Introduction: Posterior canal-type benign paroxysmal positional vertigo (BPPV) is commonly treated using the Epley maneuver; however, the maneuver’s use in primary care is limited by insufficient expertise. Therefore, this study aimed to evaluate the efficacy of a three-dimensional (3D) semicircular canal model as a self-learning tool for primary care physicians to improve their Epley maneuver technique.
Methods: Thirty-one participants (18 family physicians, seven residents, and six medical students) performed the Dix–Hallpike maneuver on a nursing manikin, followed by the Epley maneuver on the covered 3D models before and after a 5-minute self-study period with the uncovered 3D model. We measured the number of moved beads from posterior canal into the utricle of the 3D model, time spent on the Epley maneuver, and head suspension angle of the Dix–Hallpike maneuver.
Results: Preintervention performance was divided into a skilled group (n=7) that could move almost all the beads and an unskilled group (n=24) that could move a few beads. Postintervention, the unskilled group members significantly improved their skill: The average moved beads increased from 0.35 to 8.00, maneuver time from 26.1 to 35.8 seconds, and head suspension angle from 10.3° to 16.4°. Most participants recognized the importance of correct positioning and spent adequate time.
Conclusions: The 3D model was effective as a self-learning tool for improving Epley maneuver performance, particularly for less experienced practitioners. This approach could bridge the gap between evidence and practice in primary care for BPPV treatment, enhancing patient outcomes and reducing the need for specialist referrals.
Benign paroxysmal positional vertigo (BPPV) is a common vestibular disorder encountered by primary care physicians,1 arising from the displacement and migration of canaliths within semicircular canals. The Epley maneuver is a canalith-repositioning physiotherapy for posterior canal BPPV, the most common type, promoting the migration of canaliths to the utricule.2,3 Although the effectiveness of the Epley maneuver is well established, its use in primary care settings is limited due to insufficient expertise and time constraints.4,5 Existing training tools, such as videos and animations,6 lack experiential learning. Traditional training with volunteers is often impractical due to time, cost, and accessibility issues. Moreover, many clinicians have never had their Epley procedure performance objectively evaluated.
Fujisaka et al highlighted the efficacy of a three-dimensional (3D) head model (KEZLEX #D63) for teaching the Epley maneuver to medical students.7,8 This model features semicircular canals that are 10 times larger than normal, filled with a clear, viscous fluid, and containing 10 red beads representing canaliths. This study aimed to investigate the efficacy of this 3D model as a self-learning tool for primary care physicians to learn the Epley maneuver effectively. Additionally, we evaluated the Dix–Hallpike maneuver, a diagnostic method that identifies posterior canal BPPV and serves as the first step of the Epley maneuver.
This intervention study included 31 participants (including 6 female participants): 18 certified family physicians, seven residents of general internal medicine, and six medical students interested in primary care. This study was performed in accordance with the Declaration of Helsinki and was approved by the Ethical Review Board of Toyama University Hospital (approval number: 2023094).
Before the intervention, participating physicians completed a questionnaire regarding years of clinical experience and familiarity with the Epley maneuver. All participants reviewed an illustration of the Dix–Hallpike and Epley maneuvers published in UpToDate before evaluation.9
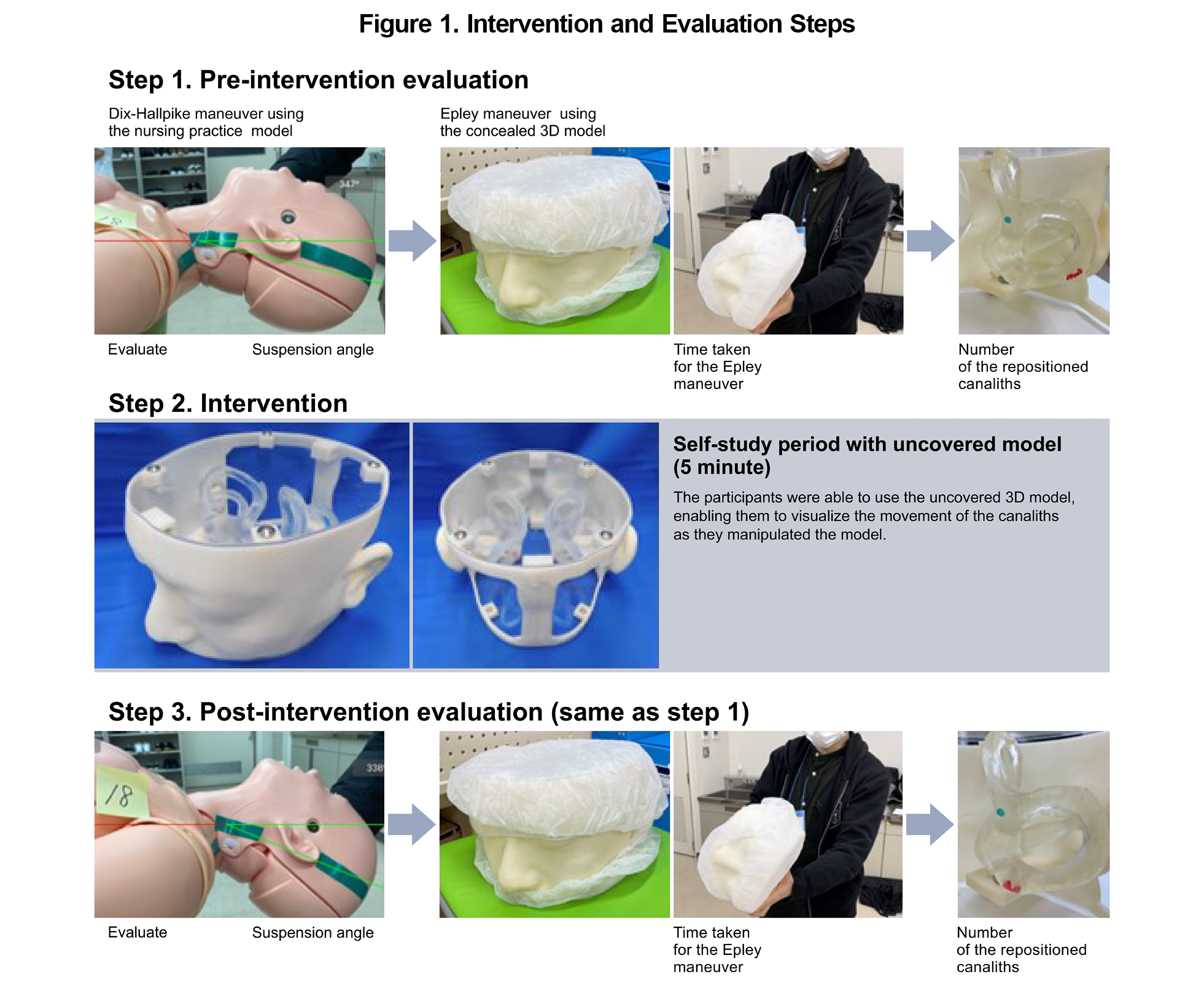
The intervention and evaluation steps are shown in Figure 1. In the preintervention evaluation, participants first performed the Dix–Hallpike maneuver on a nursing practice model (MW25, Kyoto Science).10 This manikin has multimovable joints, including the head and neck. Subsequently, participants performed the Epley maneuver using the 3D semicircular canal model, starting from the final head position of the Dix–Hallpike maneuver. The 3D model was covered by double surgical caps to obscure the internal beads. Before each evaluation, the examiner placed all 10 beads in the posterior canal. During the intervention, participants had a 5-minute self-study period with the uncovered 3D model, allowing them to manipulate the model individually and observe the movement of the canaliths. No instruction or guidance was provided by the examiner during this period.
For postintervention evaluation, participants performed the Dix–Hallpike and Epley maneuvers in the same manner as the preintervention evaluation. Thereafter, they completed a second questionnaire regarding their subjective understanding of the Epley maneuver, its practicality, and tips for successfully implementing the techniques learned during the intervention.
The primary outcome was the number of red beads moved from the posterior canal into the utricle. The secondary outcomes included time required to perform the Epley maneuver and suspension angle at the last phase of the Dix–Hallpike maneuver, which is also the first step of the Epley maneuver. Although the head rotation angle at this point is important, we could not assess it due to the model's limited range of motion. Pre- and postintervention outcomes were compared using Wilcoxon’s signed-rank test, with statistical significance set at P<.05.
The average clinical experience of participants was 7.6 years, with 69.6% having previous experience using the Epley maneuver.
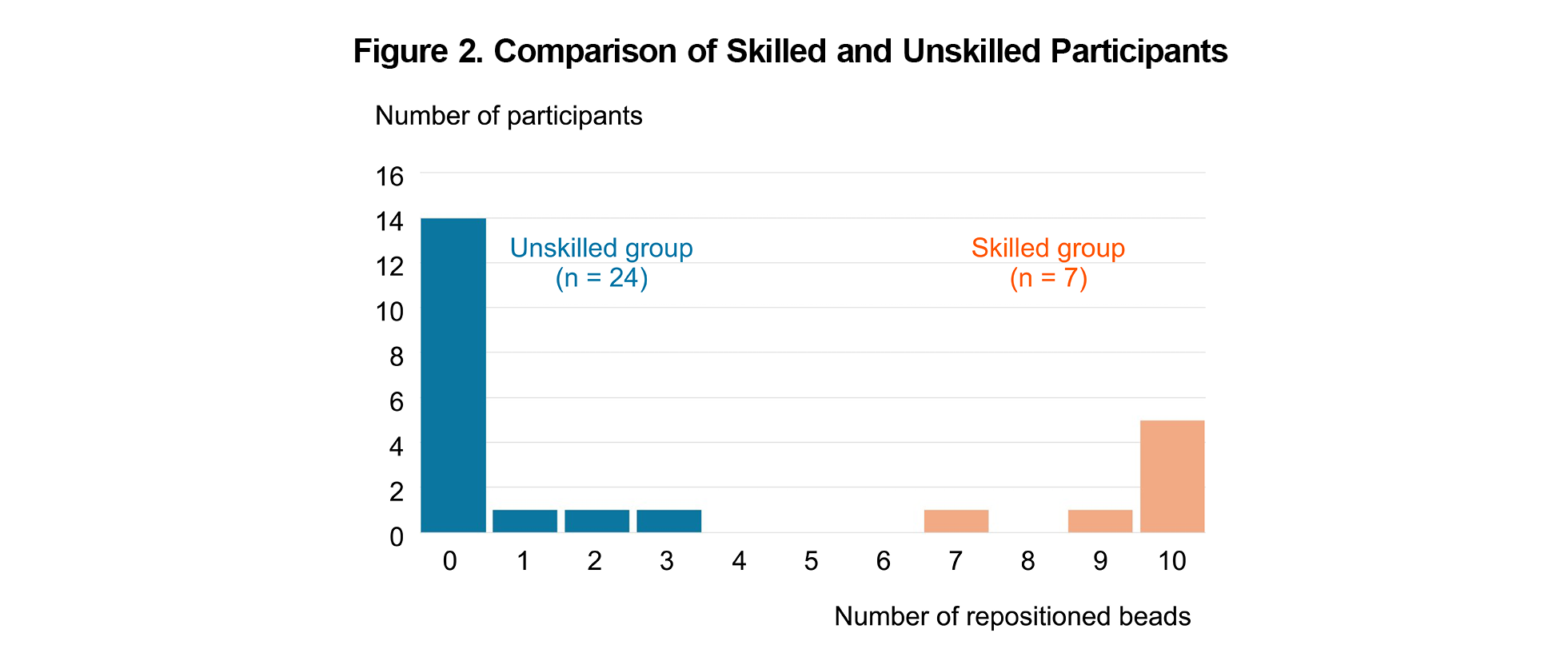
In the preintervention evaluation, participants’ performance was divided into a small skilled group that could move almost all the beads and a large unskilled group that could move a few beads (Figure 2). Two medical students were in the skilled group. The skilled group spent more time on the Epley maneuver (25.4 s vs 56 s, P<.01) and had a deeper suspension angle in the last phase of the Dix–Hallpike maneuver than the unskilled group, although this was not statistically significant (10.3° vs 15.1°, P>.1).
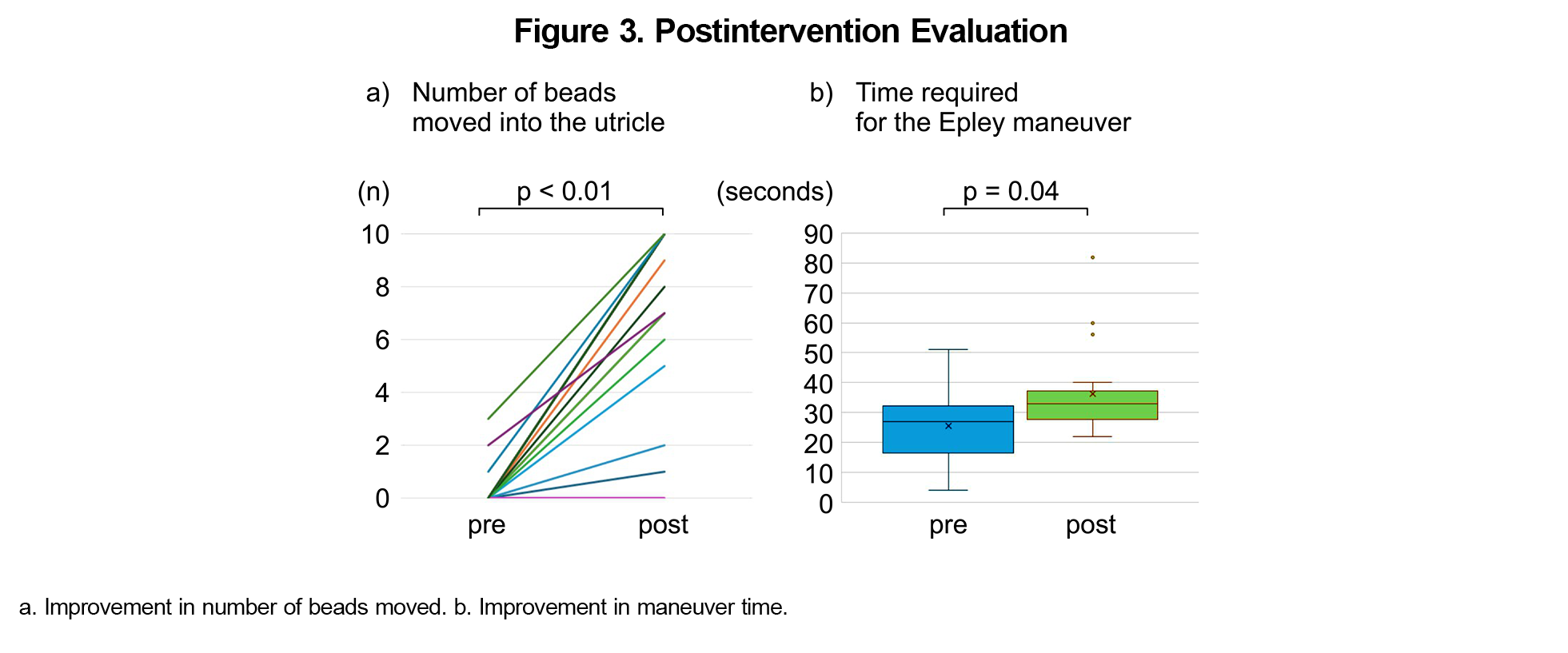
In the postintervention evaluation, the unskilled group members significantly improved their skills: The average number of moved beads increased from 0.35 to 8.00, maneuver time from 26.1 to 35.8 seconds (Figure 3), and mean head suspension angle at the end of the Dix–Hallpike maneuver from 10.3° to 16.4° (P=.024). The skilled group performed well, as in the preintervention evaluation. The three participants who could barely move the beads at the postintervention assessment completed the technique under the guidance of the instructor.
The postintervention questionnaire indicated that 70% of participants recognized that maintaining the correct head angle and holding the head position for a while at each step were crucial for the success of the Epley maneuver.
The study findings highlight the effectiveness of the 3D model as a self-learning tool for improving the participants’ performance of the Epley maneuver. Unlike previous studies on theoretical or video-based training, this study emphasized the effectiveness of practical experience using a physical model. Hands-on training has been reported to be effective in mastering the Epley maneuver.11,12 However, such training methods require accessible resources, a teaching coach, and significant time commitment. In contrast, the 3D model offers a versatile, time-efficient, and self-training method that is useful in settings with limited resources or training opportunities. This approach may bridge the gap between evidence and practice in primary care for BPPV treatment, potentially improving patient outcomes and reducing the reliance on specialist referrals.13
The study had limitations, including its small sample size, single intervention, and lack of a control group. In conclusion, the 3D model serves as an effective self-learning tool for improving Epley maneuver performance, particularly for less experienced primary practitioners. However, the number of moved beads may not directly correlate with clinical efficacy. Future studies should involve periodic evaluations using the model and assess its effectiveness in clinical practice.
Acknowledgments
We thank Editage (www.editage.jp) for English language editing.
Presentation: This study was presented at the 15th Annual Conference of Japan Primary Care Association, June 8, 2024, Hamamatsu, Japan.
References
- Grill E, Strupp M, Müller M, Jahn K. Health services utilization of patients with vertigo in primary care: a retrospective cohort study. J Neurol. 2014;261(8):1,492-1,498. doi:10.1007/s00415-014-7367-y
- Hilton MP, Pinder DK. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2014; (12):CD003162. doi:10.1002/14651858.CD003162.pub3
- Ballve Moreno JL, Carrillo Muñoz R, Villar Balboa I, et al. Effectiveness of the Epley’s maneuver performed in primary care to treat posterior canal benign paroxysmal positional vertigo: study protocol for a randomized controlled trial. Trials. 2014;15(1):179. doi:10.1186/1745-6215-15-179
- Glasziou P, Heneghan C. Epley and the slow boat from research to practice. Evid Based Med. 2008;13(2):34-35. doi:10.1136/ebm.14.2.34
- Cranfield S, Mackenzie I, Gabbay M. Can GPs diagnose benign paroxysmal positional vertigo and does the Epley manoeuvre work in primary care? Br J Gen Pract. 2010;60(578):698-699. doi:10.3399/bjgp10X515557
- Kerber KA, Burke JF, Skolarus LE, et al. A prescription for the Epley maneuver: www.youtube.com? Neurology. 2012;79(4):376–380. doi:10.1212/WNL.0b013e3182604533
- Fujisaka M, Akaogi K, Shojaku H. A tangible head model showing semicircular canals for demonstrating the physical treatment for BPPV. Acta Otolaryngol. 2015;135(12):1,212-1,218. doi:10.3109/00016489.2015.1064546
- KEZLEX. BPPV training model. Accessed July 16, 2024. https://www.kezlex.com/en/products/ent/d63
- Barton JJS. Benign paroxysmal positional vertigo. In: Connor RF, ed. UpToDate. Wolters Kluwer.
- Kyoto Kagaku. Patient care simulator “Yaye.” Accessed July 16, 2024. https://www.kyotokagaku.com/en/products_introduction/mw25
- Patiño JEP, Moreno JLB, Matos YR, et al. Effectiveness of a training intervention to improve the management of vertigo in primary care: a multicentre cluster-randomised trial, VERTAP. Trials. 2022;23(1):608. doi:10.1186/s13063-022-06548-7
- Kerber KA, Damschroder L, McLaughlin T, et al. Implementation of evidence-based practice for benign paroxysmal positional vertigo in the emergency department: a stepped-wedge randomized trial. Ann Emerg Med. 2020;75(4):459-470. doi:10.1016/j.annemergmed.2019.09.017
- Ulytė A, Valančius D, Masiliūnas R, et al. Diagnosis and treatment choices of suspected benign paroxysmal positional vertigo: current approach of general practitioners, neurologists, and ENT physicians. Eur Arch Otorhinolaryngol. 2019;276(4):985-991. doi:10.1007/s00405-019-05313-y



There are no comments for this article.