Clerkship Directors Survey. The Institutional Review Boards of the American Academy of Family Physicians and of Baylor College of Medicine approved this study in May 2022 and August 2022, respectively.
Survey Administration
CERA conducts regular surveys of family medicine educators, including clerkship directors.20 CERA sent a survey invitation to 148 US and 16 Canadian eligible family medicine clerkship directors on June 7, 2022, with the successful delivery of 159 invitations. CERA sent nonrespondents four weekly requests, plus one final request on the last day of the survey, July 8, 2022.
Survey Questions
Along with standardized demographic questions, the CERA survey included our questions on the presence of a formal mechanism for remediating faculty, the number of faculty remediated during the past 3 years due to student mistreatment concerns, the adequacy of precepting sites and the FM clerkship directors’ comfort level in remediating faculty with student mistreatment concerns. The FM clerkship directors rated their comfort level in remediating faculty using a 5-point Likert scale (1 = very uncomfortable to 5 = very comfortable).
Analysis
We analyzed our data using SPSS version 28.0 software (IBM Corp., Armonk, NY) to generate descriptive statistics, measures of association, and tests of significance (eg, Wilcoxon paired-signed ranks tests and Spearman’s ρ analysis). Unless otherwise noted, we included responses of “N/A or Unsure” in descriptive statistics summarizing survey responses but excluded them as nonresponses in measures of association and tests of significance.
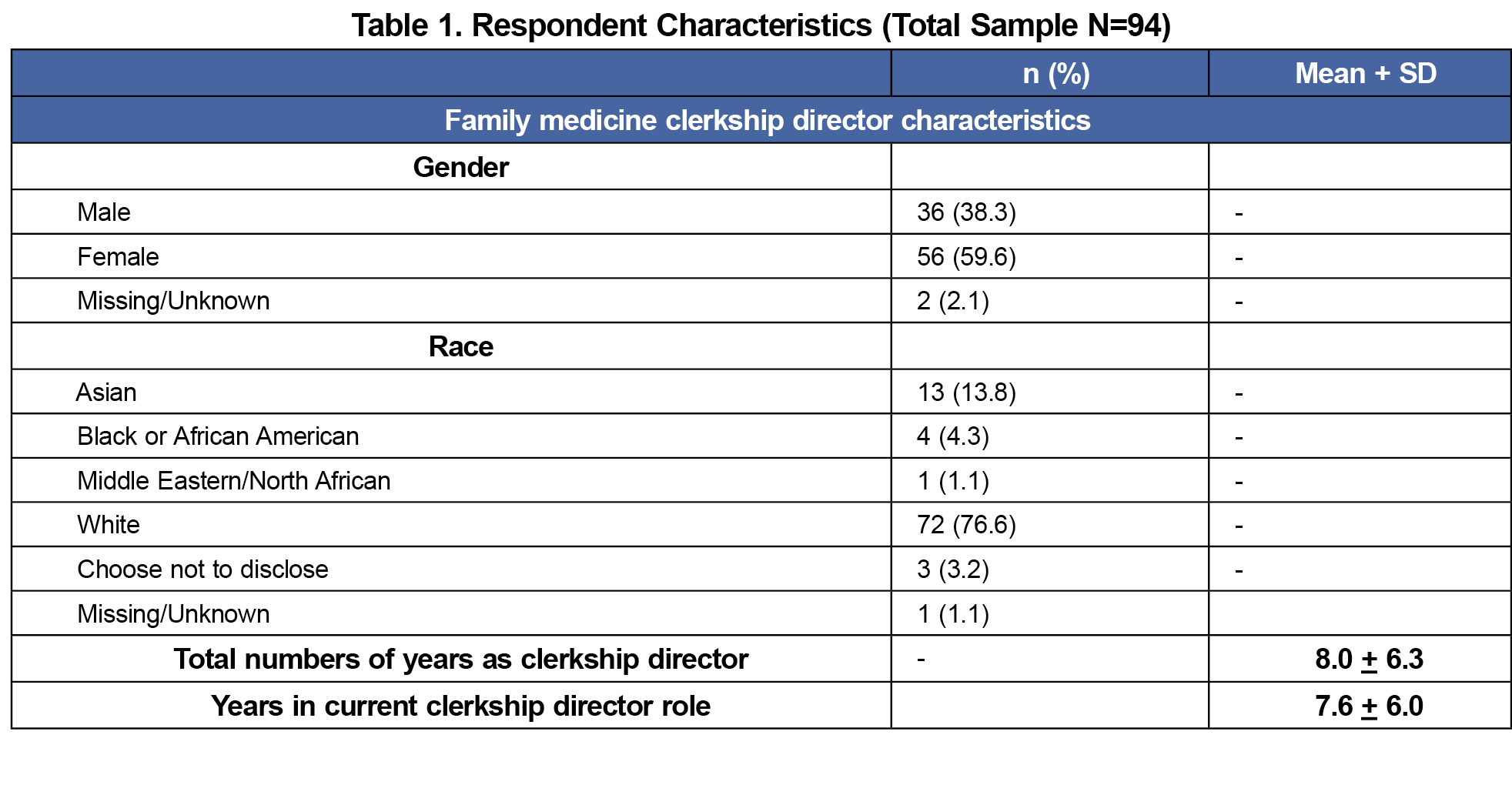
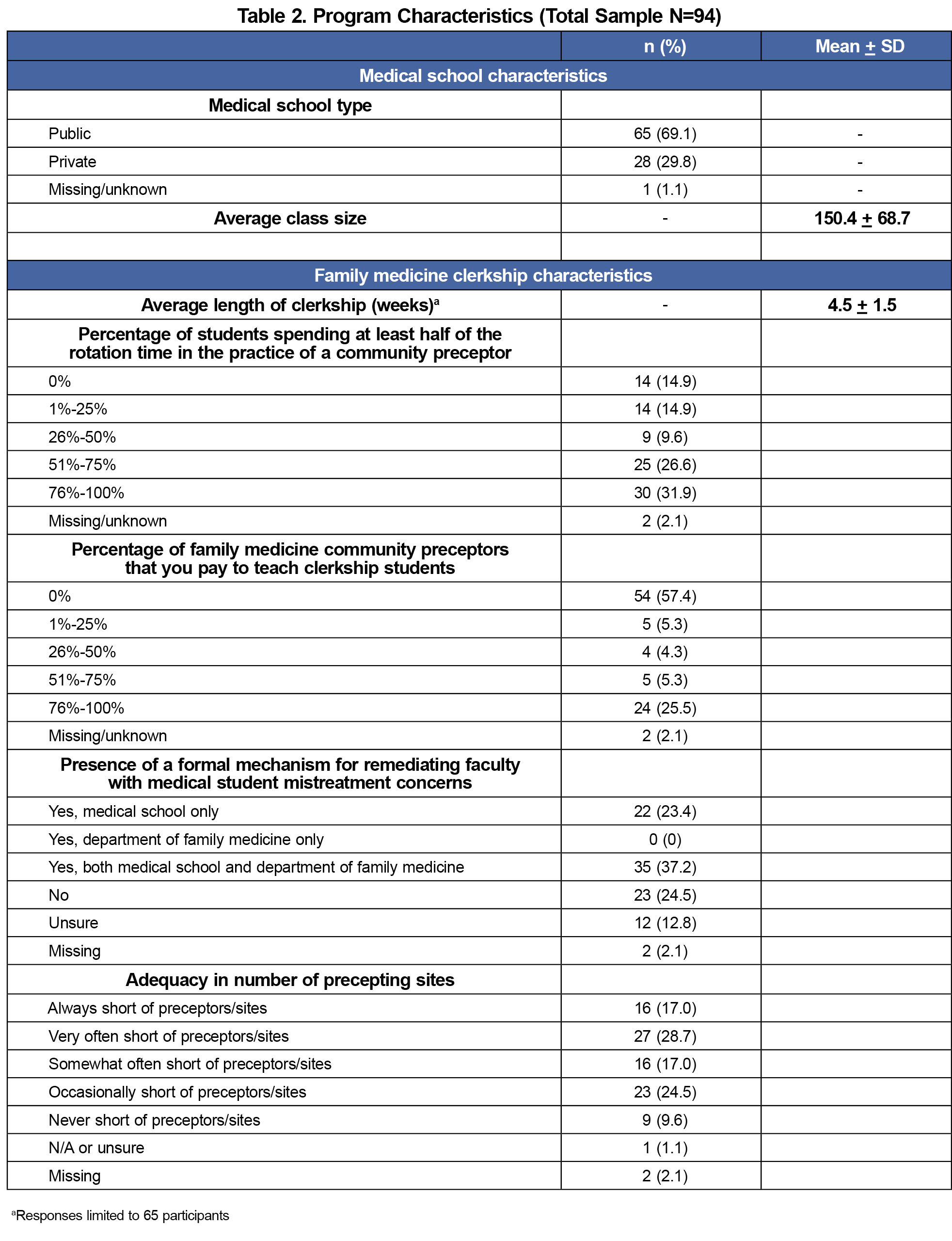
A total of 94 out of 159 FM clerkship directors (59.1% response rate) responded to the 2022 CERA Clerkship Directors survey. Data about respondents and their clerkships are summarized in Tables 1 and 2.
Over half (n=57, 60.6%) of respondents indicated that their medical school and/or department of family medicine had a formal mechanism for remediating faculty with mistreatment concerns (Table 2).
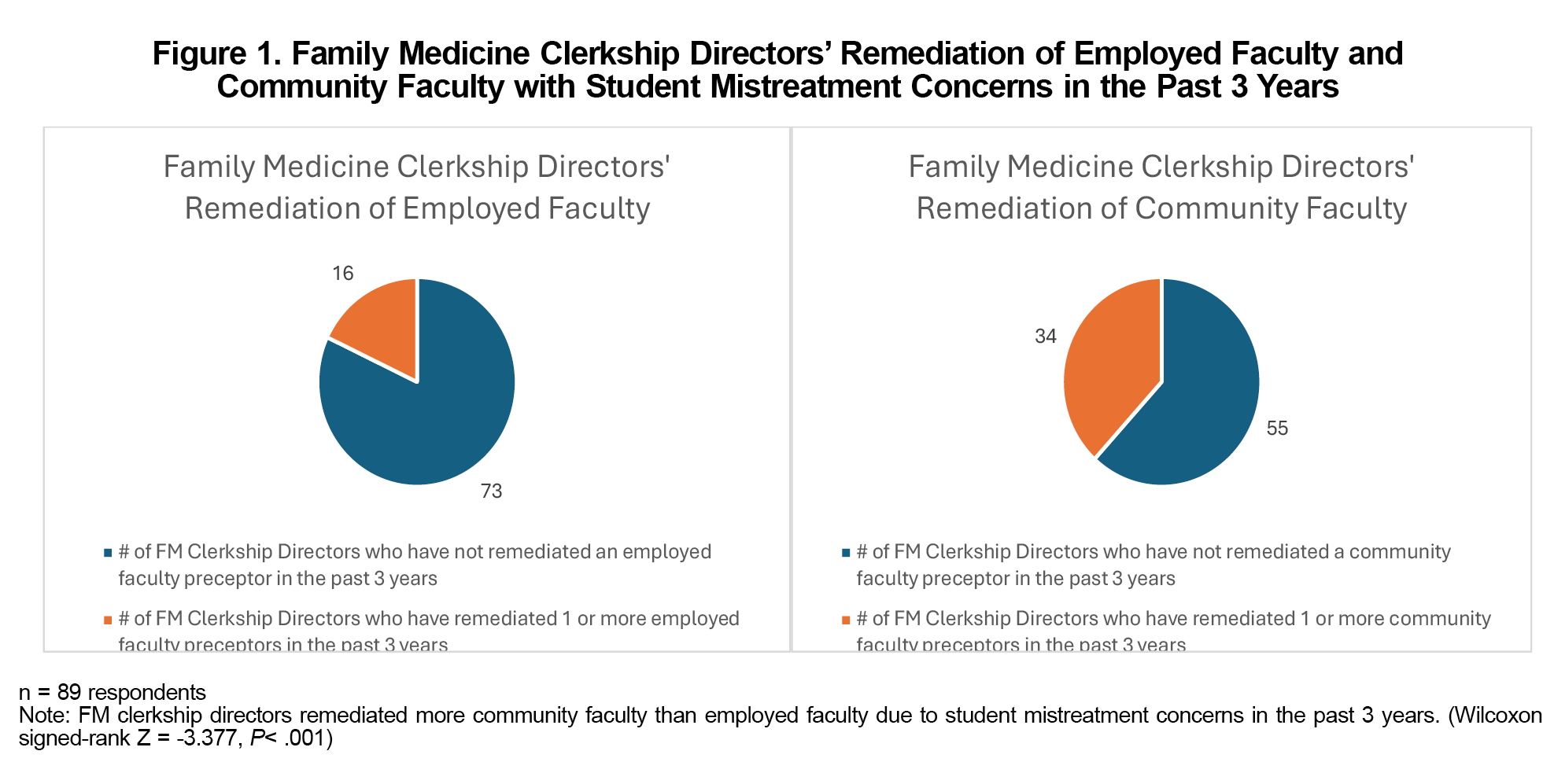
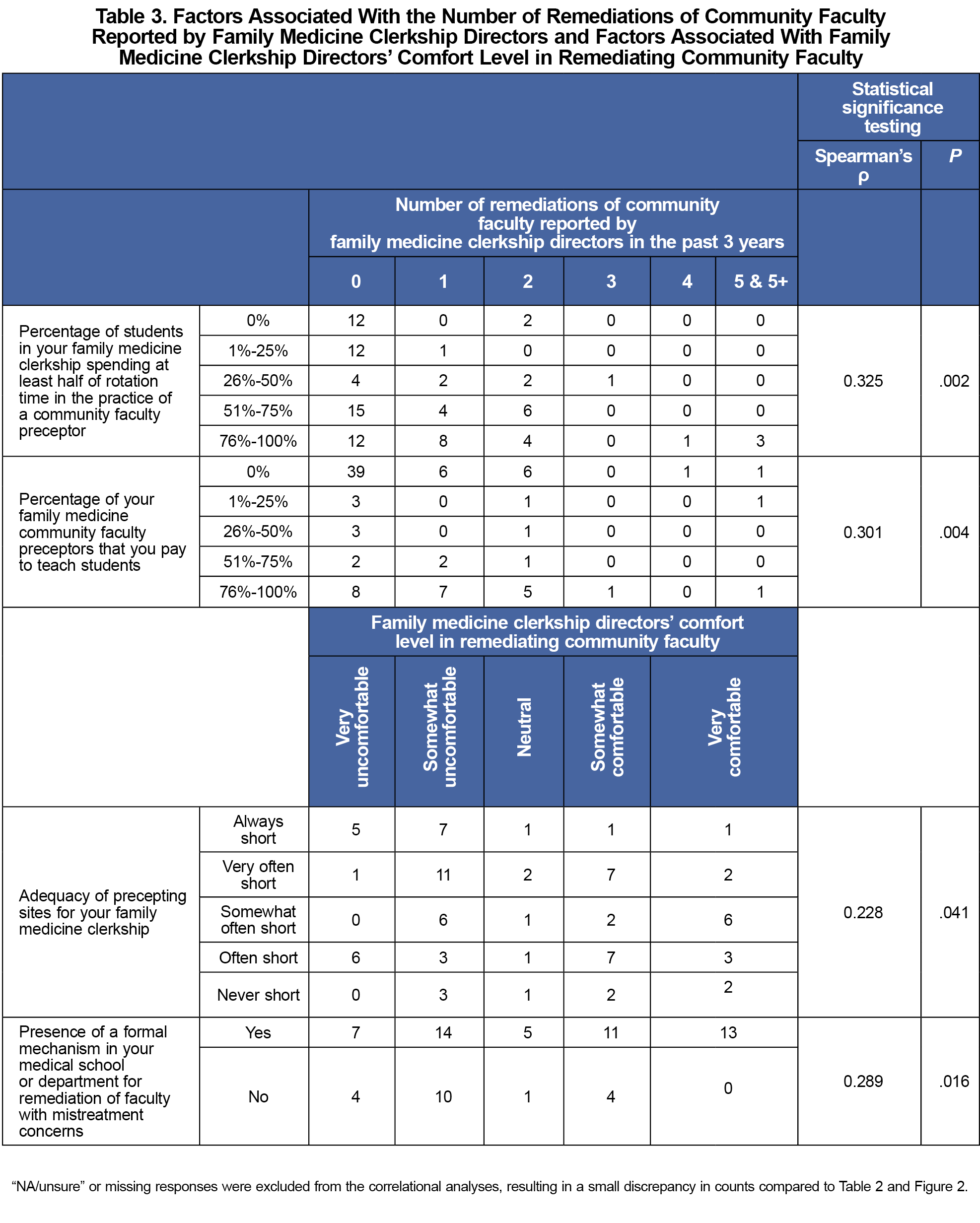
FM clerkship directors remediated more community faculty than employed faculty due to student mistreatment concerns in the past 3 years (Wilcoxon signed-rank Z=-3.377, P<.001; Figure 1). FM clerkship directors at schools where a larger percentage of students spent at least half of their rotation with community faculty (Spearman’s ρ=.325, P=.002) or where there was a higher percentage of paid community faculty (Spearman’s ρ=.301, P=.004) were more likely to have remediated community faculty with a medical student mistreatment concern. (Table 3) We did not identify any factors associated with the likelihood of remediating employed faculty.
FM clerkship directors reported more comfort in remediating employed faculty compared to community faculty (Wilcoxon signed-rank Z=-1.976, P=.048; Figure 2). FM clerkship directors in a school or department with a formal mechanism for remediation of mistreatment reported higher comfort levels in remediating community faculty for mistreatment (Spearman’s ρ=.289, P=.016), but not employed faculty. FM clerkship directors reporting higher levels of adequacy in number of preceptor sites reported higher levels of comfort in remediating community faculty (Spearman’s ρ=.228, P=.041), but not employed faculty (Table 3).
In this exploratory study, we found differences in the number of employed faculty and community faculty remediated by FM clerkship directors and in the comfort level of FM clerkship directors in remediating these two groups. We also identified factors associated with the differences.
Paying community faculty may give FM clerkship directors leverage to enforce accountability19,21 when addressing mistreatment concerns and increase the likelihood of remediation. If their institution does not pay community faculty, FM clerkship directors can still establish collaborative relationships with community faculty to facilitate any future remediation efforts.
In our previous study, factors such as adequacy of preceptor sites, paying community faculty, and the number of students who spent at least half of their time in the office of a community faculty preceptor were not associated with the comfort level of FM clerkship directors in their general handling and resolving of mistreatment reports.13 In this study, we investigated a more specific aspect of handling mistreatment concerns (the remediation of faculty), and found that adequacy of preceptor sites was associated with the FM clerkship directors’ comfort level in remediating community faculty.
Drowos and colleagues found that a remediation system was associated with less difficulty in identifying clinical sites and less removal of clinical sites for various performance concerns, which included but was not limited to mistreatment issues.19 Our study adds to these findings by demonstrating that a formal mechanism specifically for remediation of faculty with mistreatment concerns was associated with FM clerkship directors’ comfort in remediating community faculty but was not associated with their comfort in remediating employed faculty. Nevertheless, as 37% of FM clerkship directors stated there was no formal remediation policy at their institution for faculty with mistreatment concerns or were unsure of its existence, there is a need to develop formal remediation policies at those schools or more clearly communicate the policies that exist.
Limitations
Our findings are limited by restrictions on the number of survey questions allowed and the required closed-response format. There is a possibility of response bias (eg, social desirability bias), and recall bias due to the potential difficulty remembering events that occurred a few years ago. Our relatively small sample size may have resulted in type 2 errors, based on the limited power to identify significant predictors of comfort level.
Future Directions
Despite these limitations, our study demonstrates factors associated with FM clerkship directors’ remediation of faculty with mistreatment concerns.
An example of a detailed remediation plan for faculty with mistreatment concerns is available.22 Further research to investigate the effectiveness of different strategies may determine the best approach FM clerkship directors can use in remediating faculty with mistreatment concerns.
Acknowledgments
Presentations: Findings from this study were presented at the 2023 Society of Teachers of Family Medicine Annual Spring Conference in Tampa, Florida on May 2, 2023 and at the 2024 Association of American Medical Colleges: Southern Group on Educational Affairs meeting in Houston, Texas on April 12, 2024.
References
- Mavis B, Sousa A, Lipscomb W, Rappley MD. Learning about medical student mistreatment from responses to the medical school graduation questionnaire. Acad Med. 2014;89(5):705-711. doi:10.1097/ACM.0000000000000199
- Mazer LM, Bereknyei Merrell S, Hasty BN, Stave C, Lau JN. Assessment of programs aimed to decrease or prevent mistreatment of medical trainees. JAMA Netw Open. 2018;1(3):e180870. doi:10.1001/jamanetworkopen.2018.0870
- Fried JM, Vermillion M, Parker NH, Uijtdehaage S. Eradicating medical student mistreatment: a longitudinal study of one institution’s efforts. Acad Med. 2012;87(9):1191-1198. doi:10.1097/ACM.0b013e3182625408
- Association of American Medical Colleges. Medical School Graduation Questionnaire: 2023 All Schools Summary Report. July 2023. Accessed June 19, 2024. https://www.aamc.org/data-reports/students-residents/report/graduation-questionnaire-gq
- Heru A, Gagne G, Strong D. Medical student mistreatment results in symptoms of posttraumatic stress. Acad Psychiatry. 2009;33(4):302-306. doi:10.1176/appi.ap.33.4.302
- Cook AF, Arora VM, Rasinski KA, Curlin FA, Yoon JD. The prevalence of medical student mistreatment and its association with burnout. Acad Med. 2014;89(5):749-754. doi:10.1097/ACM.0000000000000204
- Hu YY, Ellis RJ, Hewitt DB, et al. Discrimination, abuse, harassment, and burnout in surgical residency training. N Engl J Med. 2019;381(18):1741-1752. doi:10.1056/NEJMsa1903759
- Kemper KJ, Schwartz A; Pediatric Resident Burnout-Resilience Study Consortium. Bullying, discrimination, sexual harassment, and physical violence: common and associated with burnout in pediatric residents. Acad Pediatr. 2020;20(7):991-997. doi:10.1016/j.acap.2020.02.023
- Dyrbye L, Satele D, West CP. A longitudinal national study exploring impact of the learning environment on medical student burnout, empathy, and career regret. Acad Med. 2021;96(11S):S204-S205. doi:10.1097/ACM.0000000000004285
- Gianakos AL, Freischlag JA, Mercurio AM, et al. Bullying, discrimination, harassment, sexual harassment, and the fear of retaliation during surgical residency training: a systematic review. World J Surg. 2022;46(7):1587-1599. doi:10.1007/s00268-021-06432-6
- Oser TK, Haidet P, Lewis PR, Mauger DT, Gingrich DL, Leong SL. Frequency and negative impact of medical student mistreatment based on specialty choice: a longitudinal study. Acad Med. 2014;89(5):755-761. doi:10.1097/ACM.0000000000000207
- Breed C, Skinner B, Purkiss J, et al. Clerkship-specific medical student mistreatment. Med Sci Educ. 2018;28(3):477-482. doi:10.1007/s40670-018-0568-8
- Huang WY, Purkiss J, Eden AR, Appelbaum N. Family medicine clerkship directors’ handling of student mistreatment: results from a CERA survey. Fam Med. 2020;52(5):324-331. doi:10.22454/FamMed.2020.409025
- Hauer KE, Ciccone A, Henzel TR, et al. Remediation of the deficiencies of physicians across the continuum from medical school to practice: a thematic review of the literature. Acad Med. 2009;84(12):1822-1832. doi:10.1097/ACM.0b013e3181bf3170
- Guerrasio J, Garrity MJ, Aagaard EM. Learner deficits and academic outcomes of medical students, residents, fellows, and attending physicians referred to a remediation program, 2006-2012. Acad Med. 2014;89(2):352-358. doi:10.1097/ACM.0000000000000122
- Fainstad T, Ebel B. Faculty remediation coaching: invest time to build trust. Med Educ. 2020;54(5):478-479. doi:10.1111/medu.14089
- Cherr GS, Orrange SM, Berger RC. Remediation of the struggling clinical educator. J Grad Med Educ. 2019;11(1):6-9. doi:10.4300/JGME-D-18-00262.1
- Morgenstern BZ, Beck Dallaghan GL, Horak HA, et al, eds. Alliance for Clinical Education. Guidebook for clerkship directors.5th ed. Gegensatz Press; 2019.
- Drowos J, Sairenji T, Watson KH, et al. Identifying and remediating quality issues at clinical teaching sites: A CERA clerkship directors survey. Fam Med. 2019;51(10):811-816. doi:10.22454/FamMed.2019.838842
- Seehusen DA, Mainous AG III, Chessman AW. Creating a centralized infrastructure to facilitate medical education research. Ann Fam Med. 2018;16(3):257-260. doi:10.1370/afm.2228
- Christner JG, Beck Dallaghan G, Briscoe G, et al. To pay or not to pay community preceptors? That is a question…. Teach Learn Med. 2019;31(3):279-287. doi:10.1080/10401334.2018.1528156
- Saint Louis University School of Medicine. Process for Faculty Remediation. Accessed June 19, 2024. https://www.slu.edu/medicine/professional-oversight/faculty-process.php.



There are no comments for this article.