In academic settings, different methods have been used to assess student progress, confidence, and knowledge in particular subjects. In multiple studies, self-assessed confidence is utilized as a method to measure student knowledge. Although some studies have found confidence levels to be uncorrelated to student knowledge, researchers continue to use self-assessed confidence as a measure of knowledge. There has been evidence in the literature to support the absence of a correlation between confidence and knowledge as students tend to overestimate or underestimate their confidence.1–4 Much of that research is conducted in a population of nursing students or residents. It is imperative that future health care providers are knowledgeable and confident in their abilities to diagnose and treat common illnesses, one of those being diabetes. In this study, we assessed the correlation between confidence and knowledge levels in fourth-year medical students at a United States medical school on the topic of diabetes management. Results will provide insight into whether or not the confidence medical students have in managing diabetes matches their actual diabetes-related knowledge.
LEARNER RESEARCH
US Fourth-Year Medical Students: Diabetes Knowledge and Confidence Dissonance
Danielle Pitter, BS | Alyssa M. Indelicato, BA | Christopher P. Morley, PhD | Barbara Feuerstein, MD, PhD | Ruth S. Weinstock, MD, PhD
PRiMER. 2024;8:4.
Published: 1/23/2024 | DOI: 10.22454/PRiMER.2024.497586
Introduction: Self-assessed confidence is not a reliable indicator of knowledge levels, as multiple studies have shown; however, it is often used as a measure of knowledge. The purpose of this study is to identify whether the confidence of graduating students in a US medical school to diagnose and treat diabetes is correlated with their diabetes-related knowledge.
Methods: We developed a 38-question survey, targeting students’ external experiences, knowledge, and confidence related to the diagnosis, treatment, and prevention of diabetes. The survey includes six self-reported confidence questions and 15 multiple choice-style questions, to test diabetes knowledge. The survey was administered electronically using REDCap to the graduating medical school class (n=176) at Upstate Medical University. We calculated mean knowledge scores and confidence scores were calculated. We used Pearson correlation and t tests to assess for correlations and differences in the collected data. We also reviewed diabetes content in the current curriculum.
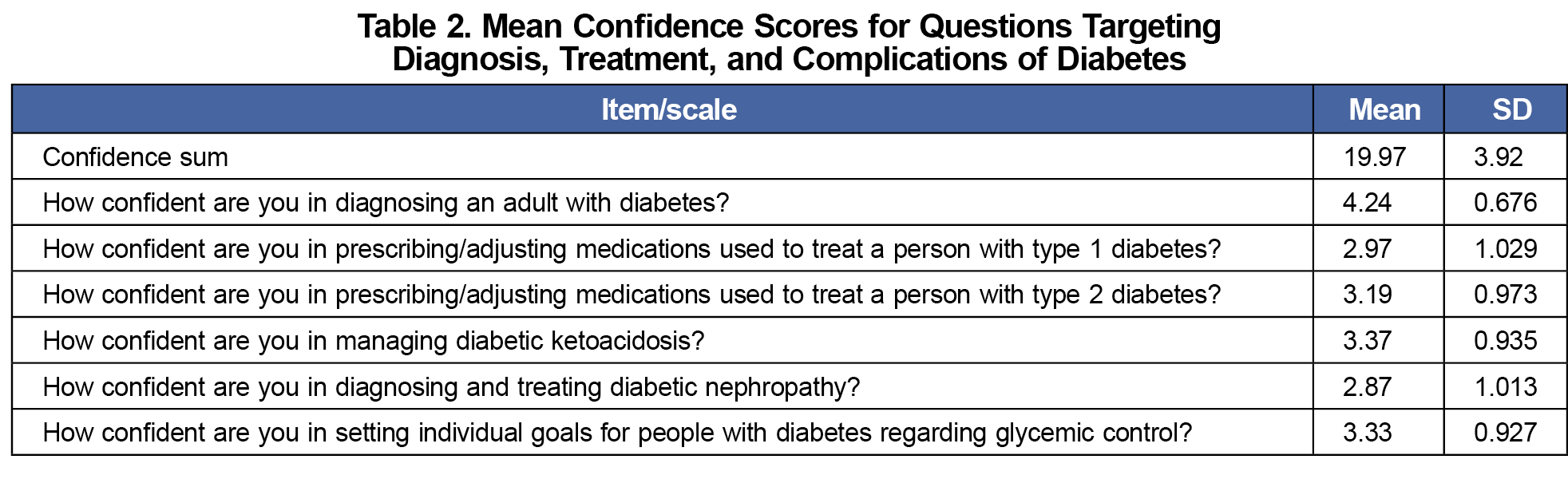
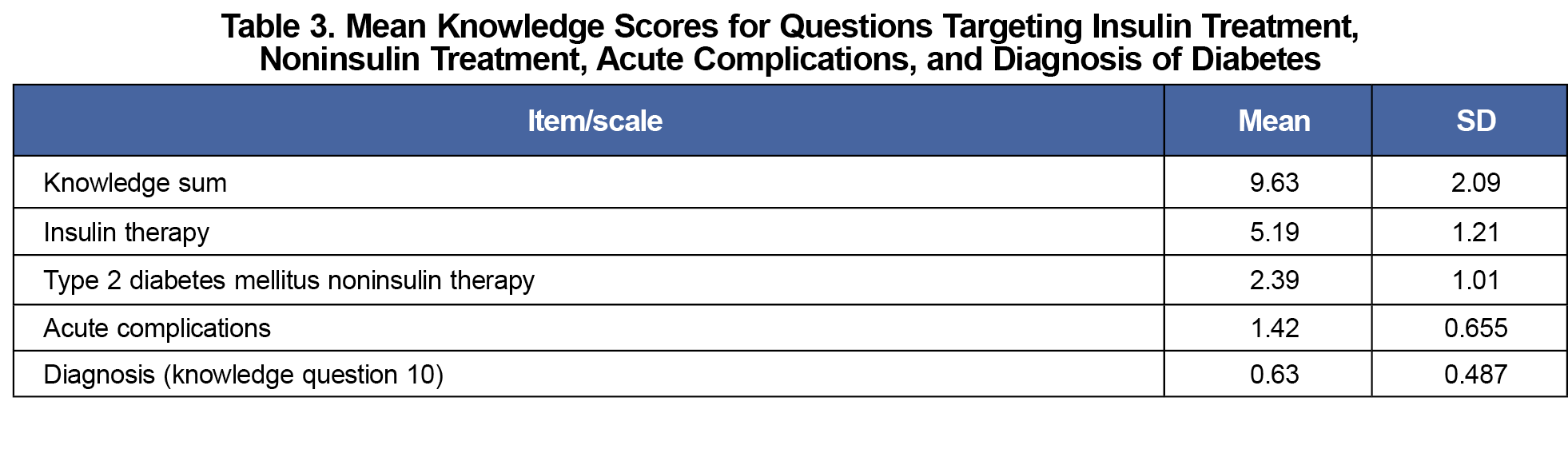
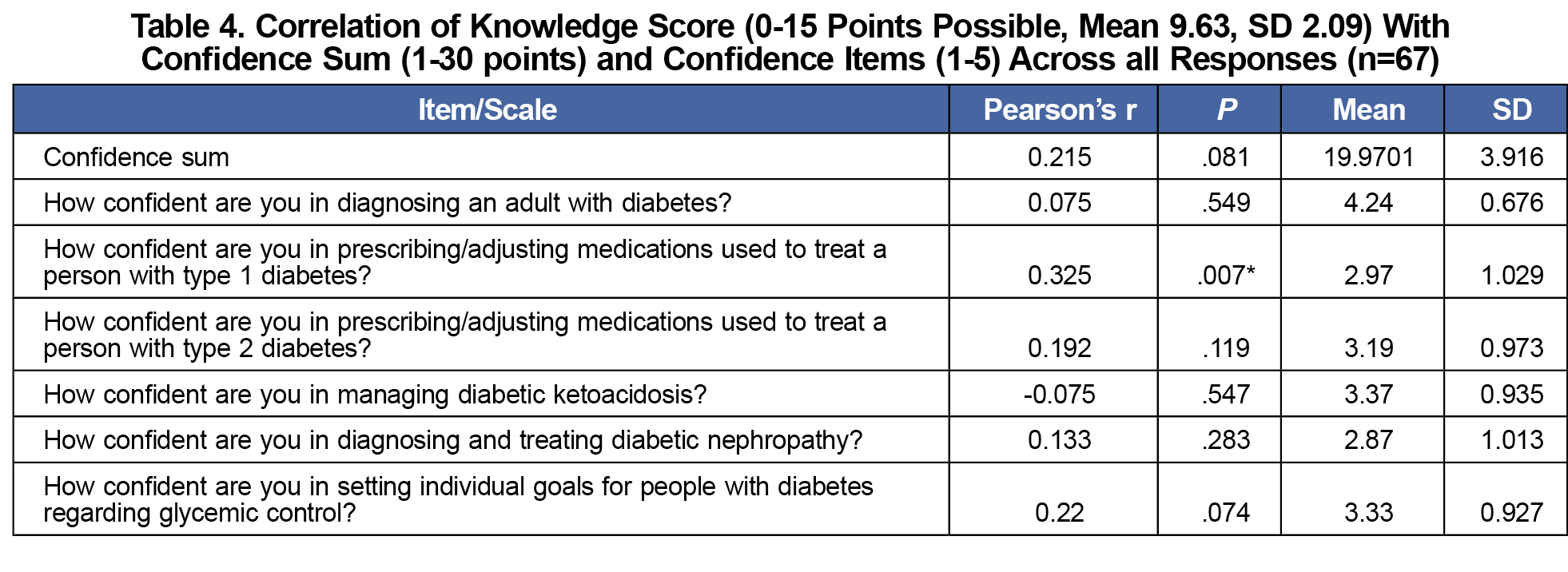
Results: The response rate was 38%. The mean confidence score was 19.97 out of 30 (SD=3.92) and the mean knowledge score was 9.63 out of 15 (SD=2.09). Total knowledge and confidence scores were not correlated. A positive correlation between confidence in prescribing/adjusting medications to treat patients with type 1 diabetes and knowledge levels was found (R=.325, P=.007). Academic electives, external experiences with diabetes, and demographics did not correlate with knowledge and confidence differences.
Conclusions: Students overestimated their ability to adequately manage people with diabetes. Better approaches are needed to prepare future physicians to diagnose and treat diabetes.
We conducted this cross-sectional, observational study at a 4-year allopathic medical school in the northeastern region of the United States, using a questionnaire developed by applying de novo questions and questions from previously published validated questionnaires on diabetes.5–7 The questions collected demographic data, student feedback about learning experiences, and information about external experiences. The questions included six self-reported items regarding confidence, as well as 15 multiple-choice, quiz-style questions testing knowledge related to the topic of diabetes. A copy of the survey items is available in the STFM Resource Library.8 We also recorded teaching methods and settings (eg, lectures, clinical experience with people with diabetes). We implemented the survey via the REDCap system and distributed it electronically to all graduating medical students (n=176) at Upstate Medical University in March 2023. Responses were confidential and data de-identified. The Institutional Review for the Protection of Human Subjects at SUNY Upstate Medical University determined that this project was exempt from review.
For knowledge questions, each correct answer was awarded 1 point. The total possible score for the knowledge section ranged from 0-15. The confidence questions were Likert-scaled from 0 (not confident) to 5 (confident). The total possible score for the confidence section ranged from 0-30. We calculated the average knowledge and confidence score along with the standard deviations. The percentage of each response was reported for each question. Scores were also totaled with one point for each yes answer. Questions pertaining to previous experiences, electives, and learning opportunities related to diabetes were formulated as yes/no (1/0) questions.
We calculated mean knowledge and mean confidence scores using the summed totals for each student. We calculated pearson correlation coefficients to assess the correlation between confidence levels and the number of correct answers to knowledge questions. We also assessed knowledge scores and individual confidence items in this manner. We used t tests to assess the differences in the confidence and knowledge scores, individually, with their demographics, each yes/no experience question, and future specialty. All analyses were conducted in SPSS v.28.
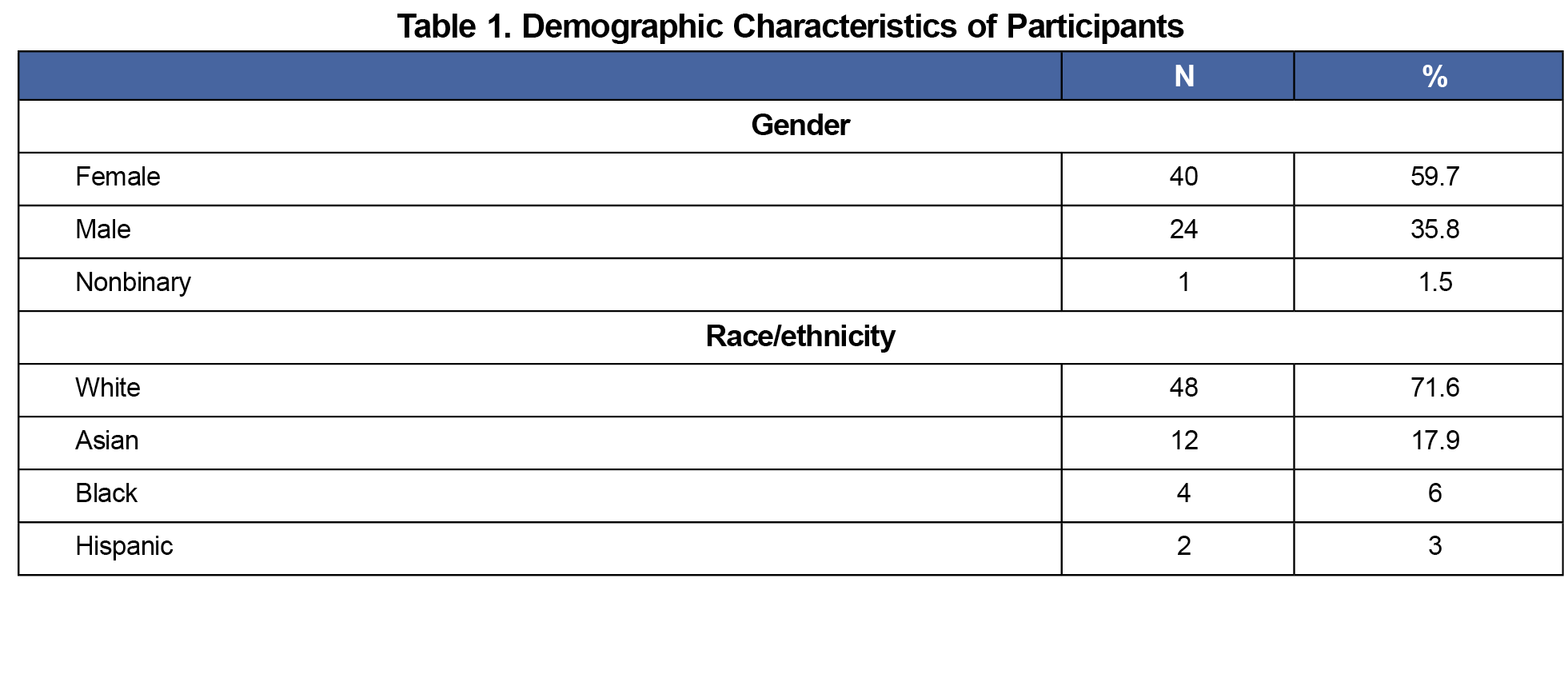
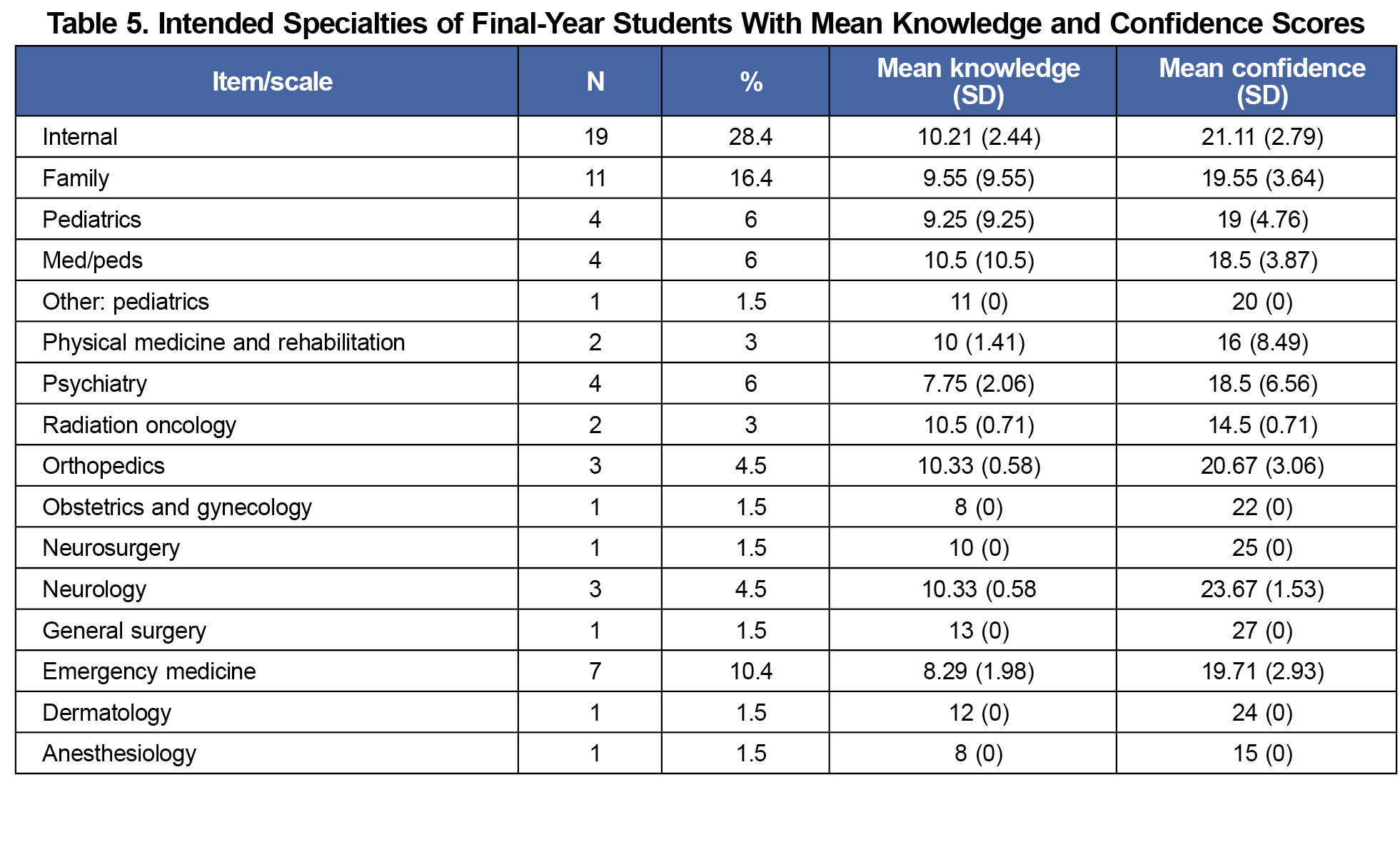
The student questionnaire response rate was 38% (n=67). The respondents were about 36% male, 60% female, 2% nonbinary, 72% White, 18% Asian, 6% Black, and 3% Hispanic (Table 1). The highest percentage of students matched into internal (28.4%), family (16.4%), and emergency (10.4%) medicine. The respondents were representative of the class as whole, both in terms of demographic distribution and specialty preference. Additional characteristics were collected but the small sample size limited analyses. The overall mean confidence score was 19.97 out of 30 (SD=3.92; Table 2). The overall mean knowledge score was 9.63 out of 15 (SD=2.09; Table 3). We observed no correlation between overall knowledge and confidence levels (R=.215, P=.081), and only one individual confidence item, prescribing/adjusting medications to treat a patient with type 1 diabetes, was correlated with knowledge scores (R=.325, P=.007), out of six items (Table 4). The highest mean confidence levels were noted among students entering general surgery, scoring 27 out of 30 (SD=0) and neurosurgery, scoring 25 out of 30 (SD=0). The highest mean knowledge levels were noted among students entering general surgery, scoring 13 out of 15 (SD=0) and dermatology, scoring 12 out of 15 (SD=0; Table 5).
The results of this study add further evidence that self-assessed confidence levels of fourth-year medical students are poorly correlated with knowledge and extends that evidence to knowledge and confidence regarding the management of type 1 diabetes. These findings are important, as they offer additional evidence as to why self-assessed confidence should not be utilized as a proxy for knowledge. The use of self-assessed confidence to measure knowledge levels should be de-emphasized when conducting studies on student subject knowledge. A more effective way to measure student knowledge may be to assess their scores on knowledge-based questions. These results will help inform curriculum change and methods of assessing knowledge. By knowing exactly what diabetes knowledge students lack, curricula can be adjusted to incorporate more teaching time targeting those areas.
One limitation of this study is that the data collected are the first collection of diabetes knowledge versus confidence data for medical students at the host institution. No other time series data were available for review or comparison. This study would need to be continued over time to assess trends. A second limitation is that this study included one public-supported US medical school, and the data cannot be generalized to other institutions with differing curricula in other regions in the United States. A third limitation of this study was that with a response rate of 38%, we were unable to run the results using the multivariable regression, as it risked the chance of overspecification.
In conclusion, self-assessed confidence by medical students is not a sufficient indicator of their knowledge levels in managing people with diabetes. As these final-year students are possibly entering residency with more confidence than knowledge, this phenomenon needs to be addressed to ensure that their future patients will receive proper care. Future research, involving more institutions and a larger sample size, is needed to confirm these findings.
References
- Parker RW, Alford C, Passmore C. Can family medicine residents predict their performance on the in-training examination? Fam Med. 2004;36(10):705-709.
- Lerner BS, Kalish V, Ledford CJW. Exploring Residents’ Skills in Diagnosing Dementia: The Unexpected Dissonance Between Ability and Confidence. Fam Med. 2017;49(6):460-463.
- Jones R, Panda M, Desbiens N. Internal medicine residents do not accurately assess their medical knowledge. Adv Health Sci Educ Theory Pract. 2008;13(4):463-468. doi:10.1007/s10459-007-9058-2
- Sodha M, McLaughlin M, Williams G, Dhillon S. Nurses’ confidence and pharmacological knowledge: a study. Br J Community Nurs. 2002;7(6):309-315. doi:10.12968/bjcn.2002.7.6.10476
- George JT, McGrane DJ, Warriner D, et al; TOPDOC Study Team. Protocol for a national audit on self-reported confidence levels, training requirements and current practice among trainee doctors in the UK: the Trainees Own Perception of Delivery of Care in Diabetes (TOPDOC) Study. BMC Med Educ. 2010;10(1):54. doi:10.1186/1472-6920-10-54
- Rubin DJ, Moshang J, Jabbour SA. Diabetes knowledge: are resident physicians and nurses adequately prepared to manage diabetes? Endocr Pract. 2007;13(1):17-21. doi:10.4158/EP.13.1.17
- Derr RL, Sivanandy MS, Bronich-Hall L, Rodriguez A. Insulin-Related Knowledge Among Health Care Professionals in Internal Medicine. Diabetes Spectr. 2007;20(3):177-185. doi:10.2337/diaspect.20.3.177
- Pitter D. Final Year Medical Student Diabetes Questionnaire. STFM Resource Library. Accessed December 15th, 2023. https://resourcelibrary.stfm.org/viewdocument/final-year-medical-student-diabetes?CommunityKey=2751b51d-483f-45e2-81de-4faced0a290a&tab=librarydocuments
Lead Author
Danielle Pitter, BS
Affiliations: SUNY Upstate Medical University, Syracuse, NY
Co-Authors
Alyssa M. Indelicato, BA - Department of Public Health & Preventive Medicine, SUNY Upstate Medical University, Syracuse, NY
Christopher P. Morley, PhD - Departments of Public Health & Preventive Medicine and Family Medicine, SUNY Upstate Medical University, Syracuse, NY
Barbara Feuerstein, MD, PhD - Department of Medicine, SUNY Upstate Medical University, Syracuse, NY
Ruth S. Weinstock, MD, PhD - Department of Medicine, SUNY Upstate Medical University, Syracuse, NY
Corresponding Author
Danielle Pitter, BS
Correspondence: 500 Harrison St Apt 806A, Syracuse NY 13202. 516-859-6092
Email: pitterd@upstate.edu
Fetching other articles... 
Loading the comment form... 
Submitting your comment... 


There are no comments for this article.