Introduction: Clinical teaching cases are a cornerstone of health professions education programs, but cases historically have lacked diversity and have the potential to reinforce essentialism. In this article, we describe the creation, implementation, and feasibility assessment of a professional development workshop aimed at integrating an existing bias reduction tool into discussion and revision of teaching cases.
Methods: Six 60-minute workshops were held introducing “The Race and Culture Guide for Editors of Teaching Cases” to different health profession education programs wherein all participants worked in small groups to critique and edit two sample teaching cases. To assess initial feasibility, facilitators completed a facilitator evaluation survey to capture experiences after the first three workshops. Due to positive feedback, workshops were continued, and participants completed a participant evaluation survey to understand learner impact.
Results: Facilitators (n=6) identified the workshop as addressing an important need, highlighted the value in small-group format, and noted their ability to facilitate future sessions. Participants (n=18) rated the workshop as useful, effective at challenging biases, and would recommend the workshop to others.
Conclusion: The purpose of this study was to understand the feasibility of implementing a discussion-based workshop integrating a bias reduction tool. Initial feasibility and acceptability assessments demonstrate that this workshop can be useful in addressing a current need, is feasible to implement, and engaging to learners.
Medical students have called for curricula addressing structural racism as a root cause of health disparities in the United States.1-3 An increasing number of medical schools are developing curricula using social and structural determinants of health (SSDOH) and integrating these concepts into clinical teaching cases.4-7 These cases can, however, reinforce essentialist ideas when presenting disparate health outcomes among patients with minoritized identities.8-10 Inadequacies in SSDOH education may be attributed to the fact that most faculty are not adequately trained to teach about race and racism.11 Faculty should receive training on integrating SSDOH into teaching cases in a way that does not perpetuate harmful stereotypes.11
Krishnan and colleagues published the “Race and Culture Guide (RCG),” a detailed checklist describing how to review and edit teaching cases for bias and stereotypes.12 We designed and implemented a modifiable, interactive, and action-focused workshop that teaches participants how to apply this tool. The goal of this workshop was to improve participants’ attitudes and skills related to teaching about racism and SSDOH in case-based learning. We included assessments of participants and facilitators to evaluate feasibility and acceptability of implementing this professional development workshop.
We hosted six 60-minute workshops (2020-2022) for multiple health professions education programs (medicine, clinical psychology, and physician assistant practice) at a large Midwestern university. Before the workshop, all participants (n=34) were asked to read “Addressing Race, Culture, and Structural Inequality in Medical Education: A Guide for Revising Teaching Cases.”12 The workshops were cofacilitated by medical students completing a year-long academic medicine rotation (n=6), faculty in medicine and clinical psychology (n=4), and medical school administrators (n=2). The workshop began with an introduction on SSDOH and structural competency.4 Then, in breakout groups, all participants revised two provided teaching cases. Small groups then reconvened and shared highlights from their discussion.
To understand the feasibility of implementation of this discussion-based workshop, we completed a two-stage sequential feasibility review, first assessing facilitator experience and then participant engagement. After the first three workshops, facilitators completed a facilitator evaluation survey. We then implemented three additional workshops after which participants completed a participant evaluation survey. All surveys included open-ended and single-item Likert-type response questions. All workshop materials are available in the STFM Resource Library.13
We calculated descriptive statistics and coded open-ended responses using thematic analysis. To analyze the open-ended responses, a single study author coded responses using a modified grounded theory approach.14,15 Coding occurred in three phases: line-by-line coding, assessing saturation and establishing relationships between the codes, and finally forming categories. We used a paired-samples t test to determine whether participants reported significant changes in self-perceived confidence identifying bias in teaching cases. We asked learners to rate their confidence in identifying biases in teaching cases before and after the session. Previous research suggests that this retrospective pretest methodology is beneficial for reducing response-shift bias.16,17 This bias can threaten the validity of traditional pretest/posttest methodologies, especially when asking participants to self-report attitude, knowledge, or behavior.16
The participating institution's Office of Research Compliance determined this study to be exempt from review.
Facilitator Assessment
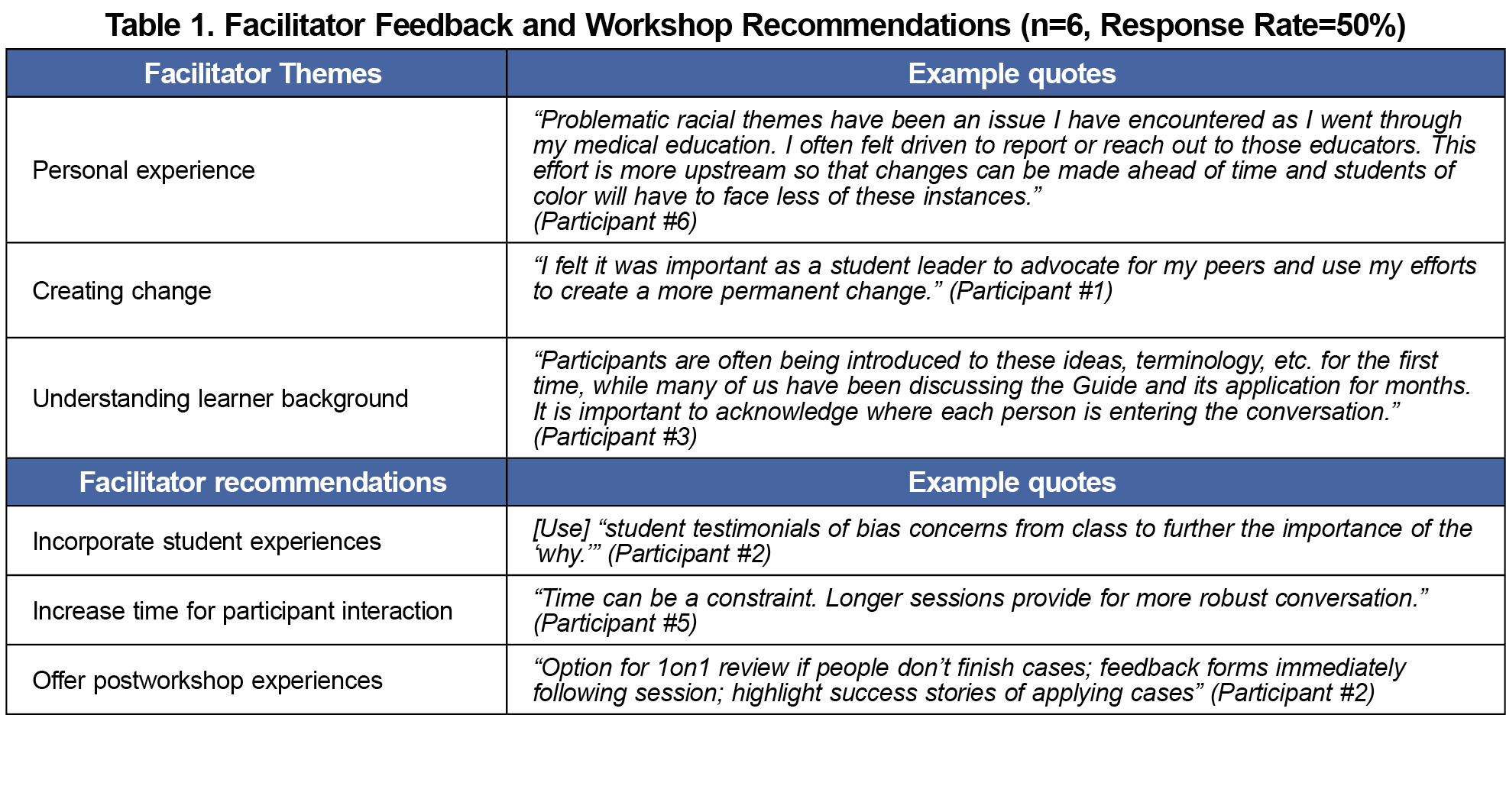
Six of the 12 facilitators completed surveys (50% response rate). Facilitators reported willingness to cofacilitate future workshops (M=4.33, SD=0.82). Facilitators were comfortable cofacilitating the content presentation (M=4.50, SD=0.55) and breakout sessions (M=4.00, SD=0.50). All items included a 5-point response scale. Table 1 shows themes on feedback and recommendations.
Participant Assessment
Thirty-four participants attended the workshops offered to health professions education programs. The 18 participants who completed the evaluation survey (53% response rate) included students (n=9), clinical faculty (n=6), nonclinical faculty (n=2), and staff/administrator (n=1).
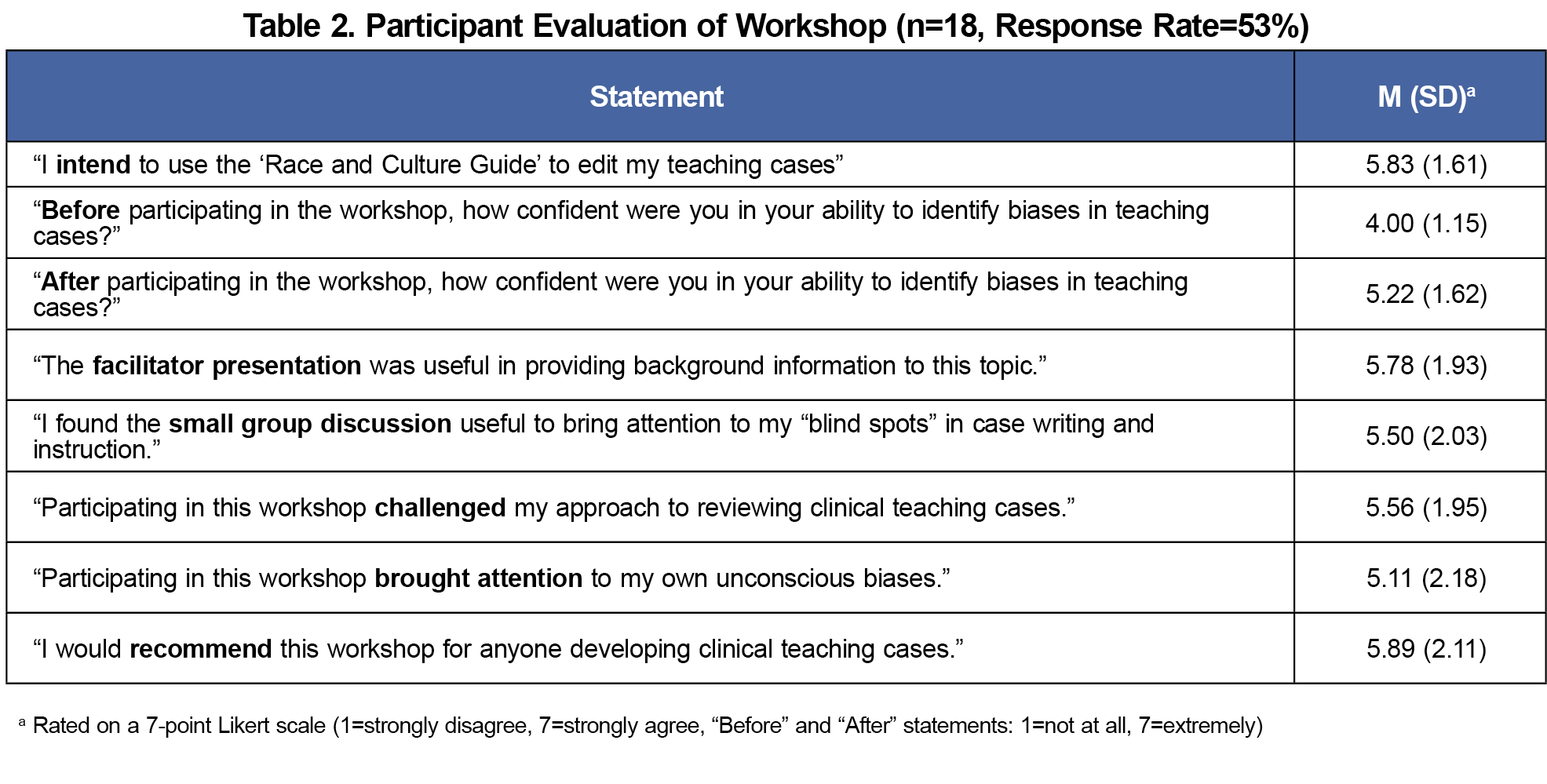
Participants reported increases in self-confidence (t[17]=4.89, P=.0001, d=0.87). Most (78%) participants reported intentions to edit their teaching cases following the workshop. Participants also reported small group discussion brought attention to “blind spots” in case writing and instruction, challenged their approach to reviewing teaching cases, brought attention to their own biases, and would recommend the workshop to others (Table 2).
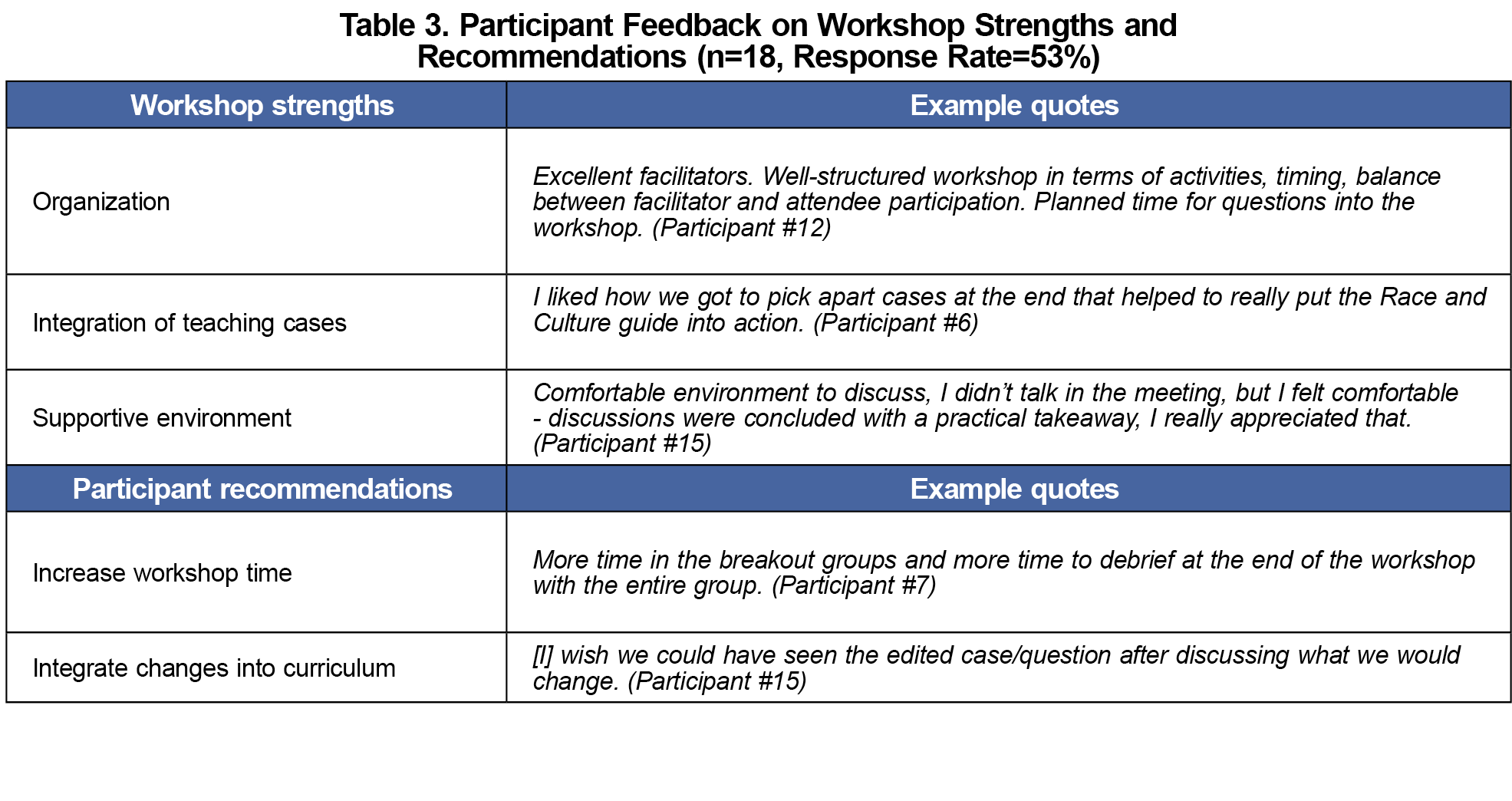
Participants noted several strengths of the workshop, including format, integration of teaching cases, time dedicated to discussion, and creation of a safe space for dialogue. Participants also suggested important areas for expansion and improvement (Table 3).
Most medical education faculty lack the training needed to effectively address race and racism in patient cases.11 We developed and assessed the acceptability and feasibility of implementing a novel, structured workshop using a published bias reduction tool. We found this workshop was feasible to implement across multiple health professions settings and is highly adaptable.
Facilitator and participant feedback suggested this workshop is needed within health professions education. Overarching themes included the importance of the content related to bias in teaching cases and identifying concrete ways to make curricular changes. Participants and facilitators valued the workshop for its focus on incorporating diverse perspectives and addressing challenging topics. Overall, participants found the workshop valuable and expressed a desire for additional training and more opportunities to practice the skills learned. Participants intended to use the RCG to edit future teaching cases, which suggests the workshop may influence future behavior.
The generalizability of our findings is limited by the small sample size and use of single-item measures. Our findings may also be affected by bias related to participants’ recall of prior and current confidence or selection and nonresponse bias. Additionally, relying only on participant reaction (Kirkpatrick Model [KM] level 1) is a significant limitation of our study.18 Future research will need to assess the impact of this workshop on educator confidence (KM level 2) and behavior change (KM level 3) in terms of using the RCG in practice and examine whether use of the RCG is associated with less stigmatizing language in teaching cases (KM level 4).18
The workshop provided a space to develop shared language among students and medical educators, allowed for discussion on the impact of race and cultural biases within teaching cases, and created a mechanism to collaboratively edit clinical teaching cases. Our assessment demonstrates that this workshop addresses an important need within health professions education by building faculty capacity to address health inequity and to not further harmful stereotypes in case-based teaching.
Acknowledgments
Presentations: Preliminary results of this manuscript were presented via oral presentation “Addressing Structural Inequality in Medical Education Cases: Applying The Race And Culture Guide” at American Association of Colleges of Osteopathic Medicine Educating Leaders Conference (April 20, 2021; virtual conference).
References
- Paul DW Jr, Knight KR, Campbell A, Aronson L. Beyond a moment - reckoning with our history and embracing antiracism in medicine. N Engl J Med. 2020;383(15):1404-1406. doi:10.1056/NEJMp2021812
- Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453-1463. doi:10.1016/S0140-6736(17)30569-X
- Bassett MT. #BlackLivesMatter--a challenge to the medical and public health communities. N Engl J Med. 2015;372(12):1085-1087. doi:10.1056/NEJMp1500529
- Metzl JM, Hansen H. Structural competency: theorizing a new medical engagement with stigma and inequality. Soc Sci Med. 2014;103(103):126-133. doi:10.1016/j.socscimed.2013.06.032
- McLean SF. Case-Based Learning and its application in medical and health-care fields: a review of worldwide literature. J Med Educ Curric Dev. 2016;3:JMECD.S20377. doi:10.4137/JMECD.S20377
- Solar O, Irwin A. A Conceptual Framework for Action on the Social Determinants of Health.World Health Organization; 2010:79. Accessed December 27, 2021. https://www.who.int/sdhconference/resources/ConceptualframeworkforactiononSDH_eng.pdf
- U.S. Department of Health and Human Services. Social Determinants of Health. Healthy People 2030. Accessed December 23, 2021. https://health.gov/healthypeople/objectives-and-data/social-determinants-health
- Wear D. Insurgent multiculturalism: rethinking how and why we teach culture in medical education. Acad Med. 2003;78(6):549-554. doi:10.1097/00001888-200306000-00002
- Edgoose J, Brown Speights J, White-Davis T, et al. Teaching about racism in medical education: a mixed-method analysis of a train-the-trainer faculty development workshop. Fam Med. 2021;53(1):23-31. doi:10.22454/FamMed.2021.408300
- Amutah C, Greenidge K, Mante A, et al. misrepresenting race - the role of medical schools in propagating physician bias. N Engl J Med. 2021;384(9):872-878. doi:10.1056/NEJMms2025768
- Acosta D, Ackerman-Barger K. Breaking the silence: time to talk about race and racism. Acad Med. 2017;92(3):285-288. doi:10.1097/ACM.0000000000001416
- Krishnan A, Rabinowitz M, Ziminsky A, Scott SM, Chretien KC. Addressing race, culture, and structural inequality in medical education: a guide for revising teaching cases. Acad Med. 2019;94(4):550-555. doi:10.1097/ACM.0000000000002589
- Vagedes R, Franz B, Kerr A, et al. Professional Development Workshop: Applying the Race and Culture Guide to Reduce Bias in Medical Teaching Cases. STFM Resource Library. Published 2023. Accessed February 3, 2024. https://resourcelibrary.stfm.org/viewdocument/professional-development-workshop?CommunityKey=2751b51d-483f-45e2-81de-4faced0a290a&tab=librarydocuments
- Charmaz K. Constructing Grounded Theory: A Practical Guide through Qualitative Analysis. Sage. 2006.
- Chun Tie Y, Birks M, Francis K. Grounded theory research: A design framework for novice researchers. SAGE Open Med. 2019;7:2050312118822927. doi:10.1177/2050312118822927
- Pratt CC, McGuigan WM, Katzev AR. Measuring program outcomes: using retrospective pretest methodology. Am J Eval. 2000;21(3):341-349. doi:10.1177/109821400002100305
- Howard GS, Dailey PR. Response-shift bias: A source of contamination of self-report measures. J Appl Psychol. 1979;64(2):144-150. doi:10.1037/0021-9010.64.2.144
- The Kirkpatrick Model. Kirkpatrick Partners, LLC. Accessed December 8, 2023. https://www.kirkpatrickpartners.com/the-kirkpatrick-model/



There are no comments for this article.