Introduction: Procedure training in family medicine residency is important for future full-spectrum practice. Some residency programs have cited difficulty providing adequate procedure education. Residency collaboration with nonfaculty attending physicians working at community nonresidency clinics may help programs increase resident exposure to procedures. We assessed the feasibility of such an educational model by establishing recurring procedure clinics in a nonresidency family medicine site supervised by nonfaculty physicians.
Methods: Twice monthly, half-day procedure clinics were conducted at a community site, where family medicine residents were supervised by nonfaculty community family physicians. After participation, we surveyed residents about their perceptions of the clinics. Using retrospective chart review, we determined quantity and type of procedures performed.
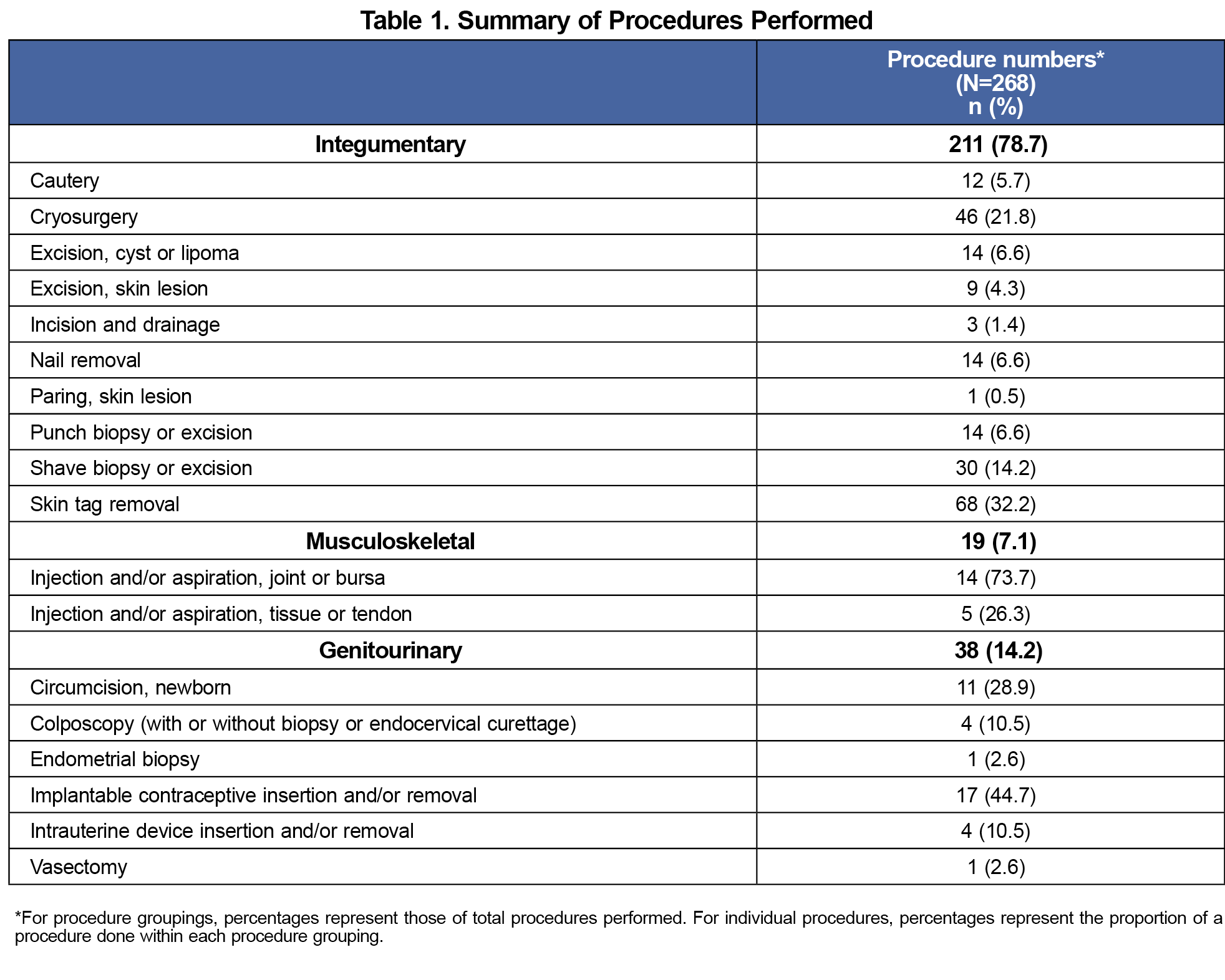
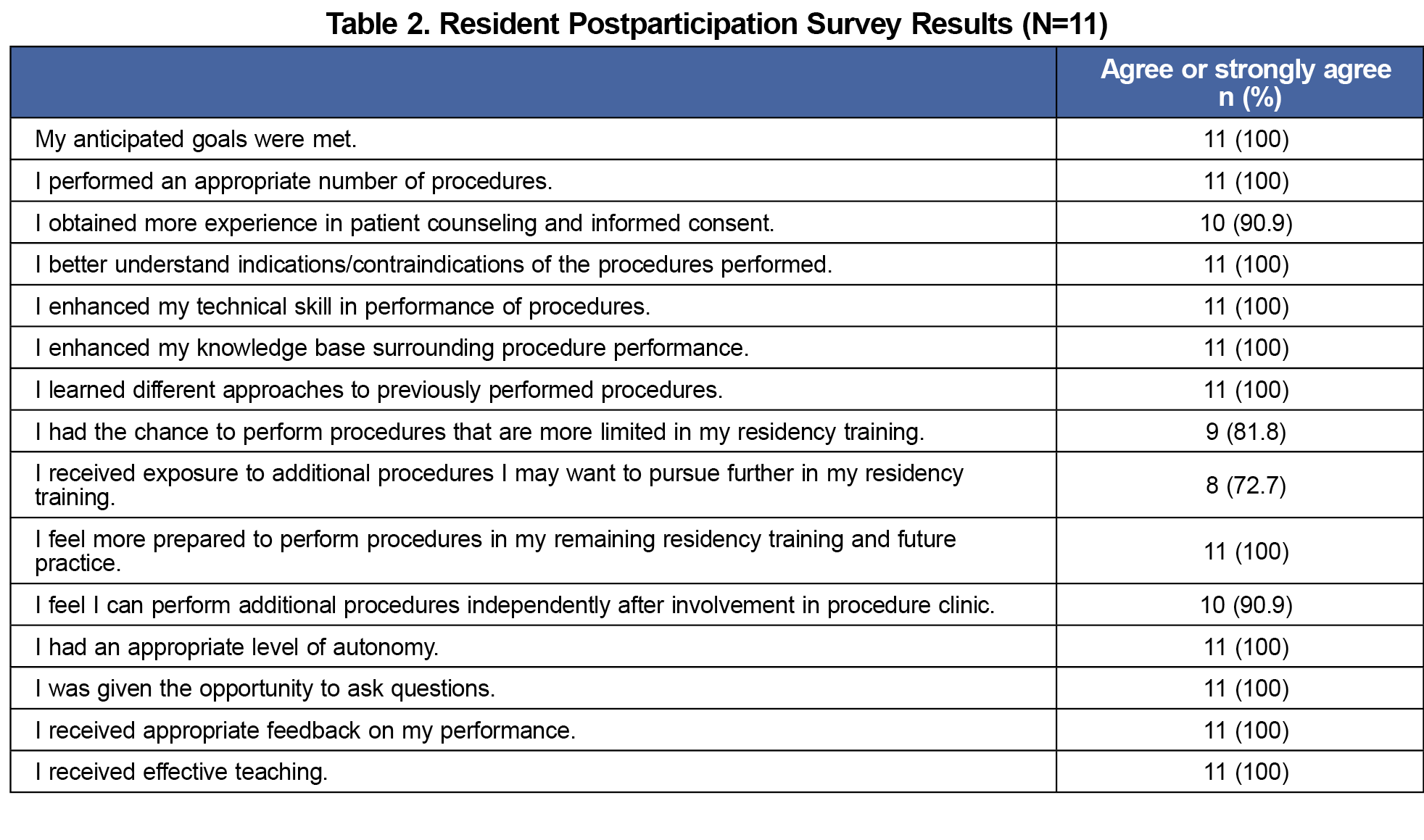
Results: Fifteen residents participated in 21 procedure clinics, featuring 18 procedure types and 268 procedures. Skin lesion excision, nail removal, punch and shave procedures, joint injection, newborn circumcision, and implantable contraception management were most consistently performed. Residents rated clinics highly and were satisfied with procedure number and variety, opportunity to learn new procedures and techniques, and feedback received. Over 80% of residents noted experiences in procedures that were less commonly encountered in their residency.
Conclusion: Procedure clinics at a nonresidency site hosted by nonfaculty attending physicians provided additional training in a variety of primary care procedures. The clinics were favorable to residents and may help programs address training gaps.
Procedural acquisition is important for family medicine training and is valued by residents and faculty.1-4 Procedure performance is associated with improved job satisfaction and increased reimbursement.5-7 Conversely, inadequate procedure training predicts lack of future procedure performance and may affect the ability of residency graduates to meet the needs of patients and health systems.8-11 Some family medicine residencies have cited difficulty meeting procedural training needs within their clinics due to a number of factors including low procedure volumes, lack of qualified faculty preceptors, or difficulty scheduling procedures into resident clinics.11-16 Dedicated procedure clinics have been used to address deficiencies and have been associated with increased procedural exposure, increased attainment of procedural comfort among residents, and high resident satisfaction.14-16 In an effort to expand upon limitations in procedure availability within one residency, the program piloted a procedure clinic based in a community site that was supervised by residency faculty. Although successful at increasing resident procedure exposure, they also noted potential difficulty in maintaining faculty funding for this clinic.14
An alternative solution could involve resident teaching by community primary care physicians in nonresidency procedure clinics. This model could potentially increase resident procedure exposure while not adding additional strain on faculty resources. We sought to assess the feasibility of community procedure clinics hosted by nonfaculty family medicine attending physicians. We hypothesized that such clinics would increase resident procedural numbers and would be viewed favorably by participating residents.
Twice monthly, half-day procedure clinics were established at a nonresidency family medicine office, in collaboration with a local residency. Two nonfaculty attending physicians with a broad scope of procedural practice volunteered to participate. Each attending physician supervised one resident per clinic. Patients were referred to the clinics internally at the community site.
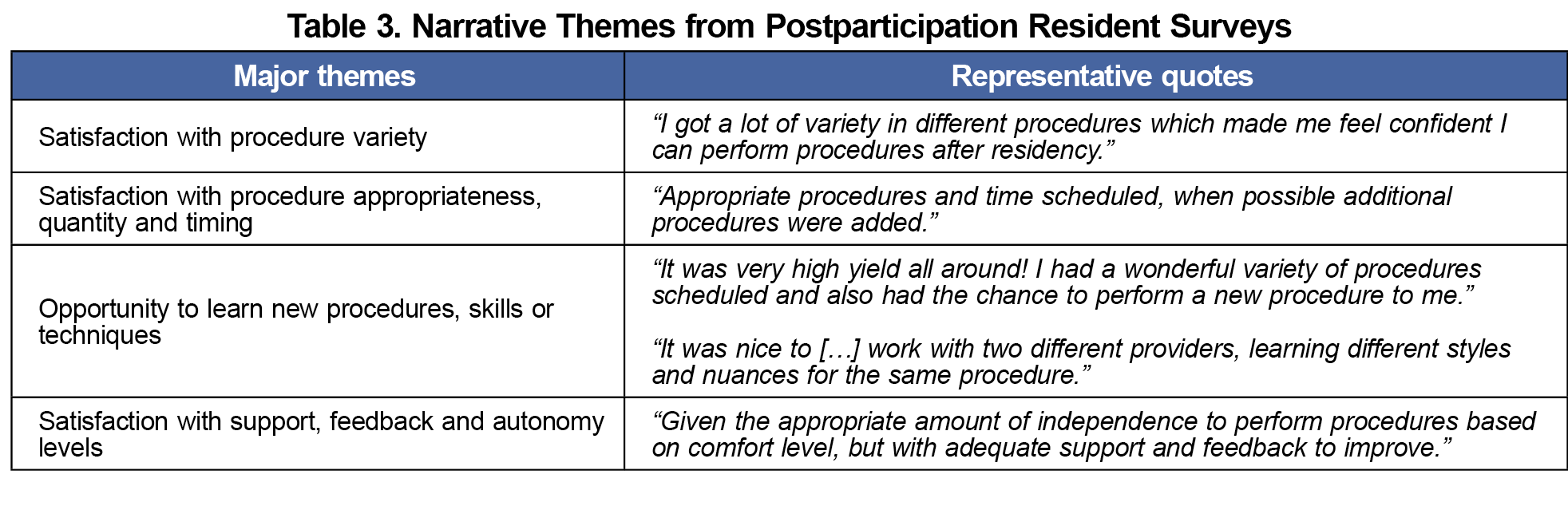
Following each clinic, the participating resident was invited to complete a postparticipation survey assessing perceptions of the clinic experience. Narrative comments from postparticipation surveys were compiled and separately evaluated by each author for major and recurring themes. These themes were reconciled among the authors to determine most common recurring themes.17
We obtained quantitative procedure data using retrospective chart review. We catalogued number and type of procedure for each clinic from April 2020 to April 2021. Procedure types performed in high volume (eg, cautery, cryosurgery, shave procedure, skin tag removal) were capped at a quantity of 10 per procedure clinic in our analysis (with actual range per clinic of 1-26, with one clinic recording an outlier of 100 skin tag removals). Although consensus recommendations give guidance as to minimum numbers for these procedures,3 specific targets for achieving comfort and competence are lacking. Based on our judgement and in consultation with four additional family medicine faculty, we concluded that 10 of each of these simple procedures would conservatively provide enough experience for any participating resident to achieve comfort. We deduced that including every individual instance of these high-volume procedures would inflate procedure numbers without adding additional meaning to the data.
The Providence St. Joseph Institutional Review Board determined that this study protocol did not constitute human subjects research.
Fifteen residents participated in 21 procedure clinics. The majority were third-year residents (n=11, 73.3%), with equal representation of first- (n=2, 13.3%) and second- (n=2, 13.3%) year residents. Five residents participated in more than one clinic. Each clinic saw an average of 5.1 procedural patients (108 patients during study duration). Eighteen procedure types and 268 procedures were performed (Table 1), with a mean of 5.3 procedure types each clinic. Each resident performed an average of 12.8 procedures per clinic, with a range from 3-29 (in some cases, multiple procedures were performed on single patients). More than 50% of residents (N=15) obtained experience with skin lesion excision (53.3%), nail removal (53.3%), punch and shave procedures (73.3% and 66.7%, respectively), joint injection (53.3%), newborn circumcision (53.3%), and implantable contraception management (60.0%).
Most residents agreed with queried educational benefits (Table 2). Narrative comments expressed satisfaction with procedure variety, opportunities to learn new techniques, and feedback received (Table 3). One critique recommended improved preclinic communication between community site and participating resident to better prepare for sessions.
Community procedure clinics supervised by nonfaculty physicians enhanced resident education by providing additional office-based procedures recommended for family medicine ambulatory practice.1,3 Residents regarded the clinics as useful for skill, comfort, and knowledge acquisition. The level of teaching and supervision was viewed favorably. Over 80% of residents said the clinics provided procedures that were limited in their residency, thus helping to potentially fill gaps in their procedural training. This small study suggests that community-academic collaborations are a feasible model to outsource procedural training, an approach that has been suggested for settings with limited training resources.1
One barrier to implementation might be concerns for maintaining nonfaculty attending physician productivity when training learners.18 Although we were not able to adequately study impact on attending productivity due to our sample size, information from our two community attending physicians suggested no adverse impact on productivity. This should be formally measured in future studies to provide a more complete assessment of value for nonresidency primary care procedure clinics.
Other limitations include retrospective study design, small study size, and single site setting. Moreover, our study attendings had an interest in teaching and procedural care. To improve generalizability, additional studies should focus on a similar training model implemented with increased clinic frequency, a wider training network, or additional primary care specialties. In determining acceptability of these procedure clinics, our study primarily relied on resident perception of their experiences in the clinics. Having a comparator group to assess the magnitude of impact of the clinics would have been helpful. Furthermore, future studies should evaluate the effect of such clinics on specific procedural competence attainment or readiness for future practice.
Procedure clinics in a nonresidency site hosted by nonfaculty attending physicians are a feasible way to enhance resident training and to fill potential training gaps in procedures that are common to primary care office-based practice. We hope these findings can assist residency programs in their procedural training curricula.
References
- Nothnagle M, Sicilia JM, Forman S, et al; STFM Group on Hospital Medicine and Procedural Training. Required procedural training in family medicine residency: a consensus statement. Fam Med. 2008;40(4):248-252.
- ACGME Program Requirements for Graduate Medical Education in Family Medicine. Accessed November 14, 2021. https://www.acgme.org/globalassets/PFAssets/ProgramRequirements/120_FamilyMedicine_2020.pdf.
- CAFM Consensus Statement for Procedural Training in Family Medicine Residency. Accessed November 14, 2021. https://www.afmrd.org/page/cafm.
- Ludden-Schlatter A, Wells J, Kruse RL. Perspectives on procedure importance: residents, faculty, and community practitioners. Fam Med. 2018;50(6):450-454. doi:10.22454/FamMed.2018.779054
- Rivet C, Ryan B, Stewart M. Hands on: is there an association between doing procedures and job satisfaction? Can Fam Physician. 2007;53(1):92-93.
- Zomahoun HTV, Samson I, Sawadogo J, et al. Effects of the scope of practice on family physicians: a systematic review. BMC Fam Pract. 2021;22(1):12. doi:10.1186/s12875-020-01328-1
- Sinsky CA, Dugdale DC. Medicare payment for cognitive vs procedural care: minding the gap. JAMA Intern Med. 2013;173(18):1733-1737. doi:10.1001/jamainternmed.2013.9257
- Tucker W, Diaz V, Carek PJ, Geesey ME. Influence of residency training on procedures performed by South Carolina family medicine graduates. Fam Med. 2007;39(10):724-729.
- Poulin EA, Swartz AW, O’Grady JS, Kersten MPM, Angstman KB. Essential office procedures for Medicare patients in primary care: comparison with family medicine residency training. Fam Med. 2019;51(7):574-577. doi:10.22454/FamMed.2019.659478
- Summit AK, Chong E, Gold M. Abortion provision by family physicians after integrated opt-out training in residency. Fam Med. 2023;55(5):317-324. doi:10.22454/FamMed.2023.526561
- Mischell S, Cabrera K, Acosta T, Levine JP, Sliwowska A, Amico J. Barriers to and facilitators of contraceptive implant training in New Jersey family medicine residencies: a qualitative study. Fam Med. 2023;55(10):660-666. doi:10.22454/FamMed.2023.694219
- Schubert FD, Herbitter C, Fletcher J, Gold M. IUD knowledge and experience among family medicine residents. Fam Med. 2015;47(6):474-477.
- Langner S, Deffenbacher B, Nagle J, Khodaee M. Barriers and methods to improve office-based procedural training in a family medicine residency. Int J Med Educ. 2016;7:158-159. doi:10.5116/ijme.573a.364c
- Firnhaber J, Kolasa K. A pilot study of training family medicine residents in procedural skills at a community health center. Fam Med. 2012;44(3):202-204.
- Sy J, Bloom J, Mizdrak N, Moaveni A, Toubassi D. Procedural skills training during residency: introduction of a procedure clinic to improve technical competencies. Can Fam Physician. 2023;69(4):292-294. doi:10.46747/cfp.6904292
- Khera KD, Boswell CL. Utilizing a referral-based procedure clinic rotation in family medicine residency. PRiMER Peer-Rev Rep Med Educ Res. 2022;6:19. doi:10.22454/PRiMER.2022.962965
- de la Cruz MS, Kopec MT, Wimsatt LA. Resident perceptions of giving and receiving peer-to-peer feedback. J Grad Med Educ. 2015;7(2):208-213. doi:10.4300/JGME-D-14-00388.1
- Latessa R, Beaty N, Colvin G, Landis S, Janes C. Family medicine community preceptors: different from other physician specialties? Fam Med. 2008;40(2):96-101.



There are no comments for this article.