Background and Objectives: In health care, empathy is a clinician’s ability to understand a patient’s emotional state and convey that understanding in their care; and being culturally sensitive is communicating and respecting cultural differences. Providing health care on digital platforms introduces a new challenge of conveying empathy and cultural sensitivity. This study aimed to evaluate whether patients who were seen in-person had different perceptions of clinicians’ empathy and cultural sensitivity compared to those who were seen via telemedicine.
Methods: In this cross-sectional pilot study, we recruited primary care clinicians (N=8) and their telemedicine (N=14) and in-person patients (N=20) from two clinics at Emory University in Atlanta, Georgia. We evaluated clinicians’ empathy and cultural sensitivity by self-report and from patients’ standpoints.
Results: Patient perception of clinician empathy scores were similar (P value=.31) for in-person appointments (mean=33.8) and telemedicine appointments (mean=31.3). Patient perception of culturally sensitive communication varied in the sensitivity domain and was consistently low for the domain of discrimination (suggesting low discrimination among the clinicians) regardless of the modality of the visit.
Conclusions: This novel pilot study demonstrated comparable empathy and culturally sensitive communication scores in telemedicine and in-person visits, highlighting the potential for continued use of telemedicine in outpatient primary care. Delivery of care via telemedicine can enable an expansion of high-quality care to underserved communities. Future studies are needed to confirm our findings to enhance the experience of telemedicine visits for patients and clinicians.
Empathy and culturally sensitive communication are important communication tools for clinicians in a respectful and trusting patient-centered health care setting. Empathy is a clinician’s ability to understand a patient’s emotional state and to convey that understanding.1,2 Prior studies have shown that when patients perceive their clinicians as empathetic, they openly discuss their concerns, leading to better compliance, patient satisfaction, and improved health outcomes.3-10 Empathy also improves clinician well-being and prevents burnout.4,11 In addition to empathy, culturally sensitive communication is important to improve health outcomes.12,13 Culturally sensitive communication suggests an adept comprehension of patients’ cultural backgrounds, acknowledging how these backgrounds shape their attitudes and beliefs while demonstrating respect for such diversities.14-16 Both empathetic and culturally sensitive communication are critical to reducing disparities and improving the quality of primary care.
Telemedicine, which involves patient interactions via video or telephone conversations, experienced a rapid expansion during the COVID-19 pandemic.17-19 While improving access, these digital platforms pose unique barriers to patient-physician relationships and traditional expressions of empathy. Data evaluating patient perceptions of clinician empathy during telemedicine versus in-person visits are limited.
The objective of this pilot study was to descriptively compare whether patients who were seen in-person had different perceptions of clinicians’ empathy and cultural sensitivity compared to those who were seen via telemedicine.
We designed our study as a cross-sectional pilot study to evaluate empathy and culturally sensitive communication in telemedicine and in-person primary care outpatient services.
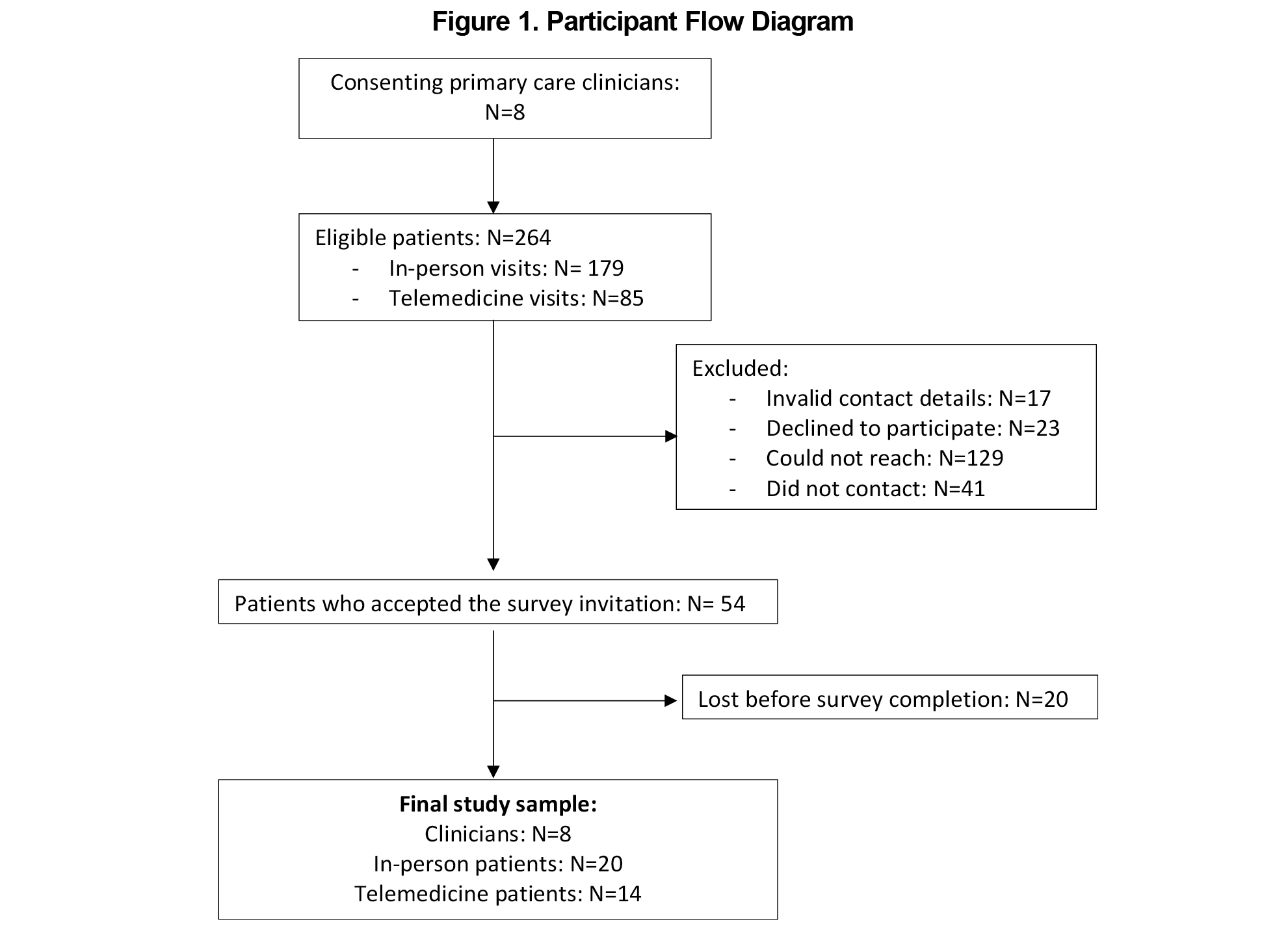
Using the Centers for Medicare & Medicaid Services definition of clinicians,20 this study recruited seven board-certified physicians in family or internal medicine and one physician assistant who offered both telemedicine and in-person care at Emory Healthcare. We also randomly enrolled 34 of their patients (20 in-person and 14 telemedicine) in 2022 (Figure 1). All participants provided informed consent before participating, and the study was determined exempt from review by the Emory Institutional Review Board under 45 CFR 46.104(d)(2II) (d)(3Ib).
Survey questionnaires were administered via RedCap21,22 (RedCap Consortium) and included two areas of inquiry: empathy and culturally sensitive communication.
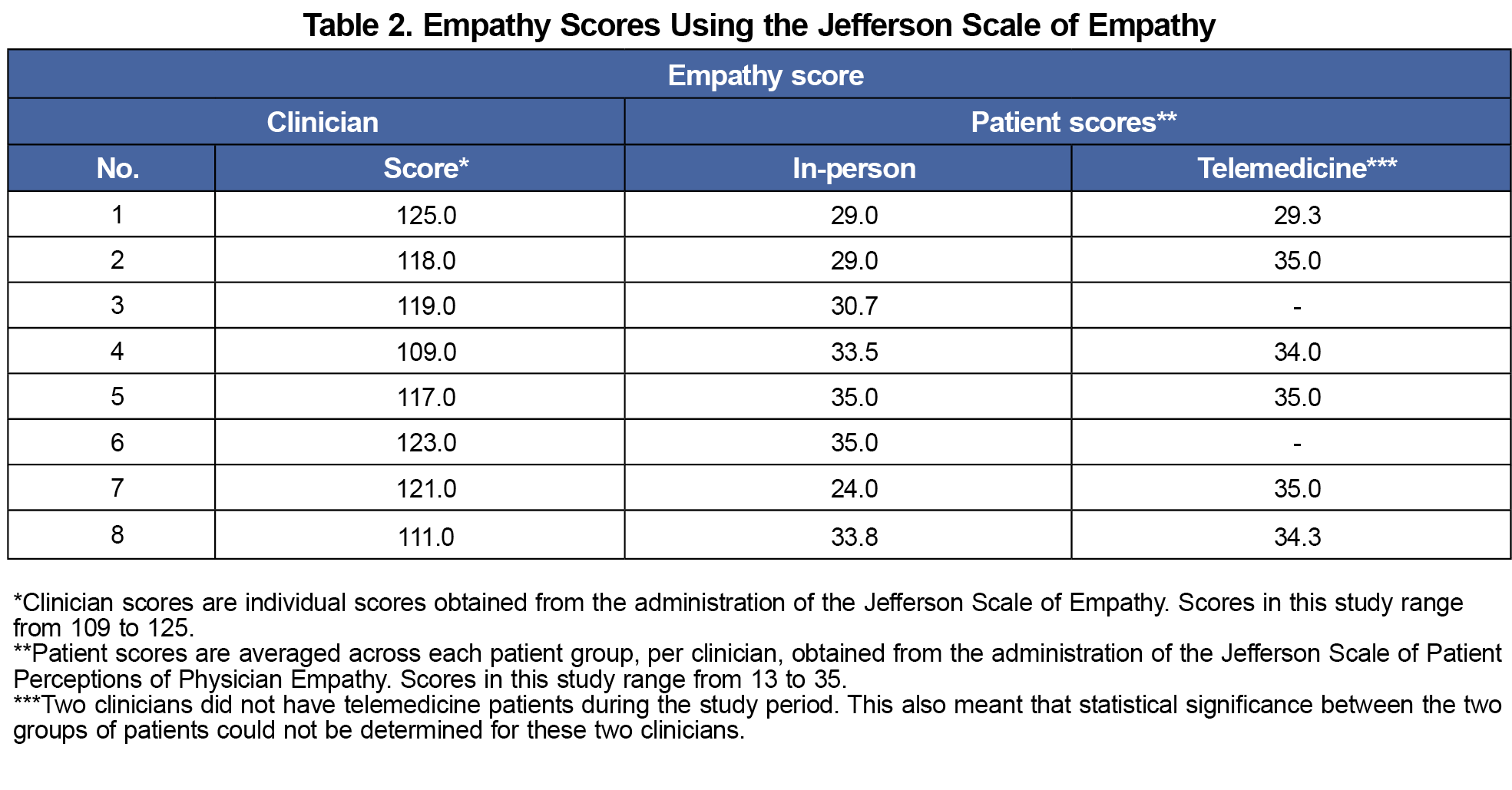
Clinicians’ self-reported empathy was determined by the Jefferson Scale of Empathy, a validated instrument that assesses perspective, compassion, and the ability to put oneself in a patient’s situation. Scores ranged from 20 to 140. Patients’ perception of empathy was determined by the Jefferson Scale of Patient’s Perceptions of Physician Empathy, where scores ranged from 5 to 35.23,24 In both scales, a higher score indicates greater empathy.
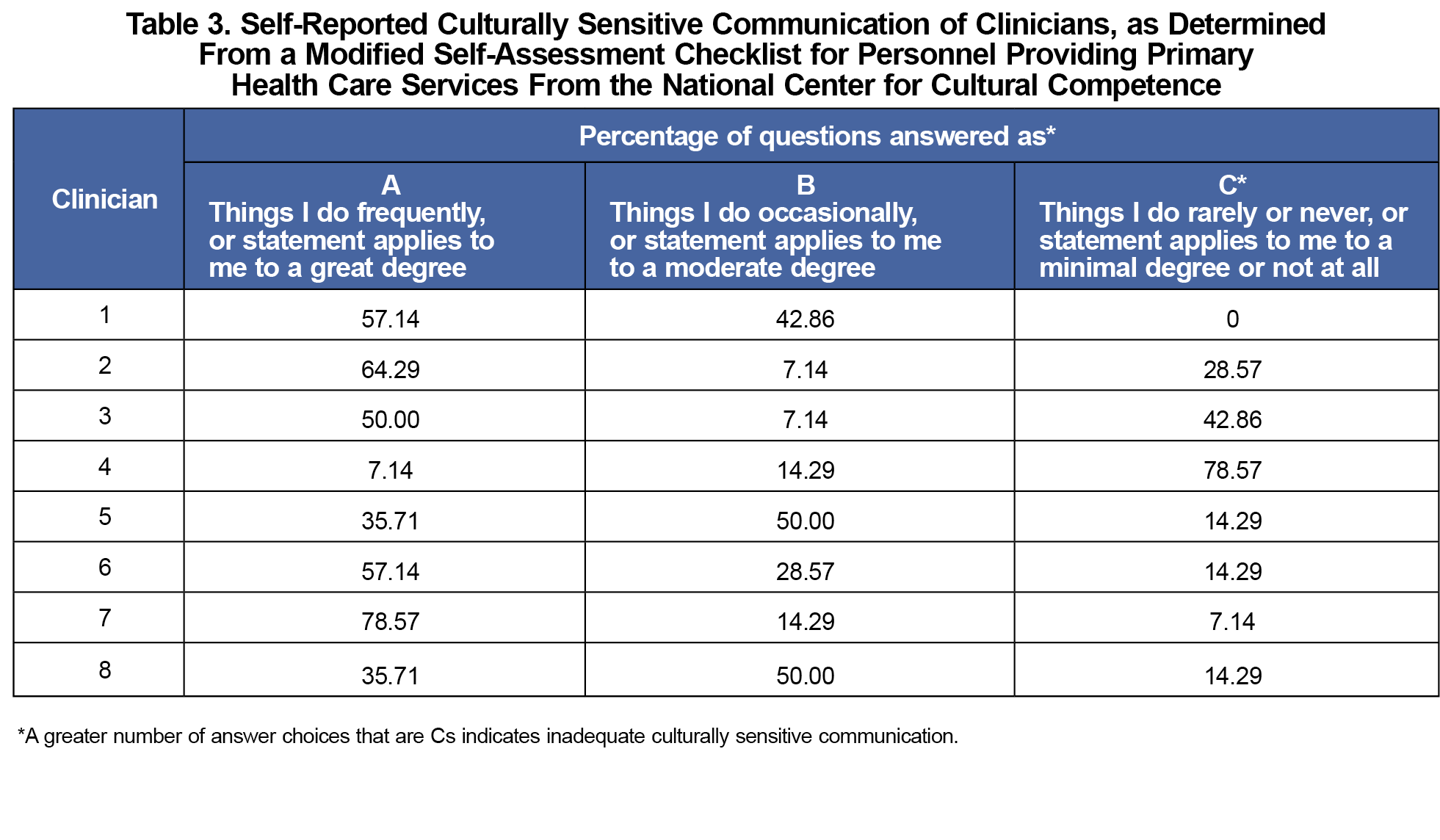
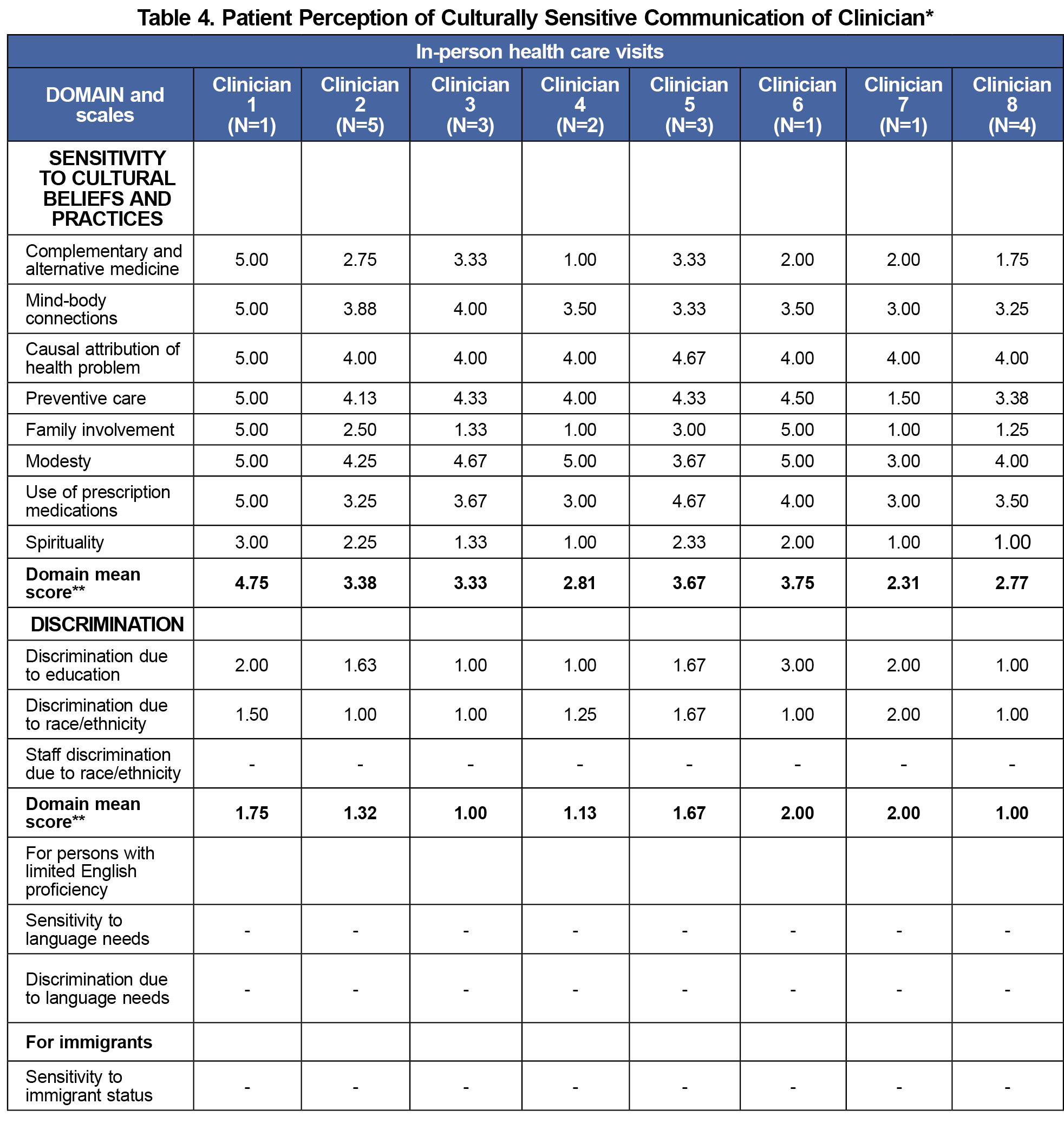
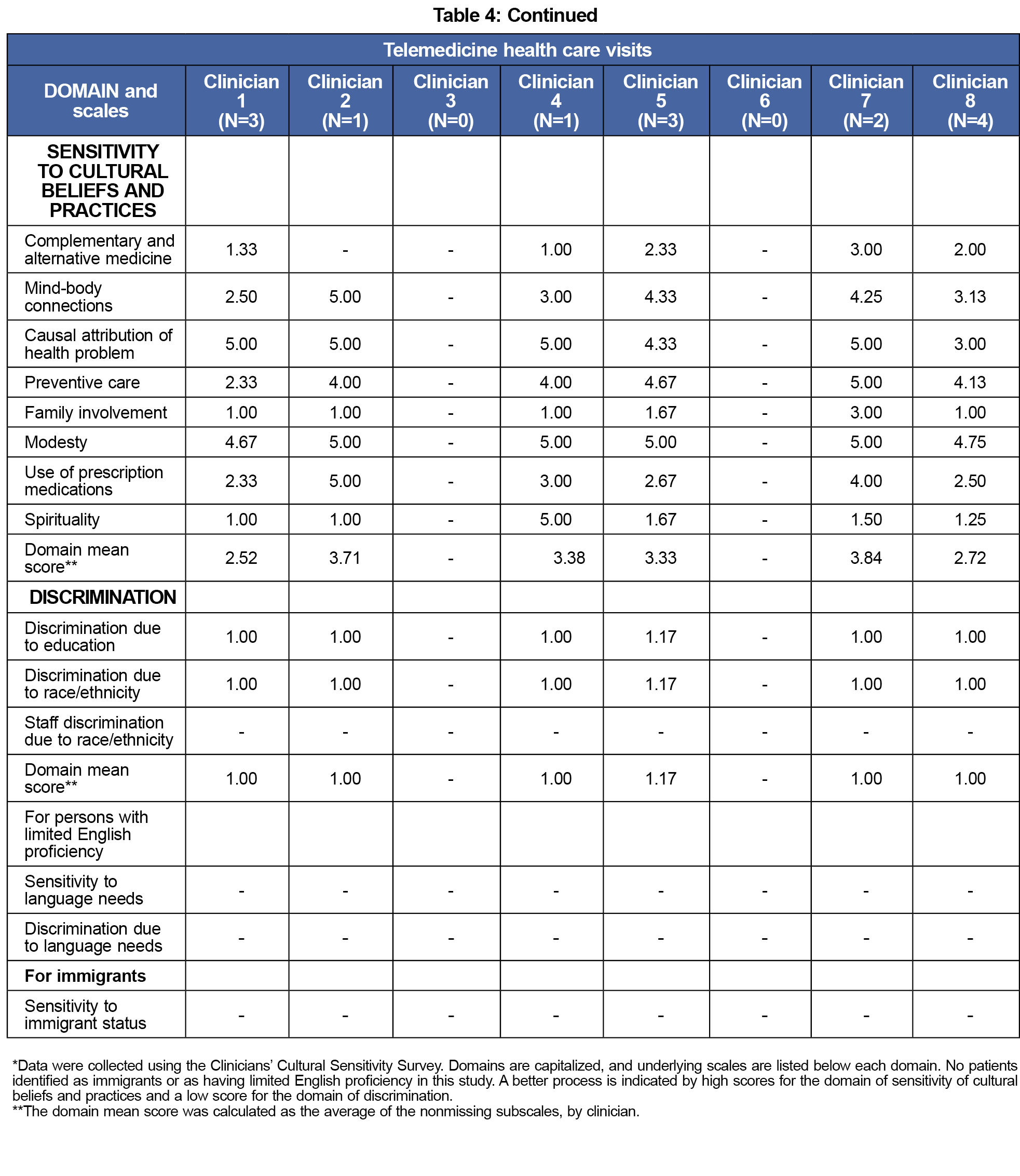
We used a modified scale from the National Center for Cultural Competence to measure clinicians’ self-perception of their cultural sensitivity25,26 This checklist identifies areas of growth with the intention to improve competence in these areas. To measure culturally sensitive care from the patient perspective, we used the Clinicians’ Cultural Sensitivity Survey.27 In the subscale for sensitivity to cultural beliefs, a higher score indicated a better process; and in the subscale for discriminatory behavior, a lower score indicated a better process.
Participant characteristics and demographics were presented as a mean(SD) or n(%). Validated questionnaire scales were scored using established guidelines and compared for in-person versus telemedicine patients.23-29 We also examined clinicians’ self-rated scores. Analyses were conducted using R statistical software version 4.2.2 (R Foundation).
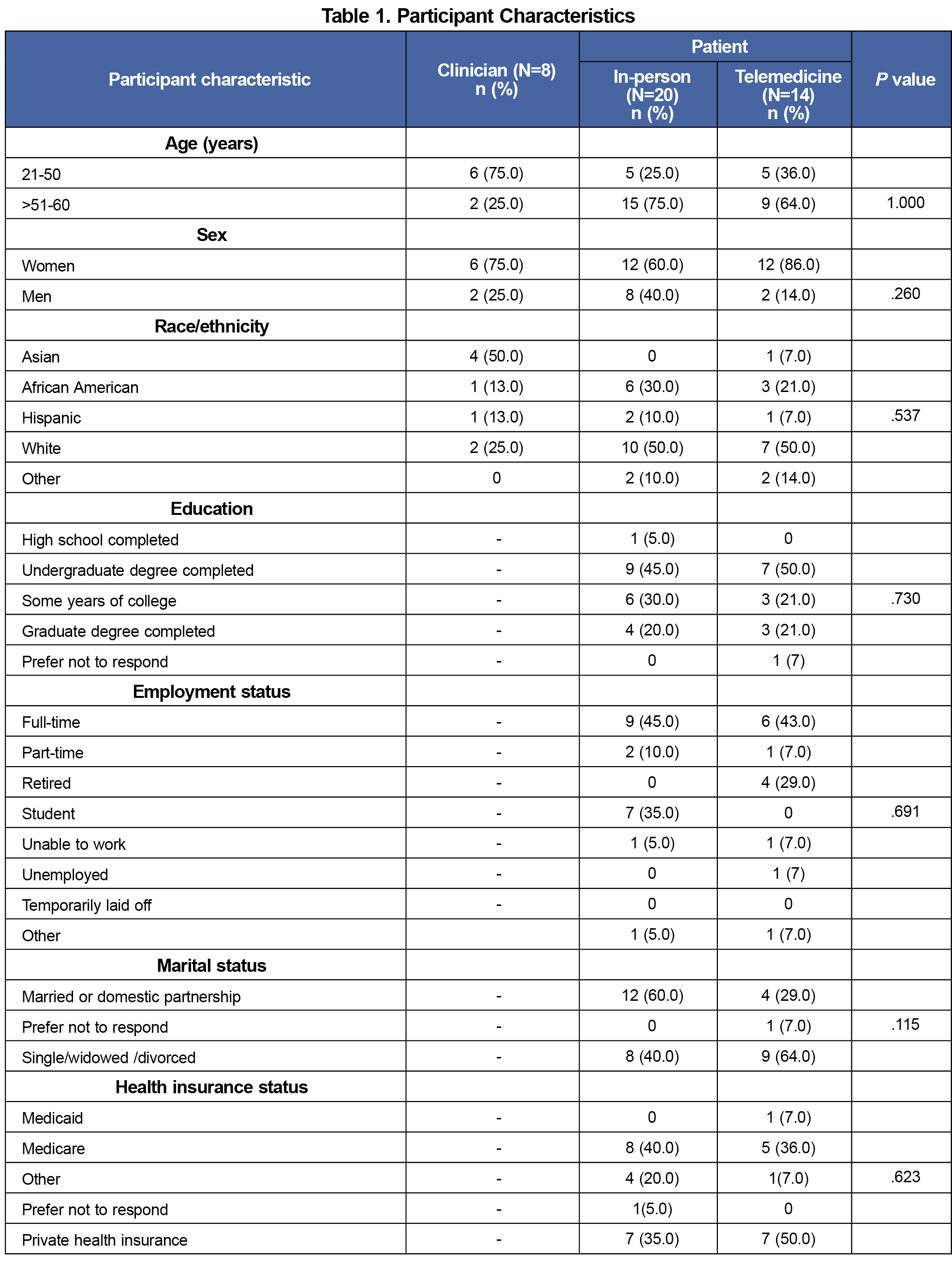
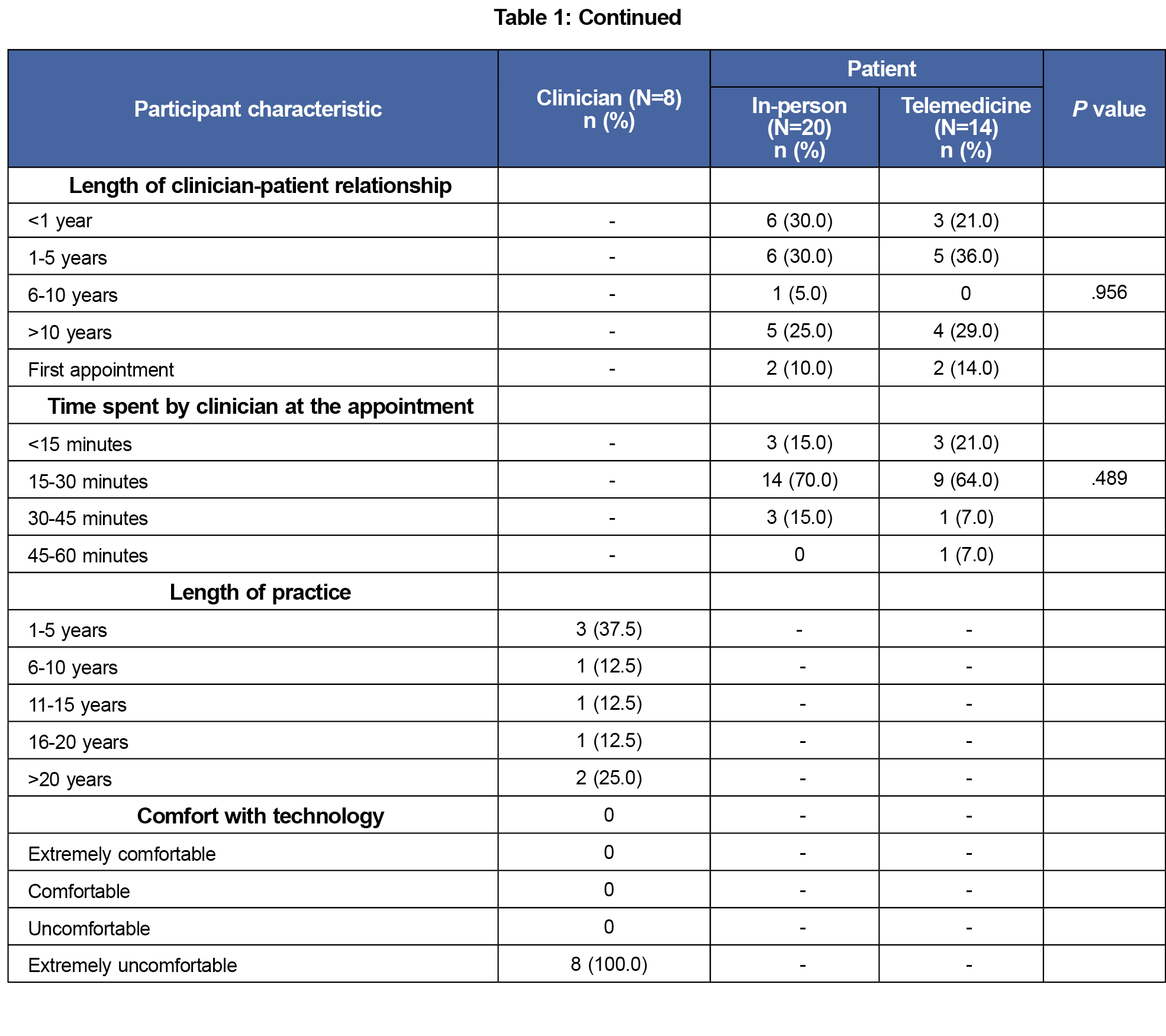
We enrolled eight clinicians, most of whom were women (75%), were less than 50 years of age (75%), and were Asian (50%). Among patients, a majority were greater than or equal to 50 years of age (75% in-person vs 64% telemedicine), identified as women, and identified as White. Employment status and educational qualifications were similar in both groups (Table 1).
Empathy Scores
Clinicians scored high on self-reported empathy, averaging 118 (range 109-125; Table 2). The average score of patients’ perception of clinician empathy (by clinician) was high and comparable across telemedicine and in-person (33.8 vs 31.3; P=.31).
Culturally Sensitive Communication
The clinician self-report (Table 3) scoring suggested that most clinicians (5 out of 8) perceived themselves as practicing culturally competent care. Scores for patient perception of clinician communication (presented as the average for each clinician; Table 4) varied widely for the subscale of cultural sensitivity for in-person (2.31-4.75) and telemedicine patients (2.52-3.84), and were comparable for subscales that measured sensitivity to alternative medicine, discrimination, family involvement, and spirituality in both modalities.
Discussion and Conclusions
Empathy and culturally sensitive communication are the foundation for an effective patient-clinician relationship. In our pilot study, patient perceptions of empathy appeared similar in telemedicine and in-person visits. Patient perception of culturally sensitive communication in the sensitivity domain varied widely in both modalities. In other subscales, such as discrimination, the scores were comparable, regardless of the modality of the visit.
Few studies have evaluated culturally sensitive communication in both types of visits and none in primary care.30,31 A study on stroke patients found no difference in the two modalities, while another evaluating psychological services found a preference for in-person visits.30,31 Our pilot study found that sensitivity in cultural communication varied, and discrimination was consistently low in both modalities. Our findings also suggested that ongoing training is needed for clinicians in alternative medicine, family involvement, and spirituality to advance their competence.
Our study was a cross-sectional pilot, funded competitively by a small health innovation program. As such, we cannot infer any causal association, and generalizability is limited. However, we included various clinicians and randomly selected patient participants in both modalities for the study. Response bias, common with most studies of this nature, is a possibility. Despite these limitations, this study is a first step to understanding essential pillars of communication and patient satisfaction between two different visit modalities of health care. Delivery of care via telemedicine can enable an expansion of high-quality care to previously underserved communities. Larger studies are needed to confirm our findings, and ongoing health care interventions can enhance the telemedicine visit experience for patients and clinicians.
Acknowledgments
The authors thank all participating clinicians and patients for their time and invaluable input. The authors also thank (a) Dr Mohammadreza Hojat and collaborators at Thomas Jefferson University for use of the Jefferson Scale of Empathy and Jefferson Scale of Patient’s Perceptions of Physician Empathy, and (b) the National Center for Cultural Competence for use of the Clinicians’ Cultural Sensitivity Survey.
Funding: This study was funded by the Healthcare Innovation Program/Georgia Clinical Translational Science Alliance Seed Grant Program (PI: Vinita Subramanya) and K23AG066931 (PI: Ambar Kulshreshtha).
References
- Hirsch EM. The role of empathy in medicine: a medical student’s perspective. Virtual Mentor. 2007;9(6):423-427. doi:10.1001/virtualmentor.2007.9.6.medu1-0706
- Mercer SW, Reynolds WJ. Empathy and quality of care. Br J Gen Pract. 2002;52(Suppl):S9-S12.
- Rakel D, Barrett B, Zhang Z, et al. Perception of empathy in the therapeutic encounter: effects on the common cold. Patient Educ Couns. 2011;85(3):390-397. doi:10.1016/j.pec.2011.01.009
- Halpern J. What is clinical empathy? J Gen Intern Med. 2003;18(8):670-674. doi:10.1046/j.1525-1497.2003.21017.x
- Suchman AL, Markakis K, Beckman HB, Frankel R. A model of empathic communication in the medical interview. JAMA. 1997;277(8):678-682. doi:10.1001/jama.1997.03540320082047
- Neumann M, Edelhäuser F, Tauschel D, et al. Empathy decline and its reasons: a systematic review of studies with medical students and residents. Acad Med. 2011;86(8):996-1,009. doi:10.1097/ACM.0b013e318221e615
- Rakel DP, Hoeft TJ, Barrett BP, Chewning BA, Craig BM, Niu M. Practitioner empathy and the duration of the common cold. Fam Med. 2009;41(7):494-501. https://www.stfm.org/familymedicine/vol41issue7/Rakel494
- Derksen F, Bensing J, Lagro-Janssen A. Effectiveness of empathy in general practice: a systematic review. Br J Gen Pract. 2013;63(606):e76-e84. doi:10.3399/bjgp13X660814
- Larson EB, Yao X. Clinical empathy as emotional labor in the patient-physician relationship. JAMA. 2005;293(9):1,100-1,106. doi:10.1001/jama.293.9.1100
- Neumann M, Bensing J, Mercer S, Ernstmann N, Ommen O, Pfaff H. Analyzing the “nature” and “specific effectiveness” of clinical empathy: a theoretical overview and contribution towards a theory-based research agenda. Patient Educ Couns. 2009;74(3):339-346. doi:10.1016/j.pec.2008.11.013
- Thirioux B, Birault F, Jaafari N. Empathy is a protective factor of burnout in physicians: new neuro-phenomenological hypotheses regarding empathy and sympathy in care relationship. Front Psychol. 2016;7:763. doi:10.3389/fpsyg.2016.00763
- Anderson LM, Scrimshaw SC, Fullilove MT, Fielding JE, Normand J; Task Force on Community Preventive Services. Culturally competent healthcare systems. a systematic review. Am J Prev Med. 2003;24(3,suppl):68-79. doi:10.1016/S0749-3797(02)00657-8
- Betancourt JR, Corbett J, Bondaryk MR. Addressing disparities and achieving equity: cultural competence, ethics, and health-care transformation. Chest. 2014;145(1):143-148. doi:10.1378/chest.13-0634
- Crawley LM, Marshall PA, Lo B, Koenig BA; End-of-Life Care Consensus Panel. Strategies for culturally effective end-of-life care. Ann Intern Med. 2002;136(9):673-679. doi:10.7326/0003-4819-136-9-200205070-00010
- Claramita M, Tuah R, Riskione P, Prabandari YS, Effendy C. Comparison of communication skills between trained and untrained students using a culturally sensitive nurse-client communication guideline in Indonesia. Nurse Educ Today. 2016;36:236-241. doi:10.1016/j.nedt.2015.10.022
- Douglas MK, Pierce JU, Rosenkoetter M, et al. Standards of practice for culturally competent nursing care: 2011 update. J Transcult Nurs. 2011;22(4):317-333. doi:10.1177/1043659611412965
- Terry C, Cain J. The emerging issue of digital empathy. Am J Pharm Educ. 2016;80(4):58. doi:10.5688/ajpe80458
- Shaver J. The state of telehealth before and after the COVID-19 pandemic. Prim Care. 2022;49(4):517-530. doi:10.1016/j.pop.2022.04.002
- Whitten P, Holtz B, Laplante C. Telemedicine: what have we learned? Appl Clin Inform. 2010;1(2):132-141. doi:10.4338/ACI-2009-12-R-0020
- Centers for Medicare & Medicaid Services. Quality measures & you: clinicians. Updated September 6, 2023. https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/mms/qmy-clinicians
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi:10.1016/j.jbi.2008.08.010
- Harris PA, Taylor R, Minor BL, et al; REDCap Consortium. The REDCap Consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi:10.1016/j.jbi.2019.103208
- Hojat M, DeSantis J, Gonnella JS. Patient perceptions of clinician’s empathy: measurement and psychometrics. J Patient Exp. 2017;4(2):78-83. doi:10.1177/2374373517699273
- Kane GC, Gotto JL, Mangione S, West S, Hojat M. Jefferson Scale of Patient’s Perceptions of Physician Empathy: preliminary psychometric data. Croat Med J. 2007;48(1):81-86.
- Goode TD, Dunne MC, Bronheim S. The Evidence Base for Cultural and Linguistic Competency in Health Care.Commonwealth Fund New York; 2006.
- National Center for Cultural Competence. Promoting cultural diversity and cultural competency: self-assessment checklist for personnel providing services and supports to children with disabilities and special health care needs and their families. NCCC. 2009.
- Nápoles AM, Santoyo-Olsson J, Farren G, et al. The patient-reported Clinicians’ Cultural Sensitivity Survey: a field test among older Latino primary care patients. Health Expect. 2012;15(1):63-77. doi:10.1111/j.1369-7625.2010.00654.x
- Hojat M, Mangione S, Nasca TJ, et al. The Jefferson Scale of Physician Empathy: development and preliminary psychometric data. Educ Psychol Meas. 2001;61(2):349-365. doi:10.1177/00131640121971158
- Hojat M, DeSantis J, Shannon SC, et al. The Jefferson Scale of Empathy: a nationwide study of measurement properties, underlying components, latent variable structure, and national norms in medical students. Adv Health Sci Educ Theory Pract. 2018;23(5):899-920. doi:10.1007/s10459-018-9839-9
- Cheshire WP, Barrett KM, Eidelman BH, et al. Patient perception of physician empathy in stroke telemedicine. J Telemed Telecare. 2021;27(9):572-581. doi:10.1177/1357633X19899237
- Ghosh A, Mahintamani T, Sharma K, et al. The therapeutic relationships, empathy, and satisfaction in teleconsultation for substance use disorders: better or worse than in-person consultation? Indian J Psychiatry. 2022;64(5):457-465. doi:10.4103/indianjpsychiatry.indianjpsychiatry_704_21



There are no comments for this article.