Introduction: Research has suggested that health care providers are not immune to implicit and explicit gender bias among their own colleagues and in the treatment of patients. To date, limited research examines gender bias in trainees and how that bias might intersect with patient care. Our study focused on gendered expectations, perceived competence of medical providers, and perceived acceptability of patients who advocate for themselves.
Methods: We used a 2x2x2x2 mixed design to examine the impact of participant gender, type of physical exam (vaginal vs elbow), trainee status, and gender of vignette physician. Participants read and responded to vignettes depicting various standardized clinical scenarios. The complete sample included 342 participants from a rural medical teaching hospital and a private liberal arts college in the same geographic region.
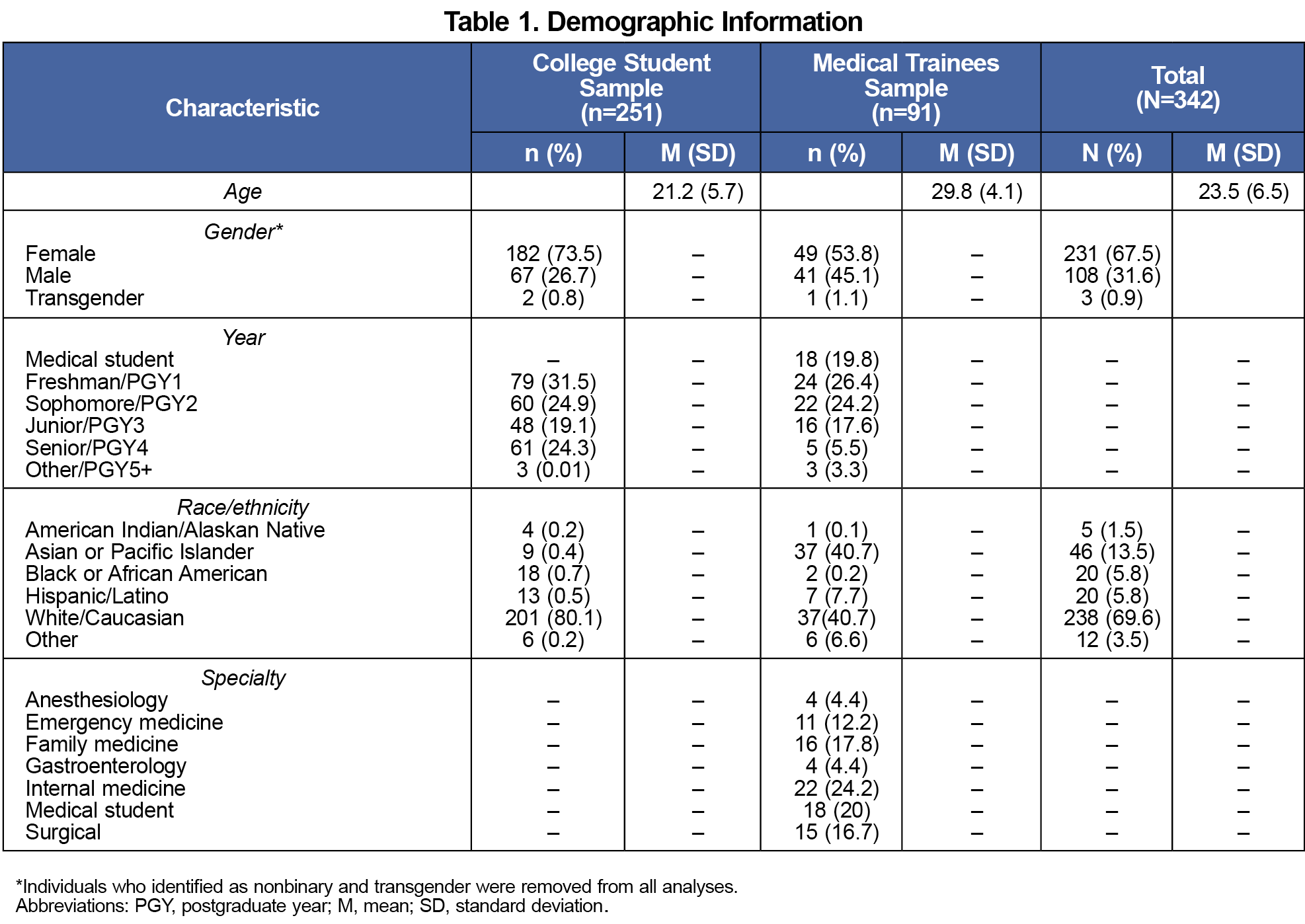
Results: Findings suggested a significant interaction between physicality and gender of the participant on perceived competence.
Conclusions: Although males and females had similar ratings of competence on an exam with low physicality (elbow), the data suggested that males did not recognize how errors during clinical practice may impact a hypothetical female patient. Future research might examine interventions that aim to increase awareness of gender bias among medical trainees and to explore whether interventions might improve patient care and perceptions of competence following identified errors.
In specialties such as family medicine, training milestones from the Accreditation Council for Graduate Medical Education require physicians to account for, recognize, and develop initiatives to minimize personal bias. Identifying and responding to bias, including gender bias, is essential to improving patient care. Because physicians rely on data and large amounts of knowledge for their work, they may believe that they are objective, which may blind them to their decision-making bias.1,2 Medically unmotivated differences in care across gender are evident in patients presenting with dermatological conditions, heart disease, polypharmacy, and neck and chronic pain.3–7 To date, limited research has examined gender bias in trainees and how that bias might intersect with patient care and perceptions of competence.
This study aimed to determine whether perceptions of provider competence, error, and justifiability of patients advocating for their rights would differ by trainee status (ie, medical trainee or college student), gender, or degree of physicality of the scenario (eg, how much the scenario dealt with a women’s health issue, such as a vaginal exam). We expected male participants (compared to female participants) to believe that errors made by a provider were less egregious. Consistent with broader cultural trends,8,9 we expected that male participants would perceive patients as less justified in making a complaint about the quality of their medical care.
Individuals from a liberal arts college and from a nearby rural teaching hospital were asked to participate in a voluntary survey of their opinions about medical care. All components of this study were considered exempt by the Institutional Review Board of the college and associated medical group.
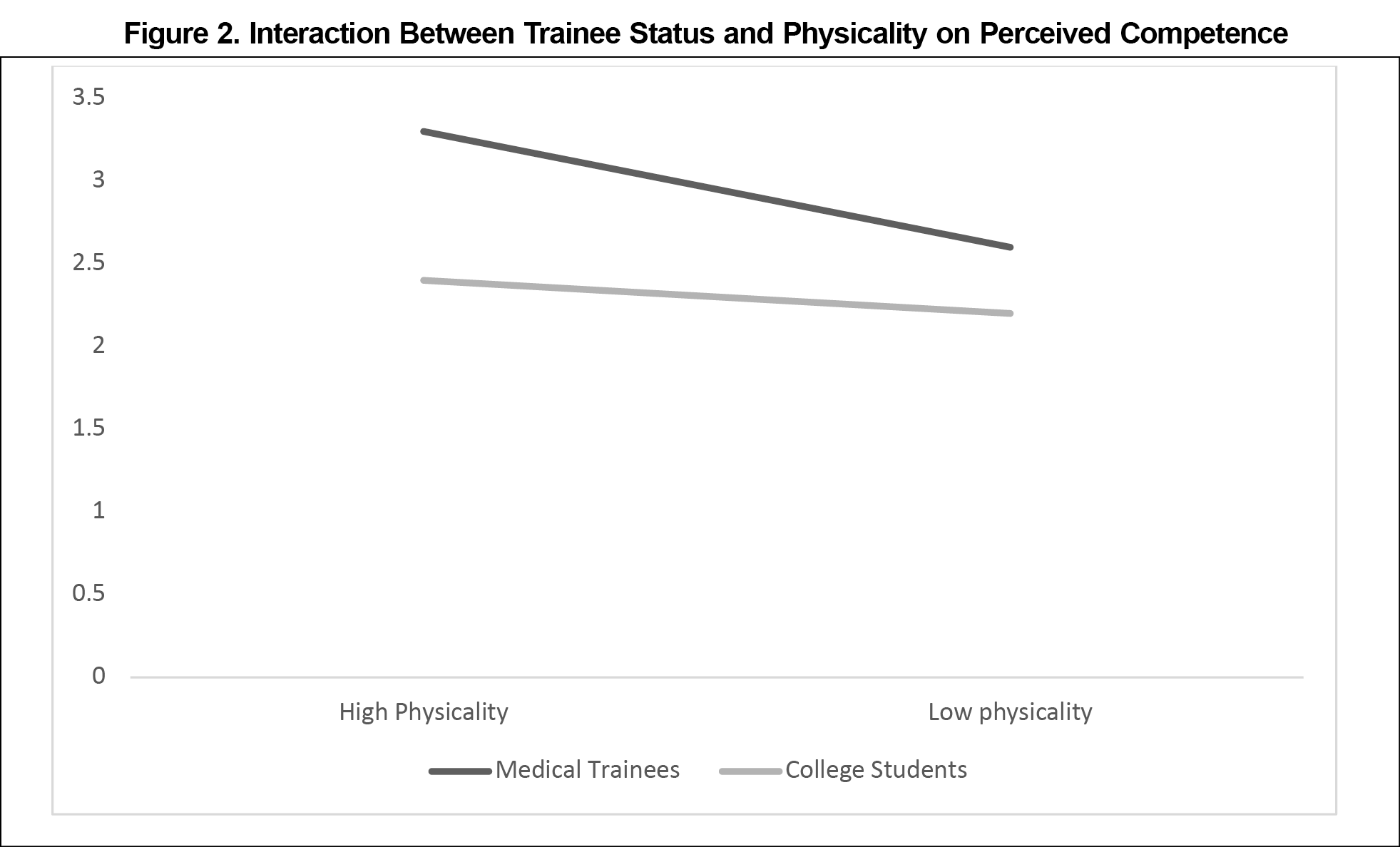
Due to the low number of individuals (n=3, 0.9%), nonbinary, two-spirit, and transgender individuals were excluded from analyses. The complete sample included 342 participants. See Table 1 for a list of demographic characteristics by sample.
Materials and Procedures
Respondents were asked to provide their opinions on the care of a medical provider as portrayed in one of two randomly assigned, standardized, written vignettes. The first vignette, portraying a male provider, described a college-aged woman receiving a routine vaginal exam (high physicality), while the second, portraying a female provider, detailed a college-aged woman who injured her elbow following a fall on an icy sidewalk (low physicality). Each vignette had four details that violated assumptions of patient-centered care: (a) not introducing themselves, (b) failing to ask before proceeding with the exam, (c) continuing the exam without acknowledging the patient’s pain, and (d) not responding personally to patient’s concerns.10 The vignettes did not provide any demographic information regarding the provider, with the exception of gender pronouns (she/her vs he/him).
Using the assessment tool developed for the purpose of this study, respondents rated the vignette provider’s overall competence from 1 (completely incompetent) to 7 (completely competent). They reported their opinion on the degree of severity the errors they perceived the provider made regarding the four assumptions of care derived from patient-centered care models. Respondents rated each assumption on a scale of 1 (none) to 7 (severe). Similarly, respondents used Likert scale ratings to assess their perceptions of how justified the patient was in making a complaint about the provider’s behavior across the four aspects of care. We summed responses to four questions to create a total score. The reliability estimates we calculated for both vignettes and all alphas were high (perceived error, α=0.81, 0.82; perceived justification, α=0.90, 0.92).
Analysis
We used a four-way mixed analysis of variance to examine main effects and interactions. The between-subjects independent variables were (a) gender of the provider in the vignette, (b) gender of the participant, (c) and trainee status. We also used a within-subjects variable of physicality. We considered three dependent variables: (a) perceived competence of medical provider, (b) perceived degree of error, and (c) perceived justification of patient complaint.
Perceived Competence
Results indicated a main effect of physicality on perceived competence (F[1, 313]=25.53, P<.001, ηp2=0.08). Regardless of the gender of the vignette provider, the provider conducting the vaginal exam (M=2.91, SD=1.48) was perceived as more competent than the physician performing the elbow exam (M=2.47, SD=1.85).
Our data revealed an interaction between physicality and gender of the participant on perceived competence (F[1, 313]=7.33, P<.01, ηp2=0.02). Among women, ratings of competence did not differ based on physicality, whereas men rated the physician performing the vaginal exam as being more competent than the physician performing the elbow exam (Figure 1).
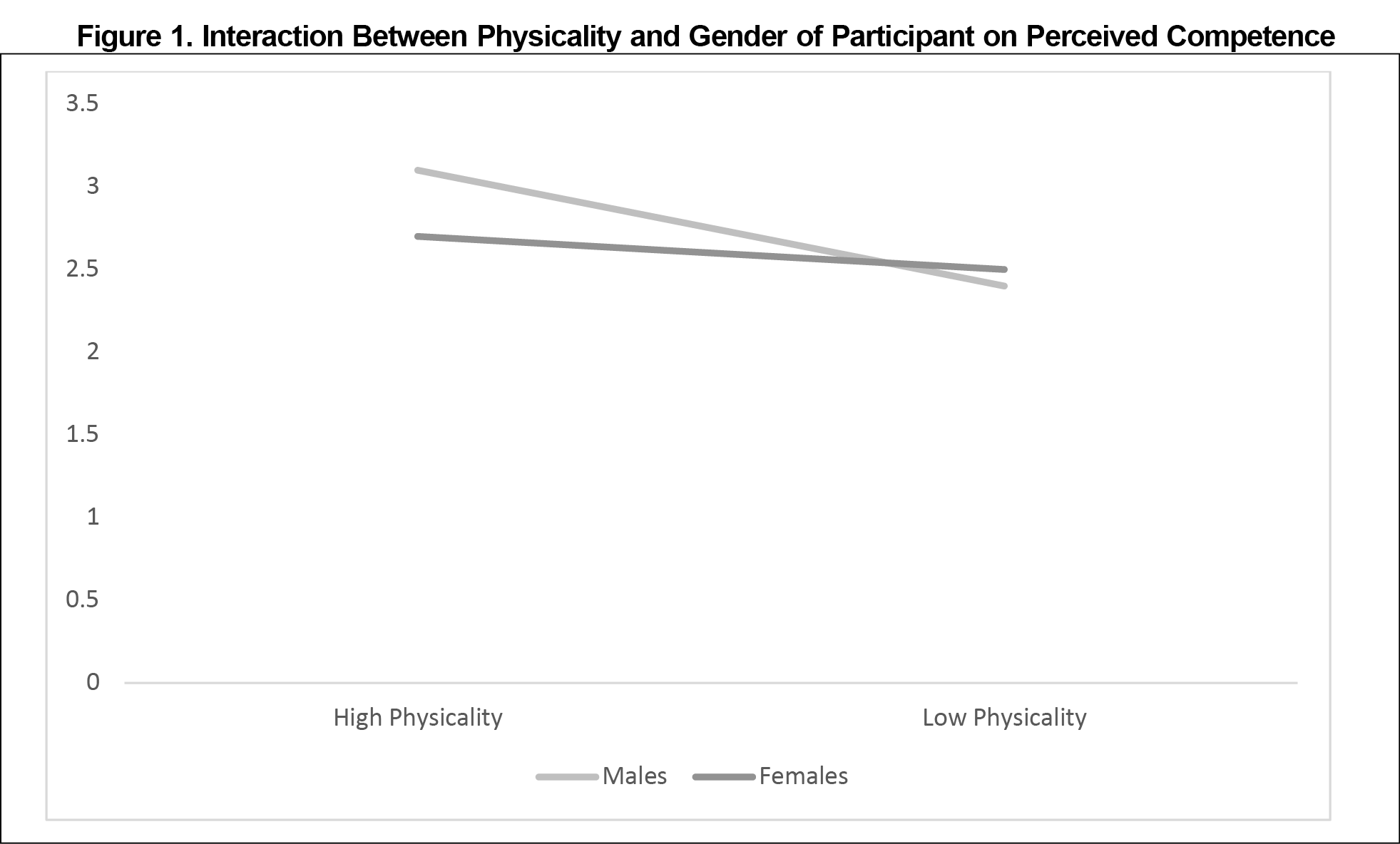
We found a main effect of sample type on perceived competence (F[1, 313]=19.21, P<.001, ηp2=0.06). Medical trainees rated the physicians in the vignettes as significantly more competent (M=3.02, SD=2.40) than did the college student participants (M=2.36, SD=1.48).
We identified an interaction between sample type and physicality on perceived competence (F[1, 313]=5.53, P=.02, ηp2=0.02). Across physicality, the medical trainees rated the physician performing the vaginal exam as significantly more competent (M=3.33, SD=0.13; Figure 2).
Perceived Error
We found a main effect of physicality on perceived error (F[1, 325]=22.44, P<.001, ηp2=0.07). The vignette physician performing the elbow exam was perceived as having made worse errors (M=24.77, SD=4.15) compared to the physician performing the vaginal exam. College students perceived the vignette physician to have made significantly more errors (F[1, 325]=5.43, P=.02, ηp2=0.02; M=24.83, SD=4.68) than did the medical trainees (M=23.77, SD=6.84). Female participants perceived the vignette physician (F[1, 325]=6.43, P=.01, ηp2=0.02; M=24.87, SD=5.04) to have made significantly more errors than did the male participants (M=23.72, SD=6.49).
Perceived Justification
We identified a main effect of physicality on participant’s perceptions of how justified the vignette patient was in making a complaint (F[1, 328]=12.11, P=.001, ηp2=0.04). Respondents perceived the patient who received the elbow exam as being more justified (M=23.86, SD=6.16) compared to the patient who received the vaginal exam (M=22.99, SD=6.16).
Female participants thought that the patient was more justified in making a complaint (F[1, 328]=6.44, P=.01 , ηp2=0.02, M=24.22, SD=7.06) than did the male participants (M=22.62, SD=8.87).
Perceptions of physician competence may depend on whether the physician’s performance is being evaluated by a college student or a medical trainee. Members of the general public may be harsher critics than other medical providers.
Males perceived the physician performing a vaginal exam as more competent than the one completing an elbow exam, and they rated the physician performing a vaginal exam as more competent compared to female respondents. Given the two-way interaction, males perceived providers as making less egregious errors and vignette patients as being less justified in their complaints than did female respondents.
The absence of a three-way interaction between physicality, gender, and participant type suggests that a gender bias was not specific to medical trainees but was possibly a broader impact of cultural and gendered expectations. This study may have been underpowered to find an effect of this nature. While findings were statistically significant, this study did not address whether these differences impacted patient care.
This study aimed to explore gender bias that may exist within a sample of medical trainees. Findings suggested that trainees who are working in health care are not immune to bias. Future research might examine interventions that aim to increase awareness of gender bias among medical trainees in their patient care behaviors.
References
- Uhlmann EL, Cohen GL. “I think it, therefore it’s true”: effects of self-perceived objectivity on hiring discrimination. Organ Behav Hum Decis Process. 2007;104(2):207-223. doi:10.1016/j.obhdp.2007.07.001
- Salles A, Awad M, Goldin L, et al. Estimating implicit and explicit gender bias among health care professionals and surgeons. JAMA Netw Open. 2019;2(7):e196545. doi:10.1001/jamanetworkopen.2019.6545
- Nyberg F, Osika I, Evengård B. “The Laundry Bag Project”—unequal distribution of dermatological healthcare resources for male and female psoriatic patients in Sweden. Int J Dermatol. 2008;47(2):144-149. doi:10.1111/j.1365-4632.2008.03485.x
- Hamberg K, Risberg G, Johansson EE, Westman G. Gender bias in physicians’ management of neck pain: a study of the answers in a Swedish national examination. J Womens Health Gend Based Med. 2002;11(7):653-666. doi:10.1089/152460902760360595
- Johnston N, Bornefalk-Hermansson A, Schenck-Gustafsson K, et al. Do clinical factors explain persistent sex disparities in the use of acute reperfusion therapy in STEMI in Sweden and Canada? Eur Heart J Acute Cardiovasc Care. 2013;2(4):350-358. doi:10.1177/2048872613496940
- Haider SI, Johnell K, Weitoft GR, Thorslund M, Fastbom J. The influence of educational level on polypharmacy and inappropriate drug use: a register-based study of more than 600,000 older people. J Am Geriatr Soc. 2009;57(1):62-69. doi:10.1111/j.1532-5415.2008.02040.x
- Hoffmann DE, Tarzian AJ. The girl who cried pain: a bias against women in the treatment of pain. J Law Med Ethics. 2001;29(1):13-27. doi:10.1111/j.1748-720X.2001.tb00037.x
- Anderson I, Swainson V. Perceived motivation for rape: gender differences in beliefs about female and male rape. Curr Res Soc Psychol. 2001;6(8):107-123.
- McQuiller Williams L, Porter JL, Smith TR. Understanding date rape attitudes and behaviors: exploring the influence of race, gender, and prior sexual victimization. Vict Offenders. 2016;11(2):173-198. doi:10.1080/15564886.2014.960025
- Hashim MJ. Patient-centered communication: basic skills. Am Fam Physician. 2017;95(1):29-34.



There are no comments for this article.