Background and Objectives: As the opioid epidemic continues in the United States, neonatal opioid withdrawal syndrome (NOWS) prevalence is rising. Research has shown positive outcomes from protocols to assess and treat infants with NOWS. A medical student preclinical elective was created to teach students about NOWS, substance use disorders (SUDs), social services, and trauma-informed care. This involved didactics, hospital volunteer experience, and reflection essays. Our study aimed to determine the impact of the course on medical student attitudes and beliefs toward people with SUDs.
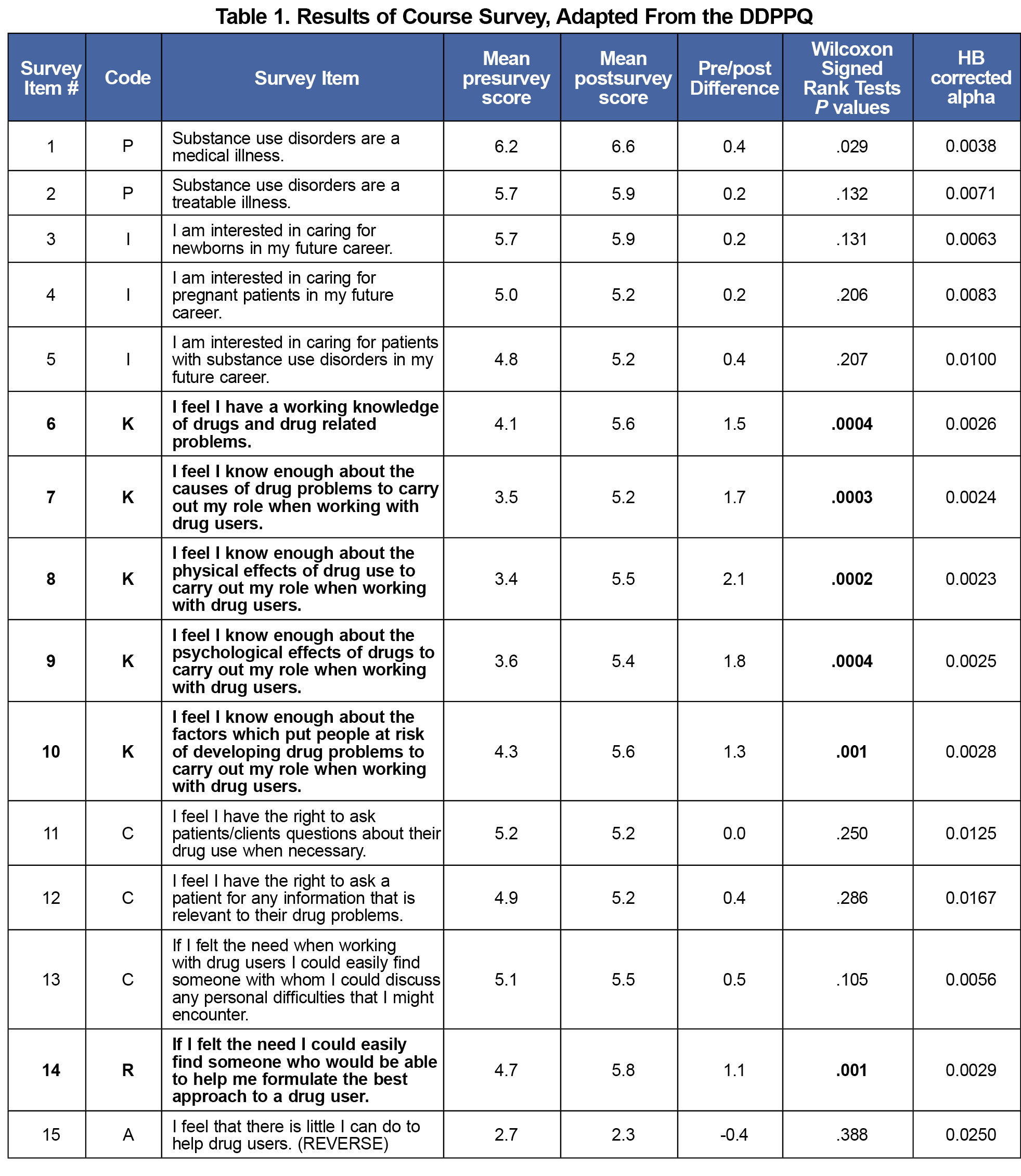
Methods: Enrolled preclinical medical students completed a pre- and postcourse survey, an adapted 22 question version of the Drug and Drug Problems Perceptions Questionnaire (DDPPQ). We analyzed results through a Wilcoxon signed ranked test and we performed a thematic analysis on students’ reflective essays.
Results: Twenty students completed the course during the study, with a 95% survey response rate. Survey results showed a statistically significant change between pre- and postcourse responses for seven of the 22 questions, showing positive changes in self-perceived knowledge, respect, and ability to find help. Reflective essays identified major themes of professional identity formation, interdisciplinary values, patient/family perspectives, empathy, and increased knowledge and confidence.
Conclusions: Implementing an elective that combines didactics and volunteer experiences can improve medical students’ self-reported perceptions of people with SUD and interest in primary care and addiction medicine, a key to continued handling of the opioid epidemic.
Neonatal opioid withdrawal syndrome (NOWS) has become more common as the rate of opioid use in pregnant people more than doubled from 2010 to 2017. 1,2 Stigma from medical providers toward patients who use substances negatively impacts health care outcomes, particularly in pregnant people with limited prenatal care.3,4 Previous studies have shown that few trainees felt their training on substance use disorders (SUD) and trauma-informed care is adequate to deliver high-quality care to dyads affected by SUD.5 Barriers include the lack of physician role models and limited educational time, 6,7 but even brief curricular interventions have improved student attitudes. 8-11
One NOWS protocol with nonpharmacologic therapies and a simplified approach to assessing infants, called “Eat, Sleep, Console” (ESC), can positively affect outcomes. Compared to Finnegan scoring, ESC dramatically reduces both the proportion of infants treated with morphine and the average length of stay, without increasing readmission rates or adverse events. 12-15 The shift from older protocols created an opportunity to educate medical students to provide better patient-centered care.
This pass-fail, preclinical elective combines five 1-hour didactics with case-based teaching, an interdisciplinary panel, and volunteer clinical experiences. The elective was started in January 2019. Students complete this optional course alongside the required preclinical 18-month curriculum. The course was created by resident and attending physicians in pediatrics, family medicine (FM), and addiction medicine, as well as maternity care nurses and medical students. Didactics, delivered across 3 months, covered NOWS physiology and treatment, standard newborn soothing techniques, trauma-informed care, and medication treatment for opioid use disorder in pregnancy. The panel, comprised of inpatient social workers, a certified drug and alcohol counselor (CADC), and a doula, discussed relevant social services. Students were required to serve at least two 2-hour volunteer shifts per month for 6 months, to assist nurses and parents with soothing techniques and ESC care for NOWS in the Neonatal Intensive Care Unit (NICU), mother-baby unit, and inpatient pediatric units. Finally, students wrote a 400-600 word reflective essay at the completion of the course on anything they learned that surprised them or changed their perspectives, meaningful interactions during volunteer shifts, and what (if any) experiences with SUD or maternal infant care they would like to pursue in their future.
We hypothesized that education and interprofessional exposure to NOWS would positively impact the perceived knowledge, attitudes, and beliefs of students toward people with SUD. This would augment earlier evidence by adding a multimodal analysis and interdisciplinary focus. 16
After obtaining institutional review board exemption, we conducted a mixed methods analysis for the first two cohorts (n=20). At their first and last course sessions, students filled out a survey (Table 1), adapted from the validated Drug and Drug Problems Perceptions Questionnaire (DDPPQ). The 20-item Likert scale questionnaire was designed to measure attitudes of professionals who work with people who use substances.17 Three questions were removed and five were added on student career goal intent to fit the scope of the elective (see Appendix 1). We analyzed responses through a Wilcoxon signed rank test using a Holm-Bonferroni correction for multiple comparisons.
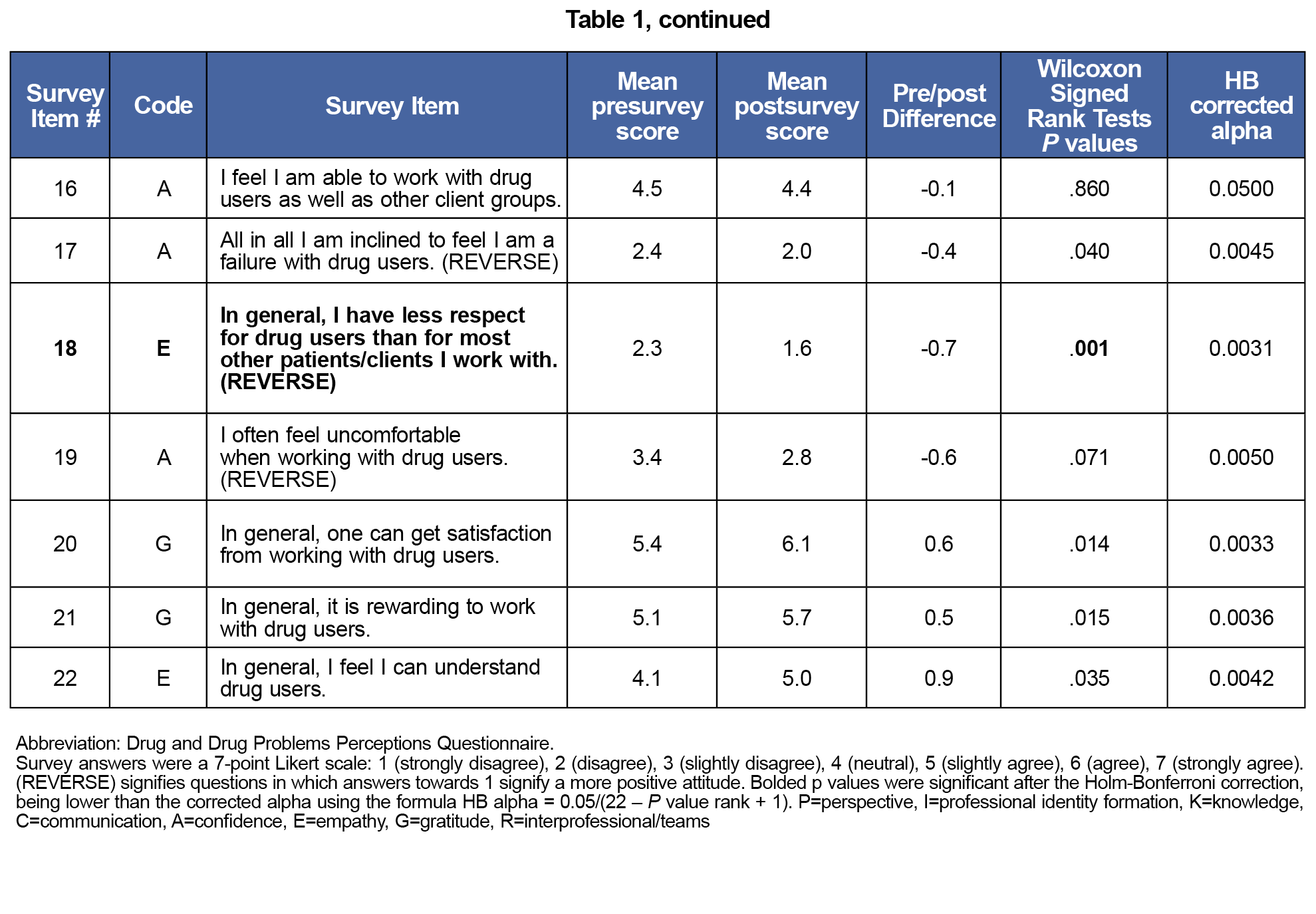
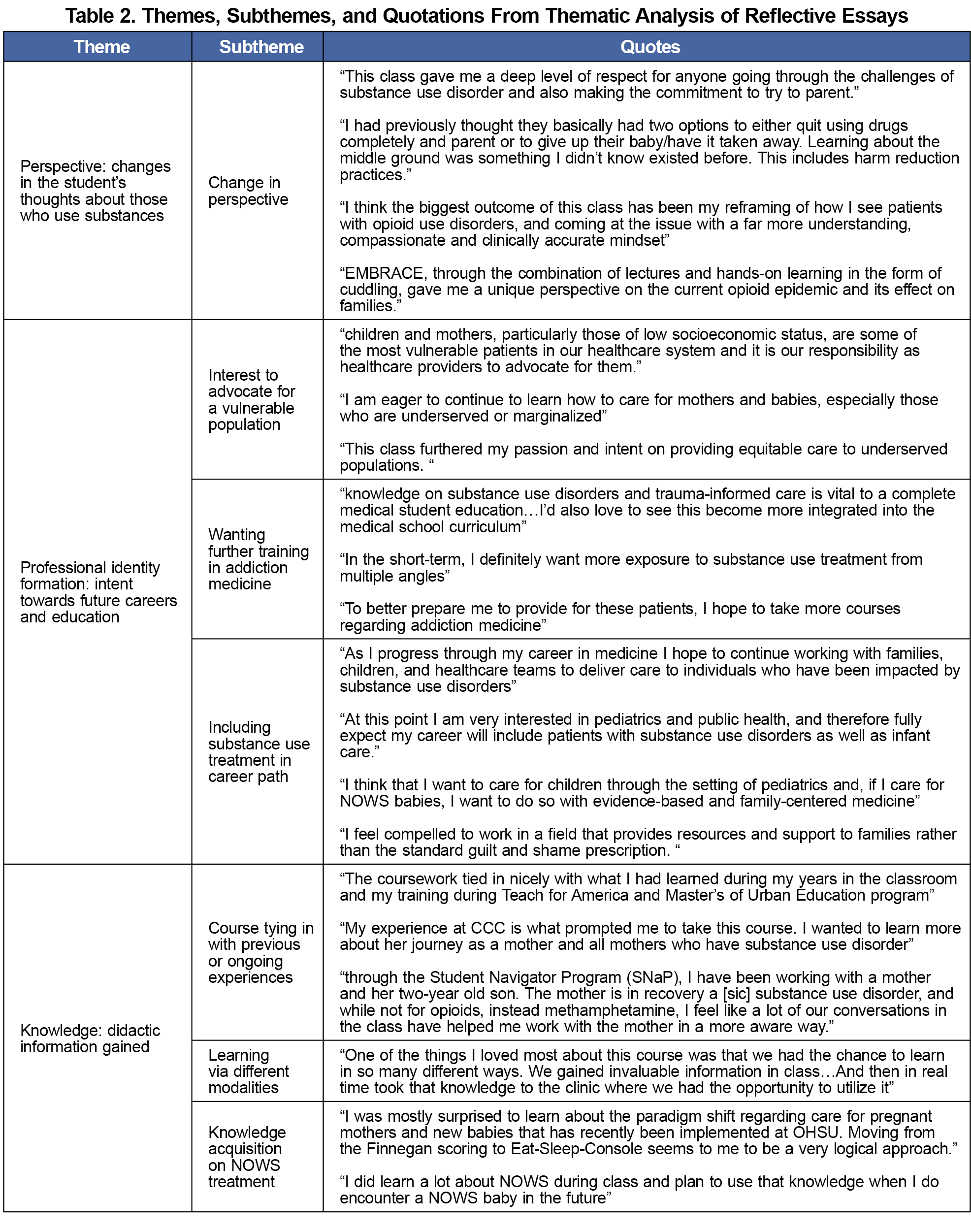
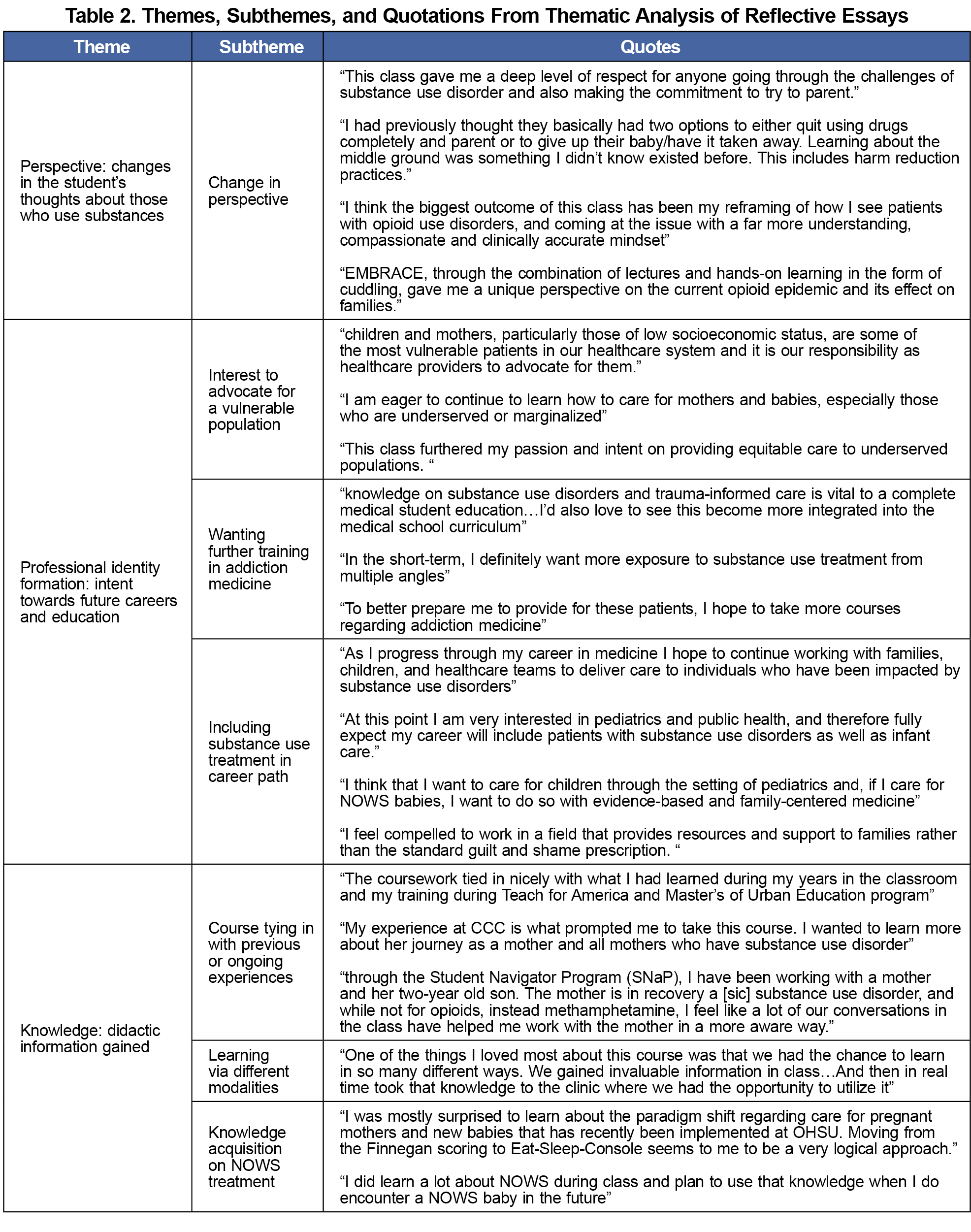
A team of seven reviewers involved in the course conducted an inductive qualitative analysis on the 10 essays from the first term to identify recurring themes, which were then organized into a code set applied to the second term’s 10 essays and to survey items, to analyze response trends.
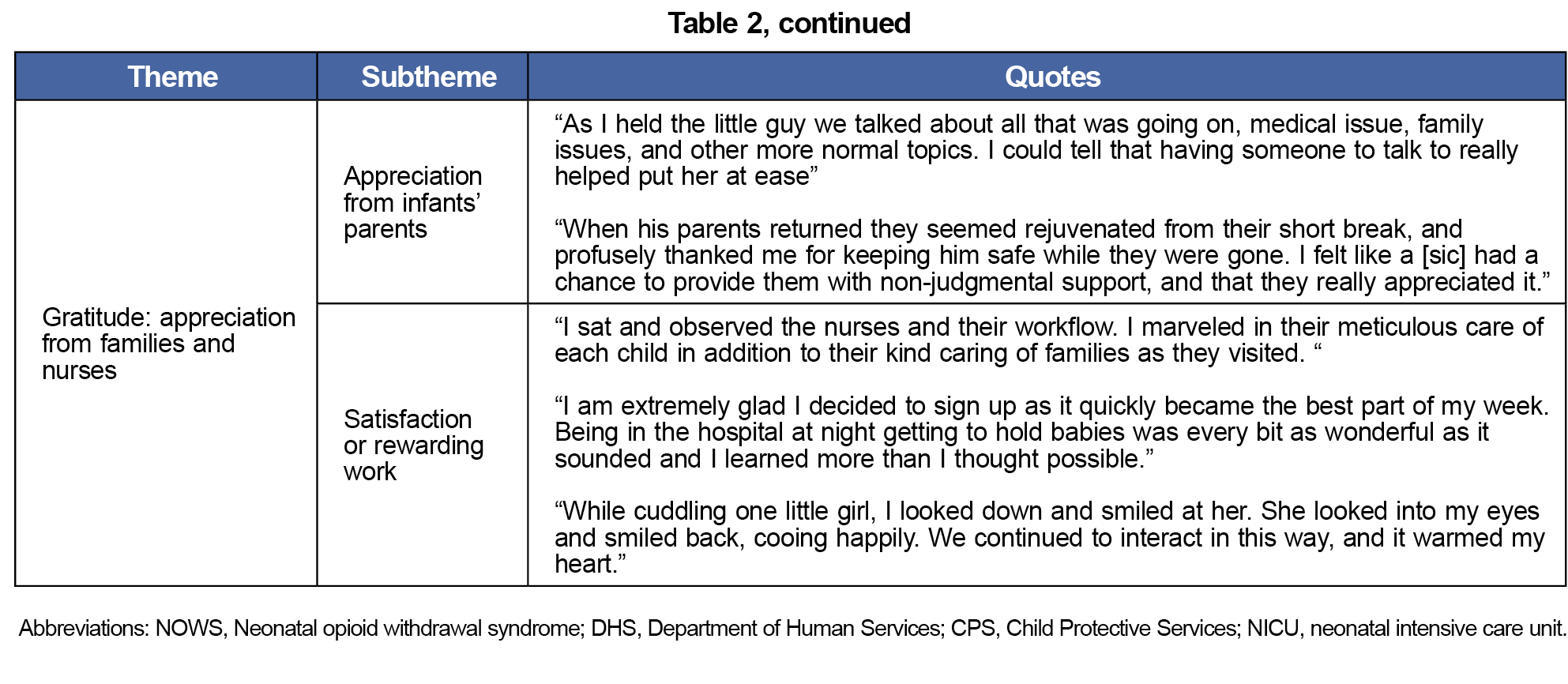
Of the 20 participants, there was a 95% paired survey completion rate. The qualitative analysis identified several major themes: perspective, professional identity formation, knowledge, confidence, empathy, gratitude, and interprofessionalism (Table 2).
The quantitative analysis revealed a statistically significant difference in seven survey items, shifting toward more positive perceptions and attitudes (Table 1). These included improved self-perceived knowledge and ability to find help for patient care, and increased respect for patients.
Finally, the combined analysis showed a subset of students who indicated lower confidence after the course in their ability to work with this population. Compared with students who had neutral or positive changes in their confidence, this group wrote more in their essays about implicit bias, and none discussed prior experience caring for people with SUD in their reflection essay.
Overall, this course improved many facets of medical students’ perspectives toward people with SUDs, showing that a course incorporating pregnancy and neonatal care can be effective, supporting findings from previously published data on SUD curricula. Quantitative improvement in attitudes correlated with qualitative themes of empathy, bias recognition, desire for further training in addiction medicine, and intent to include SUD treatment in their career path.
Many students described the interdisciplinary panel as a meaningful experience that yielded greater understanding of the social context of families with NOWS infants. Insight into interdisciplinary work is especially important in addiction medicine to combat pre-existing feelings of hopelessness or futility of treatment. 18 Acknowledgement of trauma-informed care and students’ own implicit biases may have built empathy for patients’ experiences to improve care.
The students who enrolled in the EMBRACE elective were self-selected, often with pre-existing interest in newborn care and/or SUD. This limitation was accounted for by measuring the change in the pre- and postsurveys instead of the raw numbers. The DDPPQ was adapted and lost validity from prior use but was more applicable to students. While the course was pass/no-pass, the reflective essays were a required component of the course which may have influenced responses. The small class size limited the power of our research, but should serve as early data for future, larger studies. Given the limitations of self-assessment of knowledge and communication, future research should include objective evaluation such as observed clinical encounters.
Family physicians are uniquely positioned to expertly care for patients with SUDs and NOWS given their broad training that encompasses the complex dynamics, integrating knowledge on trauma, mental health and SUDs with training in prenatal, obstetric, and newborn care. The creation of this course modeled collaboration between disciplines to educate learners to provide evidence-based, compassionate care. Additional research is needed to understand the generalizability and long-term impact of these efforts.
Acknowledgments
Presentations: This study was presented at the Society of Teachers of Family Medicine Annual Spring Conference, May 3, 2021, virtual format.
Conflict Disclosure: The authors have no conflicts of interest to declare.
References
- Hirai AH, Ko JY, Owens PL, Stocks C, Patrick SW. Neonatal abstinence syndrome and maternal opioid-related diagnoses in the US, 2010-2017. JAMA. 2021;325(2):146-155. doi:10.1001/jama.2020.24991
- Sanjanwala AR, Lim G, Krans EE. Opioids and opioid use disorder in pregnancy. Obstet Gynecol Clin North Am. 2023;50(1):229-240. doi:10.1016/j.ogc.2022.10.015
- van Boekel LC, Brouwers EPM, van Weeghel J, Garretsen HFL. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: Systematic review. Drug and Alcohol Dependence. 2013/07/01/ 2013;131(1):23-35. doi:10.1016/j.drugalcdep.2013.02.018
- Schempf AH, Strobino DM. Drug use and limited prenatal care: an examination of responsible barriers. Am J Obstet Gynecol. Apr 2009;200(4):412 e1-10. doi:10.1016/j.ajog.2008.10.055
- Schiff DM, Zuckerman B, Wachman EM, Bair-Merritt M. Trainees’ knowledge, attitudes, and practices towards caring for the substance-exposed mother-infant dyad. Subst Abus. 2017;38(4):414-421. doi:10.1080/08897077.2017.1356423
- Miller NS, Sheppard LM, Colenda CC, Magen J. Why physicians are unprepared to treat patients who have alcohol- and drug-related disorders. Acad Med. 2001;76(5):410-418. doi:10.1097/00001888-200105000-00007
- Ram A, Chisolm MS. the time is now: improving substance abuse training in medical schools. Acad Psychiatry. 2016;40(3):454-460. doi:10.1007/s40596-015-0314-0
- Albright B, Skipper B, Riley S, Wilhelm P, Rayburn WF. Medical students’ comfort with pregnant women with substance-use disorders: a randomized educational study. Acad Psychiatry. 2012;36(6):457-460. doi:10.1176/appi.ap.11070134
- Bland E, Oppenheimer L, Brisson-Carroll G, Morel C, Holmes P, Gruslin A. Influence of an educational program on medical students’ attitudes to substance use disorders in pregnancy. Am J Drug Alcohol Abuse. 2001;27(3):483-490. doi:10.1081/ADA-100104513
- Dumenco L, Monteiro K, Collins S, et al. A qualitative analysis of interprofessional students’ perceptions toward patients with opioid use disorder after a patient panel experience. Subst Abus. 2019;40(2):125-131. doi:10.1080/08897077.2018.1546262
- Matthews J, Kadish W, Barrett SV, Mazor K, Field D, Jonassen J. The impact of a brief interclerkship about substance abuse on medical students’ skills. Acad Med. 2002;77(5):419-426. doi:10.1097/00001888-200205000-00017
- Grossman MR, Lipshaw MJ, Osborn RR, Berkwitt AK. A novel approach to assessing infants with neonatal abstinence syndrome. Hosp Pediatr. 2018;8(1):1-6. doi:10.1542/hpeds.2017-0128
- Grisham LM, Stephen MM, Coykendall MR, Kane MF, Maurer JA, Bader MY. Eat, sleep, console approach: a family-centered model for the treatment of neonatal abstinence syndrome. Adv Neonatal Care. 2019;19(2):138-144. doi:10.1097/ANC.0000000000000581
- Wachman EM, Grossman M, Schiff DM, et al. Quality improvement initiative to improve inpatient outcomes for Neonatal Abstinence Syndrome. J Perinatol. 2018;38(8):1114-1122. doi:10.1038/s41372-018-0109-8
- Young LW, Ounpraseuth ST, Merhar SL, et al; ACT NOW Collaborative. Eat, sleep, console approach or usual care for neonatal opioid withdrawal. N Engl J Med. 2023;388(25):2326-2337. doi:10.1056/NEJMoa2214470
- Gummadi NH, D’Amico M, Chandra P, et al. Impact of cuddler service-learning program in medical student education of opioid use disorder in pregnancy and neonatal opioid withdrawal syndrome. Subst Abus. 2021;42(4):951-956. doi:10.1080/08897077.2021.1900983
- Watson H, Maclaren W, Kerr S. Staff attitudes towards working with drug users: development of the Drug Problems Perceptions Questionnaire. Addiction. 2007;102(2):206-215. doi:10.1111/j.1360-0443.2006.01686.x
- Muzyk A, Mullan P, Andolsek KM, et al. An interprofessional substance use disorder course to improve students’ educational outcomes and patients’ treatment decisions. Acad Med. 2019;94(11):1792-1799. doi:10.1097/ACM.0000000000002854



There are no comments for this article.