Academic clinicians have multiple demands on their time, and many find themselves without enough time to work on scholarly pursuits. This problem is near universal, and while promotion criteria are changing, written products are still a significant part of the process. Therefore, writing is a skill that all of us in academia will need to find time to practice.
The best solution to finding time for writing is to have protected or supported time during the workday. We suggest an alternative approach to how the work of writing is perceived, especially when it is done on nights and weekends or other times of inconvenience. Because of high rates of burnout among family and other physicians1 we suggest writing for wellness. By writing for wellness, we mean using writing to deal with the stressors and challenges of work; increased clinical and educational demands and the minority tax for those faculty who are underrepresented in medicine. Writing for wellness could be an approach added to the resources to help physicians deal with burnout.1
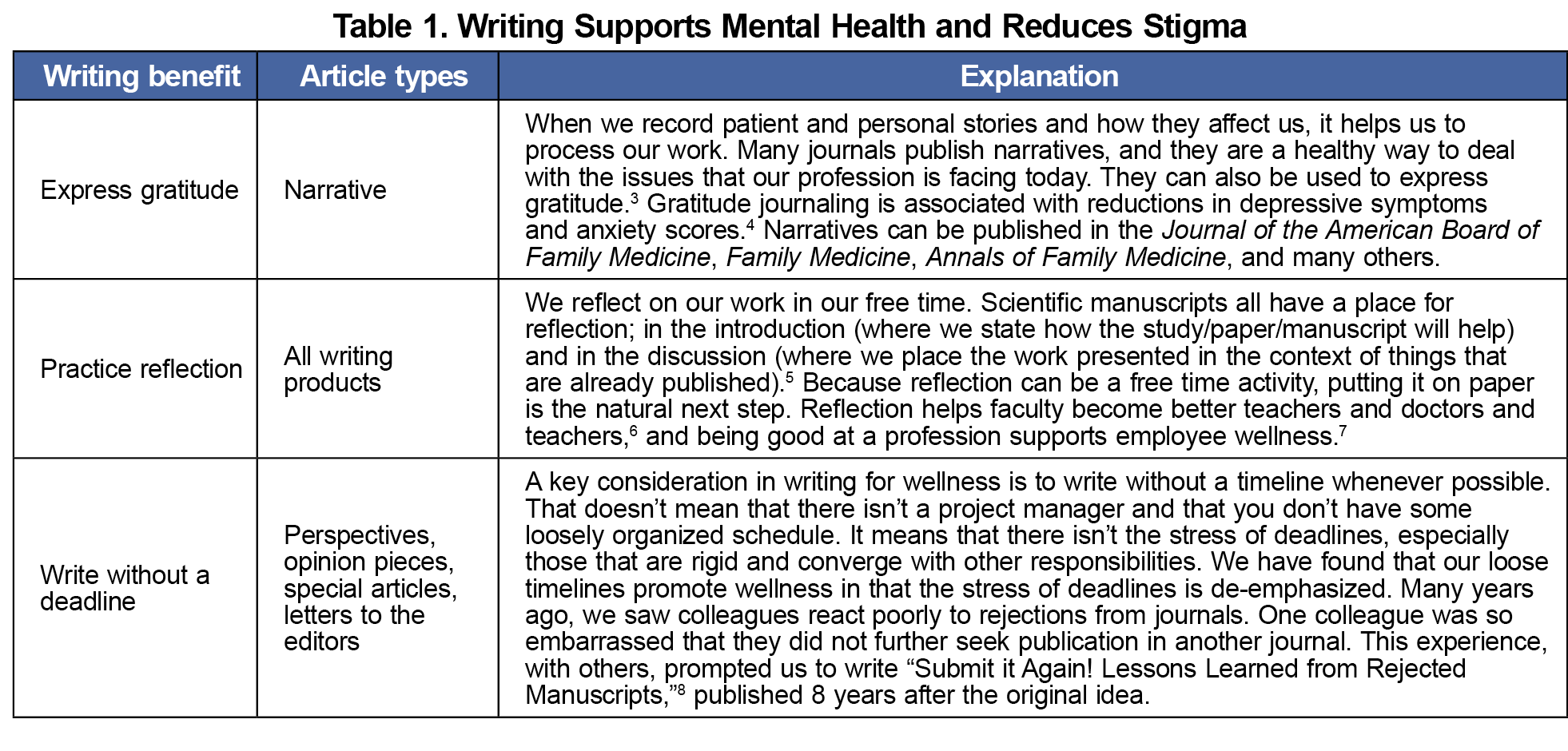
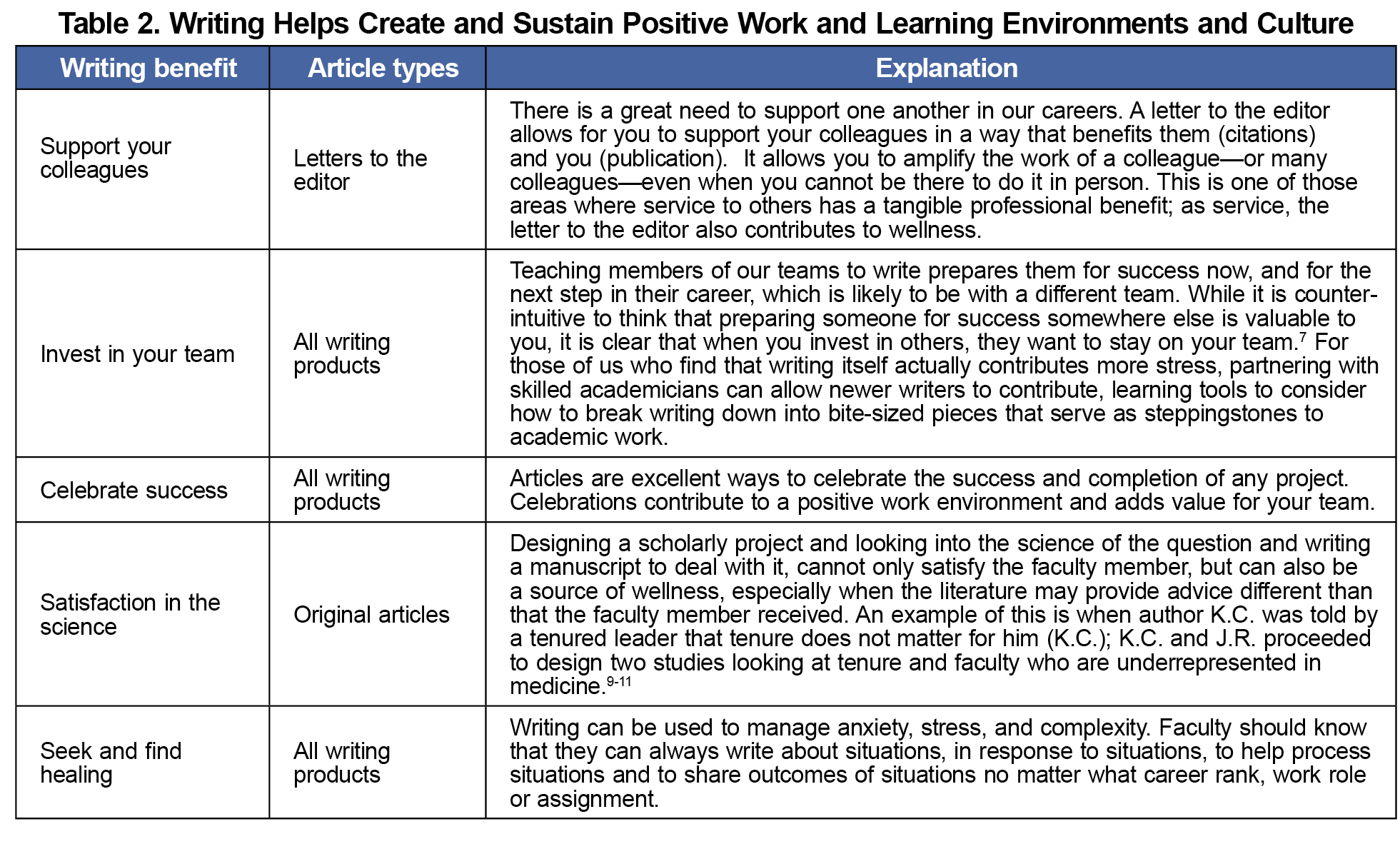
Faculty members participate in activities for wellness in their personal lives, whether that be spending time with family, exercising, vacations, etc. Those wellness activities are typically performed in their free time. If writing is seen as a wellness activity, then faculty members may choose to write during their free time. We understand that our approach to writing for wellness may be antithetical to popular culture. It may take some a lot of processing to arrive at the point where something seen as intrusive to personal time, labor, a chore, a difficult task, can be viewed as a path to wellness. Considering writing as wellness is a total reset to our thinking and approach. All avenues should be explored that have the potential to help promote wellness for academic physicians. The National Academy of Medicine’s National Plan for Health Workforce Well-being identified seven priority areas in which actions can be taken to ensure that the health workforce can find healing and well-being.2 Two of those areas, "create and sustain positive work and learning environments and culture,” and “support mental health and reduce stigma,” are places where writing can be used. In Tables 1 and 2, we explain the benefits of writing for wellness, and the article types that fit into that category.
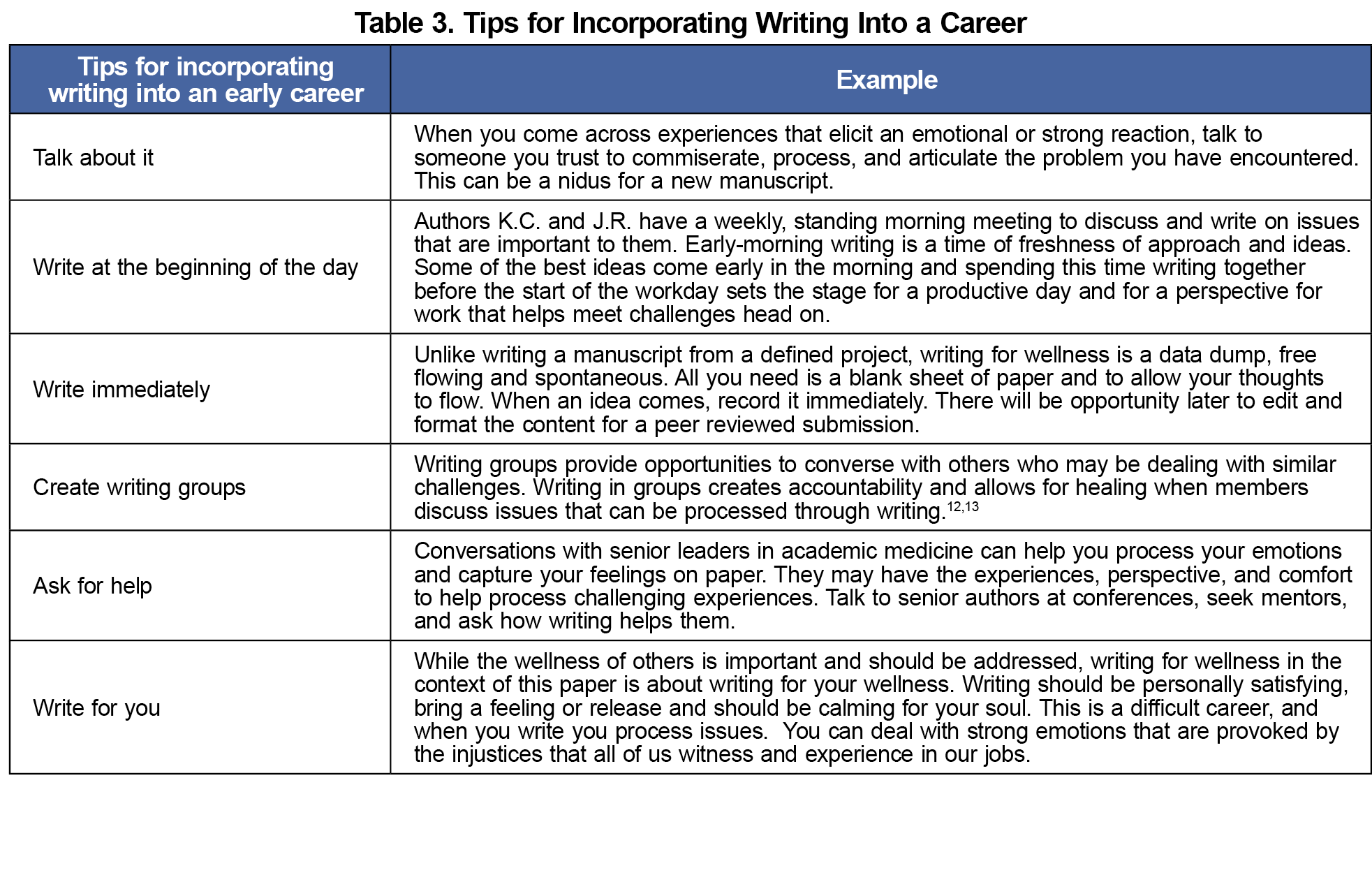
Incorporating writing into a busy career is a difficult task. Tips for incorporating writing are in Table 3. Making writing a priority, like exercise, can benefit the rest of your day. Thinking of it as a wellness activity legitimizes its use outside of work hours.
Early-career faculty should see writing as part of their jobs, no matter what their academic percentage is. Presenting writing as wellness offers an achievable reframing. When we are ill, we seek medical attention, sooner rather than later. When we are seeking wellness, the same urgency should apply. Immediate actions can get us to a better place.
The COVID-19 pandemic taught us that as stress increases the coping must rise to meet it, regardless of whether we are a patient, physician, or both. The coping skills that have assisted faculty members through years of training, medical errors, balancing childcare with clinical demands, and other difficult situations in their careers might not be enough as stressors compound. Faculty need to identify emotions and their related physical symptoms and seek interventions to ensure long-standing success in medicine. Faculty need to be self-aware to match the appropriate level of intervention to the level of distress. Writing for wellness can be an additional coping strategy. Writing has been shown to be impactful for a variety of medical conditions and as a stress reliever.14 This approach means that there is an access portal to wellness that a faculty member can traverse when needed, especially in times of stress or disorder. Writing is a tool that a faculty member can always access for wellness.
In this professional development perspective, we have discussed writing as a potent tool to promote both personal and professional wellness. Writing narratives help us process our work and writing letters to the editor help us support each other and those we supervise. In addition, writing provides the ability to celebrate successes and practice reflection. Because we already spend our nonwork time in the activities listed above, it is natural to take what we are already doing and allow it to benefit our careers. While we present writing for wellness as something that can be done during free time, institutions can support time for writing during the workday as a wellness initiative for individual faculty members. Harnessing this tool in a way that improves not only our own personal health but also contributes to the national dialog and career promotion is a three-for-one impact that even the most efficient of us can appreciate.



There are no comments for this article.