Introduction: Nutrition education remains inadequate in American medical schools, and physicians often cite lack of nutrition knowledge as a barrier to counseling patients. The goal of this study was to evaluate the impact of additional nutrition curriculum on first-year medical students.
Methods: We created a 1-hour nutrition lecture, delivered to first-year medical students. Using pre-, post-, and 3-month follow-up surveys, we assessed the following: (1) change in student knowledge; (2) confidence in counseling patients; (3) motivation to change their personal dietary behaviors; and (4) satisfaction with the curriculum. We assessed objectives using multiple choice questions and 10-point Likert scale questions.
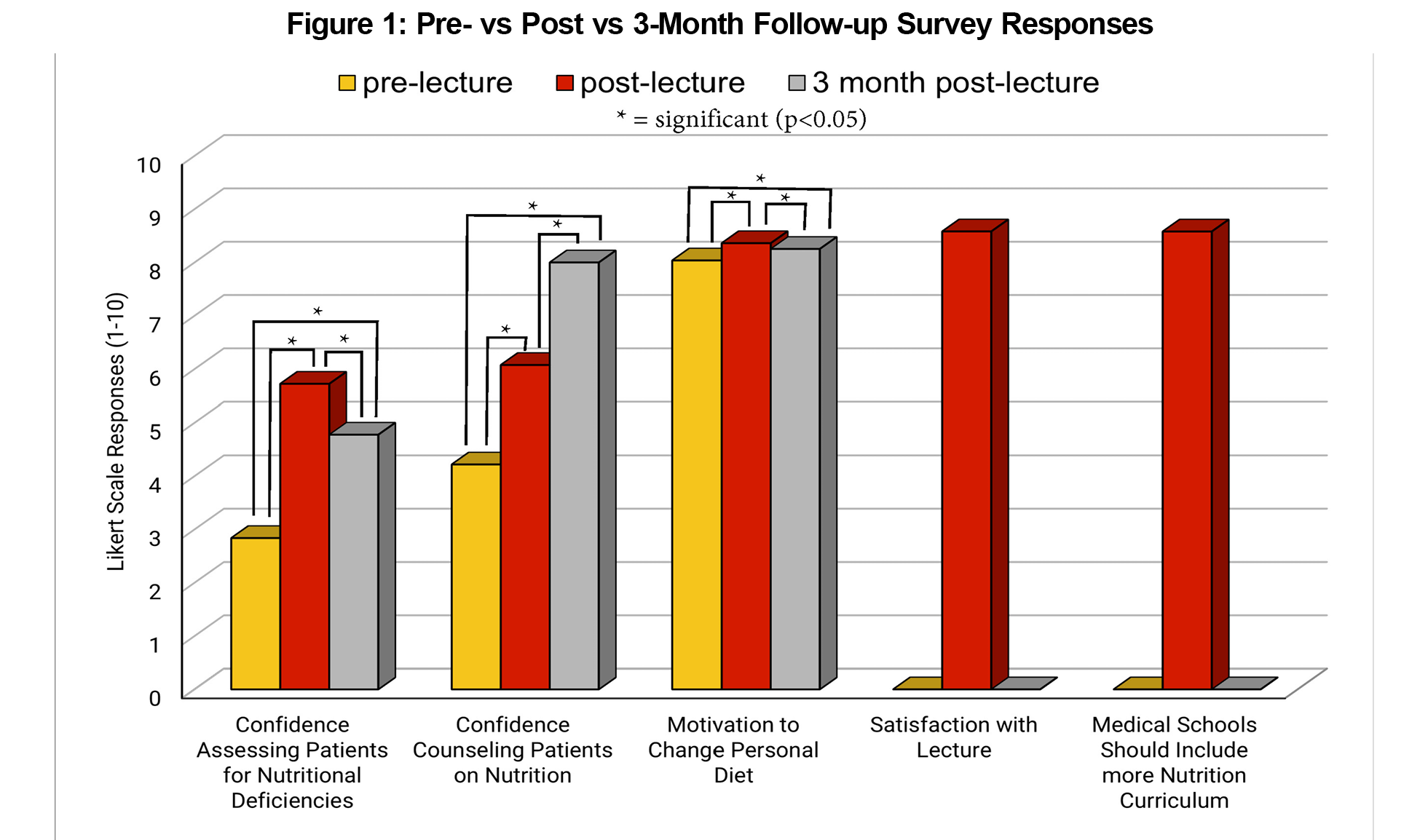
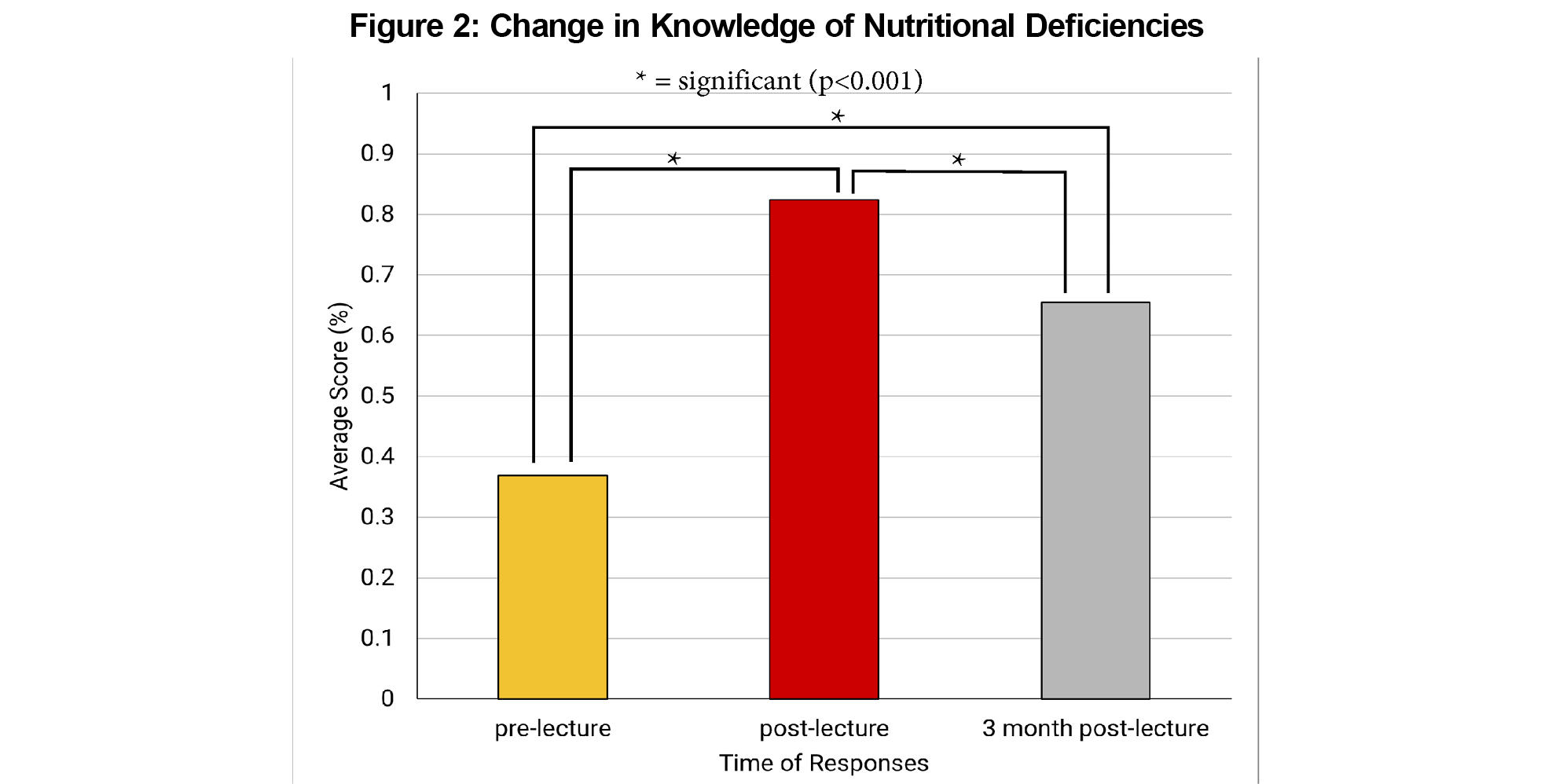
Results: Of the 142 students who attended the live lecture, 105 (73.9%) completed both pre- and postsurveys, and 65 (45.8%) completed the 3-month follow-up survey. Students’ knowledge of the material increased from 37% to 82%, but retention dropped to 65% at the 3-month mark (P<.001). Comfort in assessing and counseling patients improved across the three survey iterations, from 3.53 to 5.90 to 8.00 (P<.001). Motivation to change personal behaviors was high overall at 8.04, 8.36 and 8.25 [P<.05]). Moreover, students were satisfied with the lecture, with a rating of 8.58/10.
Conclusions: This study supports the value of additional medical student nutrition education. This curriculum significantly increases student knowledge, comfort with the material, and confidence in counseling their future patients. A longitudinal curriculum that reinforces concepts over time will help improve long-term retention.
Poor dietary choices are one of the strongest risk factors for death and disability in the United States, leading to conditions such as obesity, type 2 diabetes, and cardiovascular disease.1 These chronic illnesses are preventable, but many adults lack the knowledge to make dietary changes.2,3 The public consistently identifies primary care doctors as the preferred source of nutrition information and counseling.4 However, physicians cite a lack of knowledge as a major barrier to counseling patients on nutrition/disease prevention.5 Additionally, physicians’ personal habits predict how much they will counsel their patients on these topics.6
Nutrition education in American medical schools is inadequate and decreasing.7–9 Furthermore, there is a paucity of literature evaluating the impact of nutrition education among medical students.10,11 Therefore, increasing medical students’ nutrition education may be important to help change this paradigm.
This project was developed to expand the existing Keck School of Medicine of the University of Southern California (KSOM) nutrition curriculum. We created a 1-hour nutrition lecture that was delivered to first-year medical students. The students were surveyed before and after the lecture. This study aimed to assess change in medical students' knowledge and attitudes after receiving an additional nutrition curriculum.
A 1-hour nutrition lecture was delivered, both live and via webcast, to 186 first-year KSOM medical students. Attendance was optional. The lecture overviewed clinically important vitamins and minerals, emphasizing micronutrient deficiencies throughout the life cycle.
Using pre-, post-, and 3-month postsurveys, we assessed the students on the following parameters: (1) change in their knowledge; (2) confidence in counseling patients; (3) change in their own behaviors; and (4) satisfaction with the curriculum. We assessed change in knowledge using multiple choice factual recall questions, and we assessed confidence, behavior, and satisfaction using 10-point Likert scale survey questions. The postsurvey also included two free-response questions. The same survey was given pre, post, and 3 months after the curricular intervention. The survey is available in the STFM Resource Library.12
We used a paired samples t test to compare student responses. We analyzed the free-response questions for common themes using an inductive approach.13 This project was deemed exempt by the University of Southern California’s Institutional Review Board.
One hundred forty-two of 186 students (76%) attended the live lecture. Of the 142 students in attendance, 105 (73.9%) completed both pre/postsurveys, and 65 (45.8%) completed the 3-month follow-up survey. Students improved their knowledge of the material, from an average score of 37% to 82% (P<.001). These scores dropped to 65% at the 3-month mark (P<.001; Figure 1). Student comfort in assessing and counseling patients improved across the three intervals surveyed, from 3.53 to 5.90 to 8.00 on a 10-point Likert scale (P<.001). Students' motivations to change their personal behaviors were high overall, starting at 8.04 (pre) and improving to 8.36 (post) and 8.25 (3-month post) surveys, respectively (P<.05). Moreover, students were satisfied with the lecture (8.58/10). Students also largely agreed that medical schools should include more nutrition curricula (8.58/10; Figure 2).
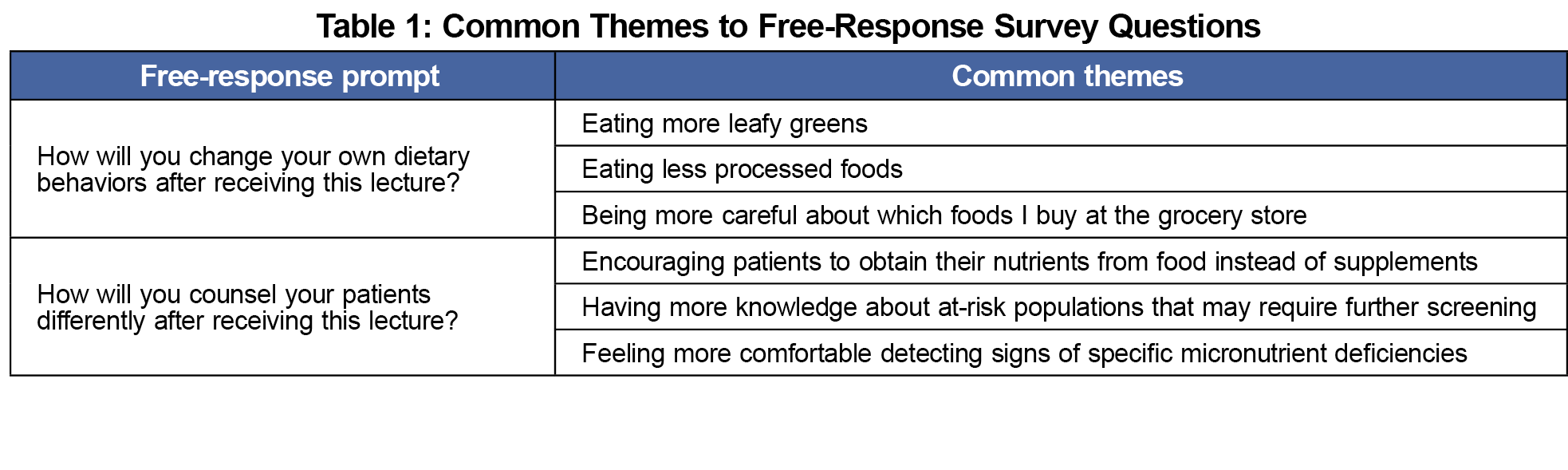
The free-response questions yielded a few common themes, which are represented in Table 1.
This study assessed the impact of additional nutrition curricula among first-year medical students. Our findings support continued and increased preclinical nutrition training as it increases student nutrition knowledge and perceived competence. The most dramatic increase was seen in nutrition knowledge, highlighting these medical students' knowledge gap before the lecture. However, knowledge retention decreased at the 3-month mark, reflecting the need for a longitudinal curriculum that provides repeated exposure to these concepts.
Generally, medical students show a high level of interest in nutrition education and believe more nutrition content should be included in medical school curricula.14,15 Our study supports this fact given the overall high level of satisfaction (8.58/10), agreeing that medical schools should include more nutrition curriculum (8.58/10), and high response rates of 73.9% (initial response rate) and 45.8% (3-months posttraining).
Our study also found a high level of student motivation to change their dietary behaviors. This may predict an increased likelihood of providing nutrition care, as previous studies have shown that doctors or medical students who follow healthy dietary habits are more likely to provide similar recommendations to their patients.16,17 Therefore, the ability of an intervention to improve the habits of students will not only improve their personal well-being but may also be passed on to their patients.18
This study has several limitations. Both the brevity of the survey and the short 3-month study time span may limit the validity of assessing long-term student knowledge retention. Moreover, the survey items reflect self-reported attitudes, which are susceptible to recall and social-desirability biases. A nonresponse bias may also be present, particularly with the decline in response rate for the 3-month survey, in which the students who responded may already be interested in the topic. This may impact generalizability. Further, we have no data to evaluate the actual practices of the students when counseling patients, which may be better measured in residency and postresidency doctors who are further involved in patient care. In addition, our intervention was limited to a single 1-hour lecture with a narrow focus on vitamins and minerals. Future studies should aim to include a more extensive, longitudinal curriculum that allows more concepts to be covered and repeated over time.19 Lastly, medical schools may choose to implement more hands-on programs that allow students to directly engage with the food. This has proven to be an effective tool for increasing nutrition competency.20,21
With a clearly demonstrated deficit in medical student nutrition education, it is important to continue implementing more content into the curricula. While nutrition education should be longitudinal with multiple training sessions, this pilot study evaluates the impact of a single nutrition session and shows promise for a larger-scale curricular nutrition integration.
Acknowledgments
Presentations:
Poster presentation, American Academy of Family Physicians National Conference, Kansas City, Missouri, July 2022.
Podium presentation, University of Southern California Research Day, Los Angeles, California, February 2023.
References
- Mokdad AH, Ballestros K, Echko M, et al; US Burden of Disease Collaborators. The state of US health, 1990-2016: burden of diseases, injuries, and risk factors among US states. JAMA. 2018;319(14):1444-1472. doi:10.1001/jama.2018.0158
- Bonaccio M, Di Castelnuovo A, Costanzo S, et al; Moli-sani Project Investigators. Nutrition knowledge is associated with higher adherence to Mediterranean diet and lower prevalence of obesity. Results from the Moli-sani study. Appetite. 2013;68:139-146. doi:10.1016/j.appet.2013.04.026
- Beydoun MA, Wang Y. Do nutrition knowledge and beliefs modify the association of socio-economic factors and diet quality among US adults? Prev Med. 2008;46(2):145-153. doi:10.1016/j.ypmed.2007.06.016
- Poínhos R, Oliveira BMPM, van der Lans IA, et al. Providing personalised nutrition: consumers’ trust and preferences regarding sources of information, service providers and regulators, and communication channels. Public Health Genomics. 2017;20(4):218-228. doi:10.1159/000481357
- Kolasa KM, Rickett K. Barriers to providing nutrition counseling cited by physicians: a survey of primary care practitioners. Nutr Clin Pract. 2010;25(5):502-509. doi:10.1177/0884533610380057
- Frank E, Segura C, Shen H, Oberg E. Predictors of Canadian physicians’ prevention counseling practices. Can J Public Health. 2010;101(5):390-395. doi:10.1007/BF03404859
- Adams KM, Kohlmeier M, Zeisel SH. Nutrition education in U.S. medical schools: latest update of a national survey. Acad Med. 2010;85(9):1537-1542. doi:10.1097/ACM.0b013e3181eab71b
- Crowley J, Ball L, Hiddink GJ. Nutrition in medical education: a systematic review. The Lancet Planetary Health. 2019;(3):E379-E389. doi:10.1016/S2542-5196(19)30171-8
- Adams KM, Butsch WS, Kohlmeier M. The state of nutrition education at US medical schools. J Biomed Educ. 2015;2015:1-7. doi:10.1155/2015/357627
- Mogre V, Amoore BY, Gaa PK. A scoping review of nutrition education interventions to improve competencies, lifestyle and dietary habits of medical students and residents. J Nutr Sci. 2023;12:e31. doi:10.1017/jns.2023.16
- Bassin SR, Al-Nimr RI, Allen K, Ogrinc G. The state of nutrition in medical education in the United States. Nutr Rev. 2020;78(9):764-780. doi:10.1093/nutrit/nuz100
- Reilly JM, Robinson K. Micronutrient Lecture-Survey Tool. Resource Library. Society of Teachers of Family Medicine; 2023. Accessed February 27, 2024. https://resourcelibrary.stfm.org/viewdocument/nutrition-project-survey-tool?CommunityKey=2751b51d-483f-45e2-81de-4faced0a290a&tab=librarydocuments
- Thomas DR. A General Inductive Approach for Analyzing Qualitative Evaluation Data. Am J Eval. 2006;27(2):237-246. doi:10.1177/1098214005283748
- Hawk VH, Kapounová Z, Krobot M, et al. Student and faculty perceptions of nutrition education in medical school. Clin Nutr ESPEN. 2022;47:351-357. doi:10.1016/j.clnesp.2021.11.011
- Mogre V, Stevens FCJ, Aryee PA, Amalba A, Scherpbier AJJA. Why nutrition education is inadequate in the medical curriculum: a qualitative study of students’ perspectives on barriers and strategies. BMC Med Educ. 2018;18(1):26. doi:10.1186/s12909-018-1130-5
- Schlair S, Hanley K, Gillespie C, et al. How medical students’ behaviors and attitudes affect the impact of a brief curriculum on nutrition counseling. J Nutr Educ Behav. 2012;44(6):653-657. doi:10.1016/j.jneb.2011.08.006
- Yu Y, Yang Y, Li Z, et al. The association between medical students’ lifestyles and their attitudes towards preventive counseling in different countries. BMC Public Health. 2015;15(1):1124. doi:10.1186/s12889-015-2458-y
- Wood NI, Gleit RD, Levine DL. Culinary nutrition course equips future physicians to educate patients on a healthy diet: an interventional pilot study. BMC Med Educ. 2021;21(1):280. doi:10.1186/s12909-021-02702-y
- Mogre V, Scherpbier AJJA, Stevens F, Aryee P, Cherry MG, Dornan T. Realist synthesis of educational interventions to improve nutrition care competencies and delivery by doctors and other healthcare professionals. BMJ Open. 2016;6(10):e010084. doi:10.1136/bmjopen-2015-010084
- Tan J, Atamanchuk L, Rao T, Sato K, Crowley J, Ball L. Exploring culinary medicine as a promising method of nutritional education in medical school: a scoping review. BMC Med Educ. 2022;22(1):441. doi:10.1186/s12909-022-03449-w
- Wood NI, Gleit RD, Levine DL. Culinary nutrition course equips future physicians to educate patients on a healthy diet: an interventional pilot study. BMC Med Educ. 2021;21(1):280. doi:10.1186/s12909-021-02702-y



There are no comments for this article.