Background and Objectives: The COVID-19 pandemic worsened the shortage of clinical training opportunities for health professions learners. During the pandemic, additional barriers to precepting health professions learners emerged. Understanding preceptors’ perceptions of barriers is a first step to providing learners with the best clinical learning opportunities.
Methods: In February 2021, the Emory Primary Care Consortium surveyed primary care providers eligible to precept health professions learners to determine their current precepting status and associated barriers encountered during and since COVID-19.
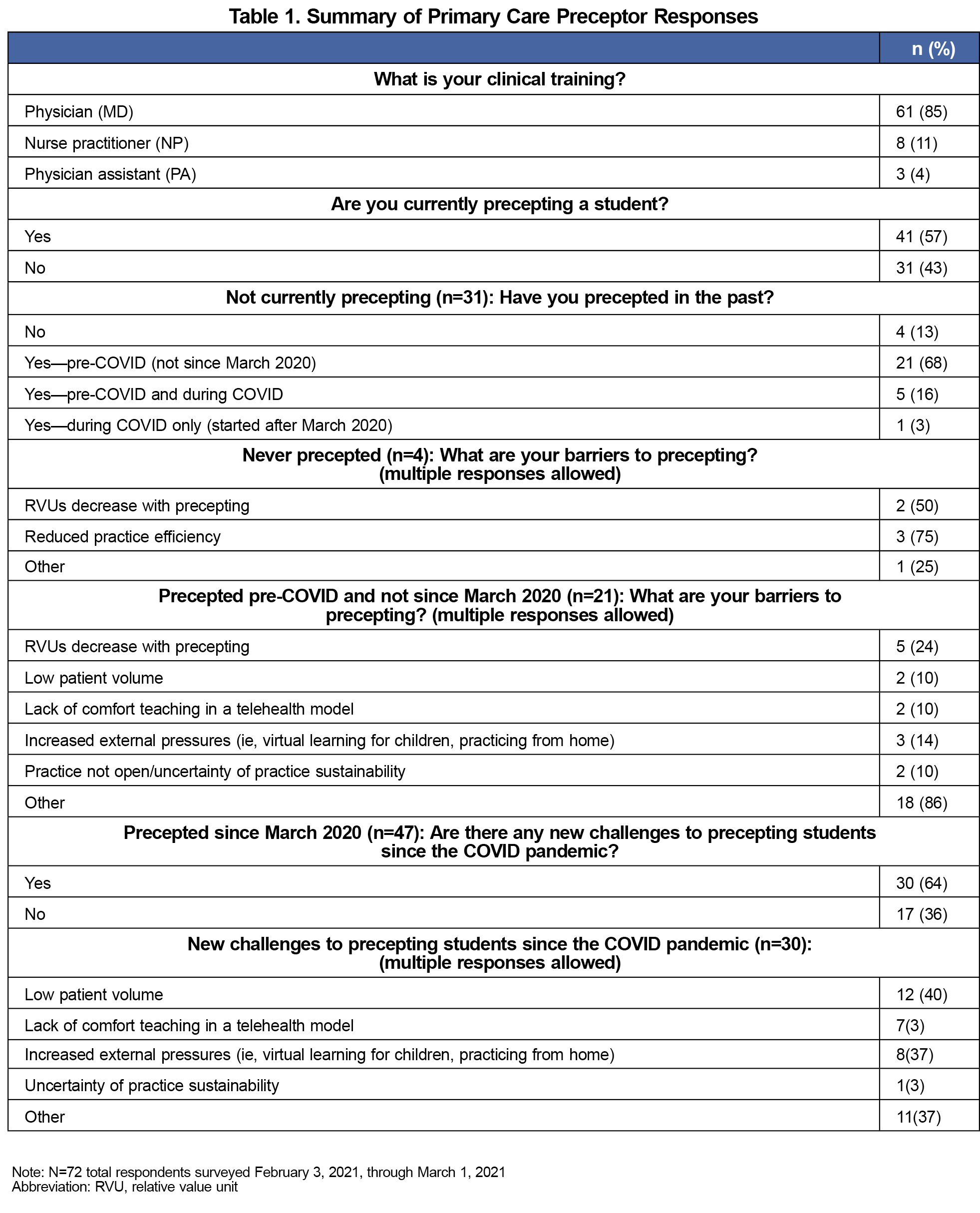
Results: A total of 61 physicians and 11 nurse practitioners (NPs) or physician assistants (PAs) completed the survey. Of the 41 current preceptors, 29 precepted only MD students, 2 MD and PA students, 7 NP students only, and 3 PA students only. Of the 31 respondents who were not precepting, most (21) had precepted before March 2020 and not since. Pandemic-related precepting challenges included low patient volume (12), lack of comfort teaching in a telehealth setting (7), increased external pressure (eg, children at home; 8), and other reasons (12). Overall, 20 respondents were interested in training on incorporating students into the telehealth clinical workflow and 13 in training on teaching and providing feedback remotely.
Conclusion: The COVID-19 pandemic placed additional burdens on preceptors in primary care. Preceptors could benefit from training on incorporating students into telehealth visits. Increased understanding of preceptor needs could lead to new resource offerings and improved future medical education.
Experiential clinical training is recognized as essential to learning the critical thinking skills1 necessary to produce competent providers.2 However, primary care has faced a shortage of clinical preceptors3 because providers have perceived negative impacts to productivity, including low patient flow,4,5 reduced income and increased working hours,6 increasing workload expectations, and self-perceived lack of qualification.7,8 The COVID-19 pandemic exacerbated these challenges, affecting experiential learning for health professions trainees.9–11
Many medical practices stopped accepting students into their facilities, shifted in-person care to telemedicine,9 and saw temporary decreases in volumes. Virtual care drawbacks from a learning perspective included reduced student engagement and loss of assessment.2 Although early evidence has shown that preceptors believe they can deliver high-quality instruction in virtual environments;12,13 students are dissatisfied with virtual clinical learning.14
In response to the pandemic, Emory Healthcare restricted clinical rotations from March through May 2020 and implemented mandatory vaccination for all employees and students in fall 2021. In fall 2020, Emory University’s doctor of medicine (MD), physician assistant (PA), and nurse practitioner (NP) primary care clerkship programs faced increased challenges in recruiting and retaining preceptors. Thus, the Emory Primary Care Consortium (EPCC), a collaborative group of family medicine (FM), general internal medicine (GIM), and geriatrics providers, undertook an investigation of their preceptors’ barriers. The EPCC found scant peer-reviewed literature describing actionable barriers faced by preceptors of health professions trainees. Thus, the objective of this study was to characterize the general and new pandemic-related barriers to precepting health professions learners.
Qualtrics was used to survey primary care providers eligible to precept health professions learners (PA, NP, and MD) to determine their current precepting status, their barriers to precepting, and whether they would be interested in receiving training materials to assist in incorporating learners in telehealth visits.
For initial content validity,15 the EPCC members (including precepting Emory faculty, and clerkship and residency directors) compiled a list of barriers they expected to resonate with preceptors. These barriers formed a nine-question, 5-minute, nonincentivized multiple-choice survey. For face validity,15 the survey was pilot tested for usability and readability in January 2021 by FM and GIM residency preceptors and fielded from February 3, 2021 through March 1, 2021.16 The pilot testing resulted in minor edits to the wording of the barriers presented and the addition of two barriers. The survey invitation and reminder at 2 weeks were emailed to approximately 450 primary care providers via a physician listserv, NP and PA program community preceptor lists, and internal social media pages. We used Stata (StataCorp LLC) to compute descriptive statistics of our results. The Emory Institutional Review Board determined this was not human subject research.
Of 72 survey respondents (16% response rate), 61 were physicians and 11 were NPs or PAs (Table 1). Overall, 41 respondents were currently precepting students: 29 precepted only MD students, 2 MD and PA students, 7 NP students only, and 3 PA students only. Of the remaining 31 respondents who were not precepting students at the time of the survey, 4 had never precepted, 21 had precepted before March 2020 and not since, 5 precepted both pre- and during COVID but not at the time of the survey, and 1 had begun precepting after March 2020.
Of the 21 respondents with precepting experience who had not resumed precepting since March 2020, 5 reported barriers to precepting of productivity decreases, 2 low patient volume, 2 lack of comfort teaching virtually, 3 increased external pressures, 2 practice not open/uncertainty of practice sustainability, and 18 other. Those who responded “other” reported their barriers as preparing for retirement, pressure to maintain clinical volume, decrease in clinical time, high COVID rates in their facility, increased demand for resident rotations, reduced time for students, inconsistent scheduling, lack of staffing, and physical distancing/spacing issues.
Of the 30 respondents reporting challenges to precepting that started with the COVID pandemic, low patient volume was cited by 12 respondents, lack of comfort teaching in a telehealth setting by 7, increased external pressures by 8, uncertainty of practice sustainability by 1, and other reasons by 11. The “other” barriers identified included inconsistent clinical schedules, students’ lack of physical exam skills due to lack of in-person experiences, increased workload, patients being more complicated post-COVID, fewer in-person patients, the need to provide personal protection equipment (PPE) for students, social distancing requirements, and workspace availability.
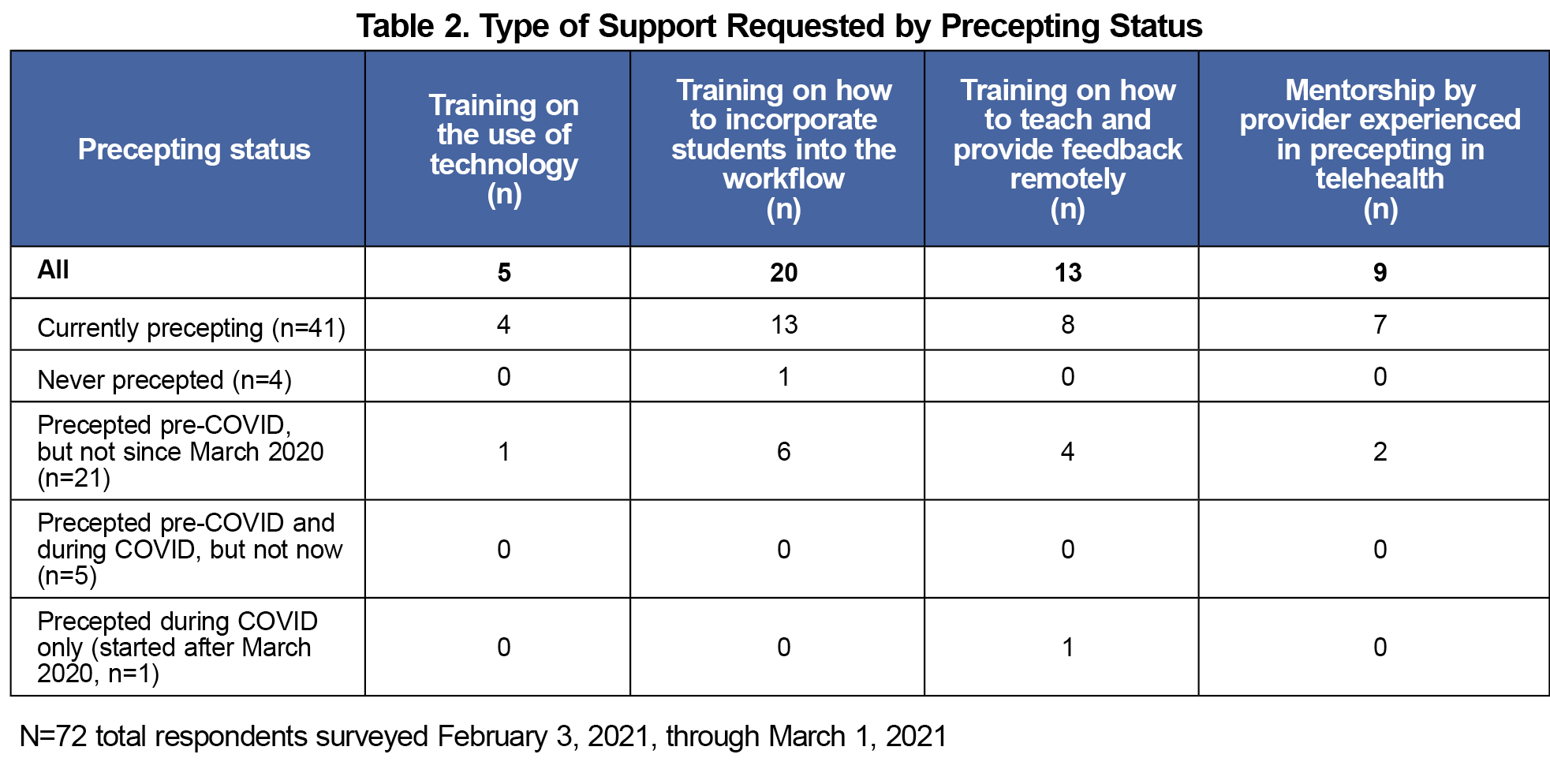
Overall, 20 respondents were interested in receiving training on how to incorporate students into the telehealth clinical workflow (Table 2), 13 in training on how to teach and provide feedback remotely, 9 in mentorship by providers experienced in precepting in telehealth, and 5 in training on the use of telehealth.
The COVID-19 pandemic placed additional burdens on preceptors due to uncertainties associated with telehealth, PPE supply, and viability of the practice. Based on our survey results, Emory provided training for preceptors on how to incorporate students into virtual visits and provided student training on virtual visits and virtual physical exams. Emory also designed preceptor and medical learner workflows to help increase preceptor efficiency and enable preceptors and students to evaluate the patient together.
Limitations
The survey was fielded at a single health system. Thus, results might not be generalizable across the United States. Also, the level of nonresponse bias was not assessed, and recall bias might have led to reporting immediate barriers instead of barriers related to COVID-19. Additionally, although the response rate of 16% was low, our survey was not incentivized, was fielded during a pandemic, and eligible respondents were volunteers. Therefore, our response rate is realistic for this real-world setting of unpaid work.17 Further, because this was a one-time survey, we were unable to conduct reliability tests of our results.15
A structured approach to address the needs of preceptors would allow a tailored response. This approach could entail ensuring that the skills of learners included use of telehealth, offering proactive educational sessions for preceptors on teaching in a telehealth environment, and developing strategies to improve efficiency and workflow with learners. Broadly sharing examples of how to best incorporate learners may help to address preceptors’ concerns.
Acknowledgments
The authors thank the Emory Primary Care Consortium for providing the survey data.
Presentations: Lund MB, Green S, Leppke A, Vohra-Khullar P, Alfonso S, Moore MA. Significant primary care preceptor shortage remains one year after the pandemic started. Poster Presentation at the Society of Teachers of Family Medicine Annual Spring Conference, Indianapolis, IN, May 1-4, 2022.
Funding: Miranda A. Moore received funding from the Agency for Healthcare Research and Quality (AHRQ), Health Resources and Services Administration (HRSA), Ardmore Institute of Health, Morehouse School of Medicine, and the Alzheimer’s Association.
References
- Sultan AS. Bedside teaching: an indispensible tool for enhancing the clinical skills of undergraduate medical students. J Pak Med Assoc. 2019;69(2):235-240.
- Wilcha RJ. Effectiveness of virtual medical teaching during the COVID-19 crisis: systematic review. JMIR Med Educ. 2020;6(2):e20963. doi:10.2196/20963
- Doherty CL, Fogg L, Bigley MB, Todd B, O’Sullivan AL. Nurse practitioner student clinical placement processes: a national survey of nurse practitioner programs. Nurs Outlook. 2020;68(1):55-61. doi:10.1016/j.outlook.2019.07.005
- Boyce DJ, Shifrin MM, Moses SR, Moss CR. Perceptions of motivating factors and barriers to precepting. J Am Assoc Nurse Pract. 2022;34(11):1,225-1,234. doi:10.1097/JXX.0000000000000788
- Bernstein J, Maatman T, Kaljo K. Leadership views on the barriers and incentives to clinical preceptorship. WMJ. 2021;120(1):23-28.
- Krehnbrink M, Patel K, Byerley J, et al. Physician preceptor satisfaction and productivity across curricula: a comparison between longitudinal integrated clerkships and traditional block rotations. Teach Learn Med. 2020;32(2):176-183. doi:10.1080/10401334.2019.1687304
- Matua GA, Seshan V, Savithri R, Fronda DC. Challenges and strategies for building and maintaining effective preceptor-preceptee relationships among nurses. Sultan Qaboos Univ Med J. 2014;14(4):e530-e536.
- Minor S, Huffman M, Lewis PR, Kost A, Prunuske J. Community preceptor perspectives on recruitment and retention: the CoPPRR study. Fam Med. 2019;51(5):389-398. doi:10.22454/FamMed.2019.937544
- Fuller KA, Heldenbrand SD, Smith MD, Malcom DR. A paradigm shift in US experiential pharmacy education accelerated by the COVID-19 pandemic. Am J Pharm Educ. 2020;84(6):ajpe8149. doi:10.5688/ajpe8149
- Courtier N, Brown P, Mundy L, Pope E, Chivers E, Williamson K. Expectations of therapeutic radiography students in Wales about transitioning to practice during the COVID-19 pandemic as registrants on the HCPC temporary register. Radiography (Lond). 2021;27(2):316-321. doi:10.1016/j.radi.2020.09.001
- Hueston WJ, Petty EM. The impact of the COVID-19 pandemic on medical student education in Wisconsin. WMJ. 2020;119(2):80-82.
- Grand D, Schuster VL, Pullman JM, Golestaneh L, Raff AC. Medical student experience and outcomes, as well as preceptor experience, with rapid conversion of a preclinical medical school course to a remote-based learning format in the setting of the COVID-19 pandemic. Med Sci Educ. 2021;31(6):1,895-1,901. doi:10.1007/s40670-021-01379-8
- Kang-Birken SL, Law EJ, Moon YSK, Lee AJ, Haydon AL, Shek A. Assessing preceptor and student perceptions of remote advanced pharmacy practice experience learning during the COVID-19 pandemic. Pharmacy (Basel). 2022;10(5):103. doi:10.3390/pharmacy10050103
- Dutta S, Ambwani S, Lal H, et al. The satisfaction level of undergraduate medical and nursing students regarding distant preclinical and clinical teaching amidst COVID-19 across India. Adv Med Educ Pract. 2021;12:113-122. doi:10.2147/AMEP.S290142
- Cobern W, Adams B. Establishing survey validity: A practical guide. Int J Assess Tools Educ. 2020;7(3):404-419. doi:10.21449/ijate.781366
- Lund MB, Green S, Leppke A, Vohra-Khullar P, Alfonso S, Moore MA. Barriers to precepting health professions learners survey. STFM Resource Library. Society of Teachers of Family Medicine; 2023.
- Barnhart BJ, Reddy SG, Arnold GK. Remind me again: Physician response to web surveys: The effect of email reminders across 11 opinion survey efforts at the American Board of Internal Medicine from 2017 to 2019. Eval Health Prof. 2021;44(3):245-259. doi:10.1177/01632787211019445



There are no comments for this article.