Introduction: Displacement due to conflict is a hallmark of humanitarian crises and traumatized survivors face unique health challenges. The purpose of this study is to investigate the health factors impacting Arab refugees in the United States and Canada, with a focus on the mental health challenges that further complicate the health care experiences of this vulnerable population.
Methods: A scoping review was conducted using a protocol based on the Preferred Reporting items for Systematic Reviews and Meta-Analyses (PRISMA) reporting guidelines. We established eligibility criteria for selecting original peer-reviewed articles published in English between January 1, 1990 and December 31, 2024. The search utilized five databases (PubMed, Embase, Scopus, CINAHL Complete, and ProQuest). We selected 31 articles based on study criteria.
Results: The literature consistently highlights a high burden of mental health disorders among Arab refugees—particularly posttraumatic stress disorder, depression, and anxiety. Additionally, despite insurance coverage, psychological service utilization remains low due to systemic health barriers.
Conclusion: Arab refugees in the United States and Canada face significant mental health challenges that are compounded by barriers such as stigma, language obstacles, and inadequate access to culturally sensitive care. Addressing these specific needs can improve health outcomes at both individual and community levels.
Arab refugees represent a highly marginalized group within the United States and Canada, having predominantly fled war, political oppression, and persecution over the past decade.1 The National Health Interview Survey revealed that individuals of Middle Eastern descent report higher levels of emotional distress compared to US-born, non-Hispanic Whites, yet Arab immigrants utilize mental health services at notably lower rates.2 The purpose of this study is to investigate the health factors impacting Arab refugees in the United States and Canada.
Family medicine, as the cornerstone of primary care, plays a crucial role in addressing these disparities. By incorporating culturally competent practices that recognize the specific health needs of Arab refugees, including the psychosocial impacts of displacement and the need for sensitive communication, family medicine can improve health care delivery.3-5 Enhancing training on cultural sensitivity, communication skills, and understanding the unique challenges faced by this population may strengthen patient-provider relationships, increase health care service utilization, and ultimately lead to better health outcomes for Arab refugee populations.3-6
We conducted a scoping review under an evidence-based set of items for reporting, known as the Preferred Reporting Items for Systemic Reviews and Meta-Analyses (PRISMA).7 To identify relevant studies, we used the following search query: (arabs OR arab) AND (refugee) AND (America OR American OR Canada OR Canadian) AND (1990/1/1:2024/12/31[pdat]). This query was utilized in five databases (PubMed, Embase, Scopus, CINAHL Complete, and ProQuest) to collect studies relevant to our target population.
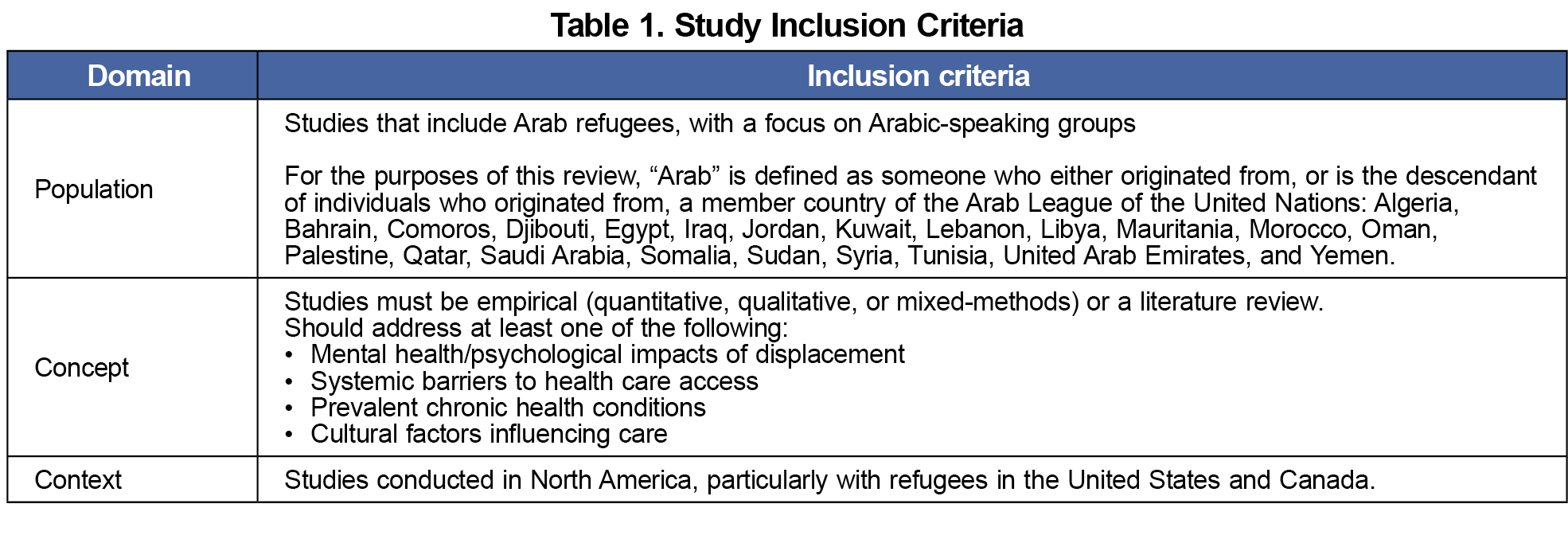
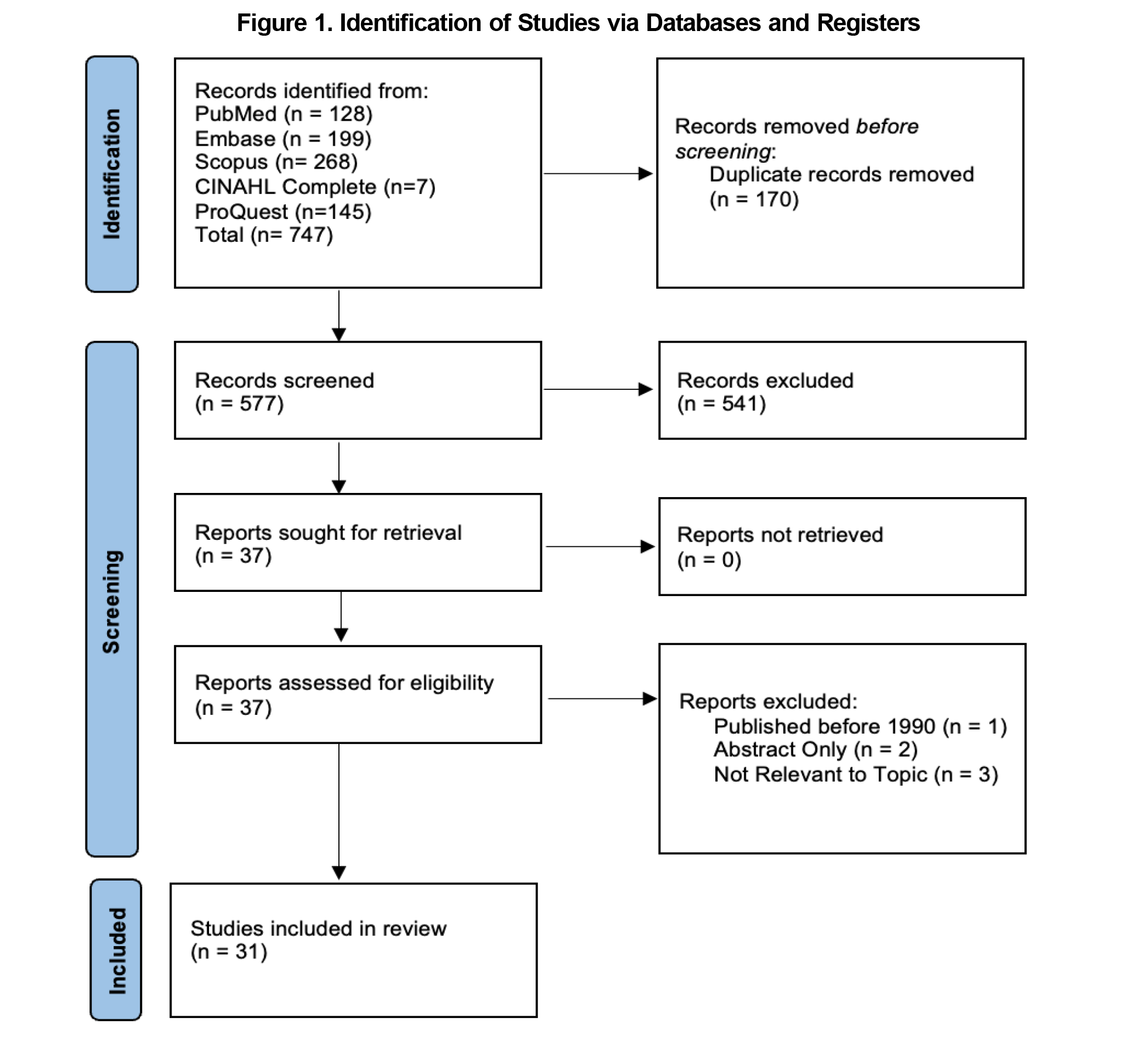
We identified 747 studies based on the search query. After 170 duplicates were removed, 577 records were screened. The study selection process involved two stages. In the first stage, a list of inclusion criteria using the Population, Concept, Context model for scoping reviews7 was agreed upon to establish study scope and minimize author bias (Table 1). In this process, we chose to analyze studies that focused primarily on individuals who self-identified as Arab or Arabic-speaking to maintain linguistic and regional specificity. The inclusion criteria were then used to manually screen articles by titles and abstracts for relevance. Studies were selected for full-text review by at least two authors, with discussion to resolve differences. In the second stage, the final 37 reports were assessed for eligibility. Study exclusion criteria are detailed in Figure 1. We included 31 studies in the review based on these criteria. Although the primary focus of this review was Arab refugees in the United States, six Canadian studies were included to provide a broader North American perspective across similar western health care contexts. From each included study, we extracted the following information:
- Reference citation,
- Background,
- Methods/intervention (including number of participants, population, and study design),
- Results,
- Conclusion, and
- Any additional relevant information.
Each study was also categorized based on the following concept inclusion criteria:
- Mental health and psychological impacts of displacement,
- Systemic barriers to health care access,
- Prevalent chronic health conditions, and
- Cultural factors influencing care.
When a study covered more than one concept, this was also noted. The results were published in the STFM Resource Library.8 References were managed using Endnote Online Classic software (Clarivate Analytics).
A consistent finding across the literature indicates a significantly high prevalence of mental health disorders among Arab refugees, including posttraumatic stress disorder, depression, and anxiety.2,4,9 For example, Iraqi children, especially those with parents who are torture survivors, exhibit heightened vulnerability to mental health issues.10 In one study surveying 366 Iraqi refugees to the United States, it was found that 49% of the participants reported depression, and 50% noted psychological distress and trauma symptoms.11
Key contributors to poor mental health within the refugee population include language barriers, lack of knowledge about available resources, and micro/macroaggressions from the host community.9 Access to mental health services is often inadequate, with many services lacking cultural and linguistic relevance.12,13 Studies link these mental health burdens to psychosomatic symptoms and low self-rated health, particularly among women and individuals with lower socioeconomic status.14 In addition, despite having health insurance, many Arab immigrants are underutilizing psychological services, indicating that there may be several systemic barriers—collectively referred to as inadequate support systems. These include the lack of culturally and linguistically appropriate care, limited awareness of available mental health services, and insufficient integration of community-based support networks with formal health care systems.6,15 There is also a cultural stigma surrounding discussing one’s personal issues with someone outside the family, rooted in beliefs that associate mental health struggles with personal or familial shame.15
As highlighted in this scoping review, mental health challenges among Arab refugees are severe and multifaceted, with high levels of emotional distress exacerbated by the trauma of displacement, stigma surrounding mental health, and barriers to care.2,4,9,12,16-18 Culturally-sensitive care by health care providers is critical, as language barriers and lack of culturally competent services severely limit refugees' ability to utilize mental health support.5,13,14,19-22 Despite these findings, some methodological weaknesses exist, including potential selection bias in the literature reviewed and the lack of longitudinal studies tracking the long-term effectiveness of interventions. Additionally, the reliance on self-reported data may introduce biases related to stigma or underreporting of mental health issues. Given the nature of a scoping review, a formal risk of bias assessment was not conducted, and the study focused on breadth rather than depth of available evidence. As such, comprehensive reviews should integrate these risk assessments and explore additional factors influencing access to and utilization of mental health care for Arab and Arabic-speaking refugee populations in the United States and Canada. Future research should focus on longitudinal studies to evaluate the long-term impact of more culturally-sensitive interventions on mental health outcomes, helping shape more effective and sustainable approaches for Arab refugee care.
Acknowledgments
Presentations: This study was presented at the following venues:
- National Arab American Medical Association National Convention (August 2024, Chicago IL)
- ACCESS Arab Health Summit (October 2024, Dearborn, MI)
Conflict Disclosure: The authors have no conflicts of interest to disclose.
References
- Gibson I. Annual Flow Report Refugees and Asylees: 2022.2023. Accessed July 10, 2025. https://ohss.dhs.gov/sites/default/files/2024-03/2023_0818_plcy_refugees_and_asylees_fy2022_v2_0.pdf
- Pampati S, Alattar Z, Cordoba E, Tariq M, Mendes de Leon C. Mental health outcomes among Arab refugees, immigrants, and U.S. born Arab Americans in Southeast Michigan: a cross-sectional study. BMC Psychiatry. 2018;18(1):379. doi:10.1186/s12888-018-1948-8
- Bridi L, Albahsahli B, Bencheikh N, et al. Barriers and facilitators to self-measured blood pressure monitoring among US-resettled Arab refugees with hypertension: a qualitative study. BMC Prim Care. 2023;24(1):256. doi:10.1186/s12875-023-02215-1
- Elshahat S, Moffat T. Mental health triggers and protective factors among Arabic-speaking immigrants and refugees in North America: a scoping review. J Immigr Minor Health. 2022;24(2):489-505. doi:10.1007/s10903-021-01215-6
- Namak SY, Kirk JK. Maternal healthcare challenges confronting Arab Muslim refugee women in Triad North Carolina. N C Med J. 2019;80(2):116-119. doi:10.18043/ncm.80.2.116
- Elsouhag D, Arnetz B, Jamil H, Lumley MA, Broadbridge CL, Arnetz J. Factors associated with healthcare utilization among Arab immigrants and Iraqi refugees. J Immigr Minor Health. 2015;17(5):1305-1312. doi:10.1007/s10903-014-0119-3
- Peters M, Godfrey C, McInerney P, Munn Z, Tricco A, Khalil H. Scoping reviews. In: Aromataris E, Munn Z, eds. JBI Manual for Evidence Synthesis.JBI; 2020:chap 10, doi:10.46658/JBIMES-20-12
- Berry Y. Determinants of Health Among Arab Refugees: Impact of Conflict-Driven Displacement (XLSX document). Retrieved from The STFM Resource Library: https://resourcelibrary.stfm.org/viewdocument/determinants-of-health-among-arab-r?CommunityKey=2751b51d-483f-45e2-81de-4faced0a290a&tab=librarydocuments
- Elshahat S, Moffat T, Iqbal BK, et al. ‘I thought we would be cherished and safe here’: understanding the multi-faceted nature of mental health among Arab immigrants/refugees in Ontario Canada - the CAN-HEAL study. Soc Psychiatry Psychiatr Epidemiol. 2025;60:163-179. doi:10.1007/s00127-024-02668-4
- Trentacosta CJ, McLear CM, Ziadni MS, Lumley MA, Arfken CL. Potentially traumatic events and mental health problems among children of Iraqi refugees: the roles of relationships with parents and feelings about school. Am J Orthopsychiatry. 2016;86(4):384-392. doi:10.1037/ort0000186
- Taylor EM, Yanni EA, Pezzi C, et al. Physical and mental health status of Iraqi refugees resettled in the United States. J Immigr Minor Health. 2014;16(6):1130-1137. doi:10.1007/s10903-013-9893-6
- al-Krenawi A, Graham JR. Culturally sensitive social work practice with Arab clients in mental health settings. Health Soc Work. 2000;25(1):9-22. doi:10.1093/hsw/25.1.9
- Thomson MS, Chaze F, George U, Guruge S. Improving immigrant populations’ access to mental health services in Canada: a review of barriers and recommendations. J Immigr Minor Health. 2015;17(6):1895-1905. doi:10.1007/s10903-015-0175-3
- Abdulrahim S, Baker W. Differences in self-rated health by immigrant status and language preference among Arab Americans in the Detroit Metropolitan Area. Soc Sci Med. 2009;68(12):2097-2103. doi:10.1016/j.socscimed.2009.04.017
- Wright AM, Aldhalimi A, Lumley MA, et al. Determinants of resource needs and utilization among refugees over time. Soc Psychiatry Psychiatr Epidemiol. 2016;51(4):539-549. doi:10.1007/s00127-015-1121-3
- Amer MM, Hovey JD. Socio-demographic differences in acculturation and mental health for a sample of 2nd generation/early immigrant Arab Americans. J Immigr Minor Health. 2007;9(4):335-347. doi:10.1007/s10903-007-9045-y
- Jamil H, Hakim-Larson J, Farrag M, Kafaji T, Jamil LH, Hammad A. Medical complaints among Iraqi American refugees with mental disorders. J Immigr Health. 2005;7(3):145-152. doi:10.1007/s10903-005-3671-z
- Slewa-Younan S, Uribe Guajardo MG, Heriseanu A, Hasan T. A systematic review of post-traumatic stress disorder and depression amongst Iraqi refugees located in Western countries. J Immigr Minor Health. 2015;17(4):1231-1239. doi:10.1007/s10903-014-0046-3
- Abu-Ras W. Cultural beliefs and service utilization by battered Arab immigrant women. Violence Against Women. 2007;13(10):1002-1028. doi:10.1177/1077801207306019
- Guruge S, Sidani S, Illesinghe V, et al. Healthcare needs and health service utilization by Syrian refugee women in Toronto. Confl Health. 2018;12:46. doi:10.1186/s13031-018-0181-x
- Inhorn MC, Fakih MH. Arab Americans, African Americans, and infertility: barriers to reproduction and medical care. Fertil Steril. 2006;85(4):844-852. doi:10.1016/j.fertnstert.2005.10.029
- Mowafi H. Conflict, displacement and health in the Middle East. Glob Public Health. 2011;6(5):472-487. doi:10.1080/17441692.2011.570358



There are no comments for this article.