The overall prevalence rate of bullying in medical residency is 51%, with higher odds of experiencing negative acts among females and minorities.1 Trainees who are subject to negative acts have increased risk of job dissatisfaction, burnout, strain on mental health, and accidents at work.2-6 The most common perpetrators of bullying are attending physicians and clinical support staff, and the hierarchical structures in medical education are primary sources of bullying and burnout.1 A favorable supervisory alliance (ie, the relationship between a supervisor and supervisee) has been associated with trainee self-efficacy, greater job satisfaction, and more availability of coping resources. Conversely, a weak supervisory alliance has been associated with greater stress, burnout, and more perceived negative events.7 The aim of this study was to determine whether supervisory alliance (eg, rapport with supervisor) mediated the association between perceived bullying and trainee burnout. We hypothesized that a trainee’s rapport with an attending physician may explain the association between bullying and burnout.
RESEARCH BRIEF
The Mediating Role of Attending Rapport on Bullying and Medical Trainee Burnout
Danielle L. Terry, PhD, ABPP | Kartik Moza, MD
PRiMER. 2024;8:30.
Published: 5/14/2024 | DOI: 10.22454/PRiMER.2024.840270
Background and Objectives: The aim of this study was to determine whether supervisory alliance (eg, rapport with supervisor) mediated the association between perceived bullying and trainee burnout.
Methods: We administered electronic surveys to medical trainees (N=108) in a rural teaching hospital. The survey included measures of bullying, burnout, and supervisory rapport.
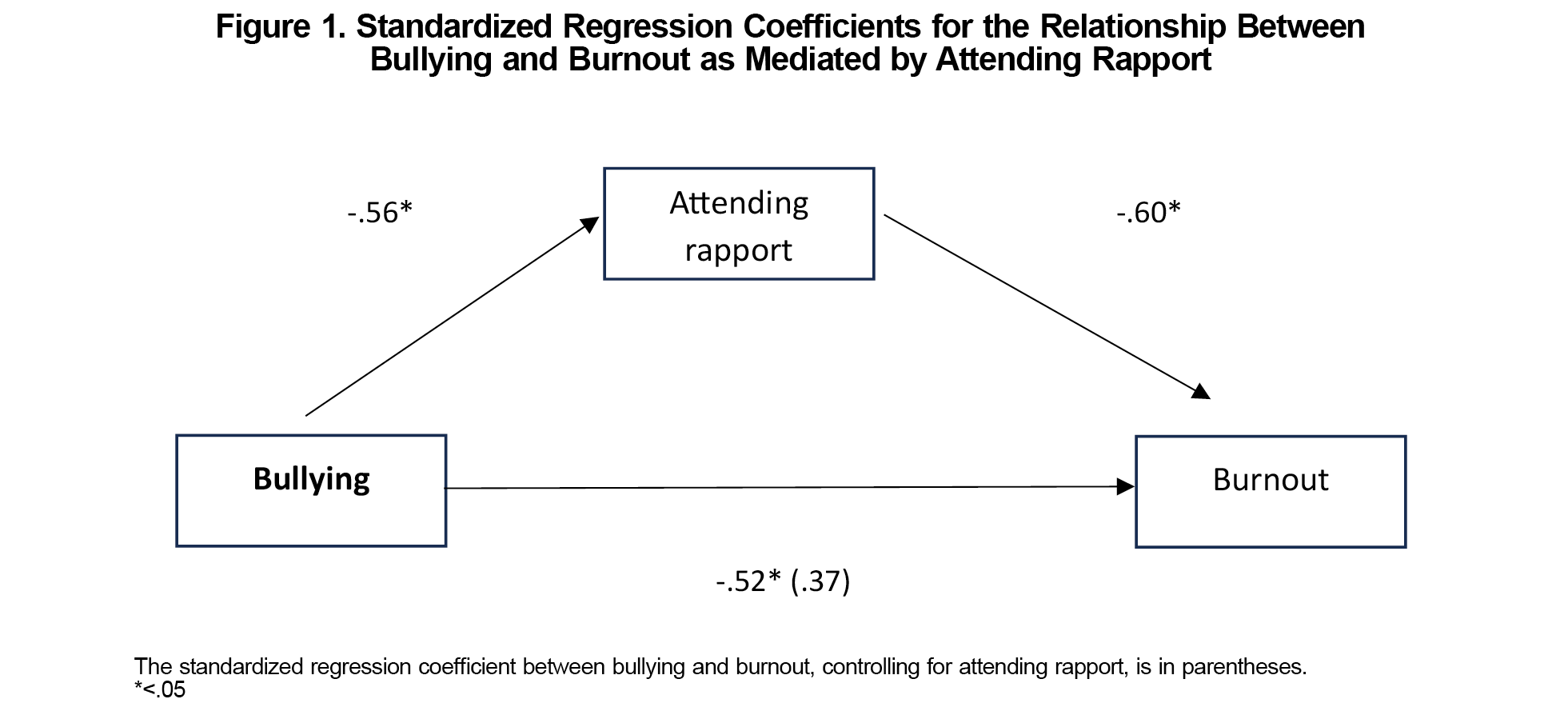
Results: Using Baron and Kenny’s test of mediation with the Sobel test, we found that rapport with supervising attending partially mediated the relationship between bullying and burnout.
Conclusions: This study reinforced the role of the attending physician and how perceived rapport may impact burnout. Given the high rate of bullying in medical training and the negative impact of burnout on physicians, further study is warranted to understand other factors that mediate the association between bullying and burnout.
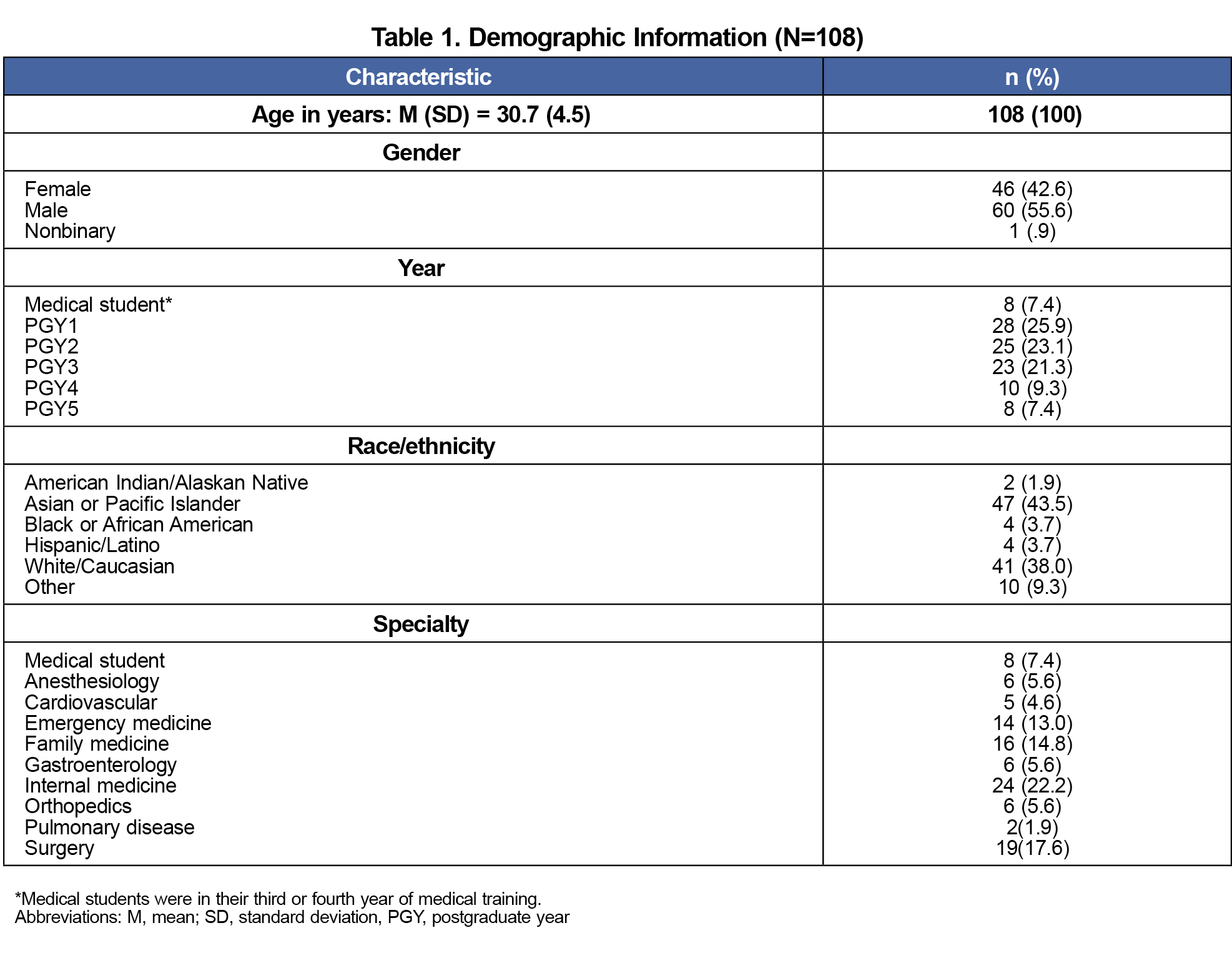
Participants included 108 medical trainees (81% response rate) from a rural teaching hospital in Pennsylvania. Medical trainees were approached at group meetings and offered an opportunity to participate in a voluntary survey. All procedures performed were considered exempt by the Institutional Review Board of the college and associated medical group. We used descriptive analyses to examine demographic characteristics and tested a mediational model via methodology described by Baron and Kenny.8
Trainees voluntarily scanned a QR code linked to a survey examining the impact of supervisory alliance that was developed using SurveyMonkey software (SurveyMonkey Inc). Questions included demographic information (age, gender identity, year in program, and medical specialty). We used the Mini-Z9 as an efficient and validated measure of burnout. This item asked respondents to indicate their level of burnout from 1 (no symptoms) to 5 (I feel completely burned out and often wonder if I can go on. I am at the point where I may need some changes or may need to seek some sort of help).
We used the brief form of the Supervisory Working Alliance Inventory10 to assess the perceived working alliance between medical trainees and attending physicians. This measure was developed and validated in nonmedical settings, and we modified terminology to use medical terms (eg, patient vs client, attending vs supervisor). This instrument includes five items that are rated from 1 (almost never) to 7 (almost always) and includes two subscales related to client focus and rapport with supervisor. The total scale reliability estimate was 0.91.
We used the Negative Acts Questionnaire-Revised,11 which has been used with medical trainees,12 to assess experiences of bullying and negative acts by others within the training environment. The total scale reliability estimate was 0.90.
See Table 1 for a list of demographic characteristics by sample. We tested a mediation model using steps outlined by Baron and Kenny’s test of mediation.8 First, simple linear regression indicated that bullying was a significant predictor of burnout (β=.52, t=5.9, P<.01). Second, regression analysis indicated that bullying was significantly associated with supervisory rapport (β=–.56, t=-6.42, P<.01). Third, both the independent variable (bullying) and the mediator (supervisory rapport) significantly predicted burnout (F[2,92]=20.92, P<.001). We used the Sobel test to determine whether rapport with attending mediated the relationship between bullying and burnout. This test confirmed that rapport with supervising attending partially mediated the relationship between bullying and burnout (z=2.36, P=.012; Figure 1).
Understanding the mediational mechanisms that explain the connection of a stimulus and response can assist with designing interventions to modify specific outcomes.13 This study highlighted a connection between bullying experiences and burnout. While most studies have highlighted the role of attending physicians as the primary perpetrators of bullying,1 this study suggested an influential role of the attending physician and that perceived rapport may increase or decrease burnout. Results inferred partial mediation (as opposed to full mediation), which also indicated that supervisory rapport may be responsible for a portion of the relationship between bullying and burnout.
These findings are consistent with a larger body of literature that suggests that supervisory alliance is associated with greater coping resources and greater job satisfaction.7 Programs that aim to provide mentorship to those most impacted by bullying (eg, females and those underrepresented in medicine) also have highlighted a positive impact on satisfaction with work climate.14 Programs that work to enhance supervisory rapport and provide mentorship may positively impact trainees, especially those affected by bullying and negative acts.
While attending physicians may be fostering relationships that mitigate the impact of bullying by other clinical staff, they also may be reducing their own negative impact. Thus, whether the rapport mechanism has an impact via additional support or is simply a perception of reduction in bullying behaviors is unclear. Regardless of reason, our findings highlight the potential import of fostering rapport between attendings and trainees.
Limitations
Our study had several limitations, including its cross-sectional design and inability to make causal inferences, with potentially limited generalizability due to its rural, single-site sample.
This study suggests that rapport with attending physicians partially mediates the relationship between bullying and burnout among medical trainees. Further study is warranted to understand other factors that mediate this association. Given the significant costs associated with medical provider burnout15 and the high rates of negative acts experienced by medical trainees, understanding mechanisms that may offset this public health concern is essential.
References
- Álvarez Villalobos NA, De León Gutiérrez H, Ruiz Hernandez FG, Elizondo Omaña GG, Vaquera Alfaro HA, Carranza Guzmán FJ. Prevalence and associated factors of bullying in medical residents: a systematic review and meta-analysis. J Occup Health. 2023;65(1):e12418. doi:10.1002/1348-9585.12418
- Paice E, Smith D. Bullying of trainee doctors is a patient safety issue. Clin Teach. 2009;6(1):13-17. doi:10.1111/j.1743-498X.2008.00251.x
- Chia MC, Hu YY, Li RD, et al. Prevalence and risk factors for burnout in U.S. vascular surgery trainees. J Vasc Surg. 2022;75(1):308-315.e4. doi:10.1016/j.jvs.2021.06.476
- Kemper KJ, Schwartz A; Pediatric Resident Burnout-Resilience Study Consortium. Bullying, discrimination, sexual harassment, and physical violence: common and associated with burnout in pediatric residents. Acad Pediatr. 2020;20(7):991-997. doi:10.1016/j.acap.2020.02.023
- Samsudin EZ, Isahak M, Rampal S. The prevalence, risk factors and outcomes of workplace bullying among junior doctors: a systematic review. Eur J Work Organ Psychol. 2018;27(6):700-718. doi:10.1080/1359432X.2018.1502171
- Gredler GR. (1993). Book reviews. [Review of the book Bullying at School: What We Know and What We Can Do by D Olweus]. Psychol Sch. 2003;40(6):699-700.doi:10.1002/pits.10114
- Enlow PT, McWhorter LG, Genuario K, Davis A. Supervisor–supervisee interactions: the importance of the supervisory working alliance. Train Educ Prof Psychol. 2019;13(3):206-211. doi:10.1037/tep0000243
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1,173-1,182. doi:10.1037/0022-3514.51.6.1173
- Rohland BM, Kruse GR, Rohrer JE. Validation of a single-item measure of burnout against the Maslach Burnout Inventory among physicians. Stress Health. 2004;20(2):75-79. doi:10.1002/smi.1002
- Sabella SA, Schultz JC, Landon TJ. Validation of a brief form of the Supervisory Working Alliance Inventory. Rehabil Couns Bull. 2020;63(2):115-124. doi:10.1177/0034355219846652
- Einarsen S, Hoel H, Notelaers G. Measuring exposure to bullying and harassment at work: validity, factor structure and psychometric properties of the Negative Acts Questionnaire-Revised. Work Stress. 2009;23(1):24-44. doi:10.1080/02678370902815673
- Terry DL, Williamson MLC. Bullying among medical residents: gender, social norms, and reporting behavior. PRiMER. 2022;6:17. doi:10.22454/PRiMER.2022.824936
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58(1):593-614. doi:10.1146/annurev.psych.58.110405.085542
- Bonifacino E, Ufomata EO, Farkas AH, Turner R, Corbelli JA. Mentorship of underrepresented physicians and trainees in academic medicine: a systematic review. J Gen Intern Med. 2021;36(4):1,023-1,034. doi:10.1007/s11606-020-06478-7
- Han S, Shanafelt TD, Sinsky CA, et al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med. 2019;170(11):784-790. doi:10.7326/M18-1422
Lead Author
Danielle L. Terry, PhD, ABPP
Affiliations: Behavioral Science Department, Guthrie Robert Packer Hospital, Sayre, PA
Co-Authors
Kartik Moza, MD - Behavioral Science Department, Guthrie Robert Packer Hospital, Sayre, PA
Corresponding Author
Danielle L. Terry, PhD, ABPP
Correspondence: Behavioral Science Department, Guthrie Robert Packer Hospital, Sayre, PA
Email: Danielle.terry@guthrie.org
Fetching other articles... 
Loading the comment form... 
Submitting your comment... 


There are no comments for this article.