Academic family medicine programs manage a substantial volume of electronic health record (EHR) tasks and must maintain productivity while residents complete external rotations with varied work hours. Faculty and resident providers carry a high administrative task burden in academic programs, consuming as much as 24% of work hours.1-3 Furthermore, EHR management contributes to burnout and worse patient outcomes.4-6 Team-based models can provide support. However, these models require additional clinical staff to complete tasks, and many workflows rely on physicians for final approval.7 Although EHR educational curricula, team-based inboxes, and coverage systems may have advantages, limited empirical evidence exists on how these may impact task management in residency-specific clinics.8,9 Thus, the current study aimed to investigate how task efficiency was influenced by using an assigned buddy with similar clinic responsibilities for a team-based approach in a residency outpatient clinic. Clinic personnel included in the pilot were resident physicians, faculty physicians, behavioral health faculty, and pharmacy faculty. We assessed outcomes related to task age and completion time.
LEARNER RESEARCH
Improving Workflow With a Task Buddy System in a Family Medicine Residency
Kathryn Hawks, DO | Brandi Dahl, PharmD | Alexander Melkonian, PhD | Laura Helmly, DO
PRiMER. 2025;9:13.
Published: 4/3/2025 | DOI: 10.22454/PRiMER.2025.685891
Introduction: Inbox management in outpatient primary care consumes a substantial amount of time, and residency training programs face unique challenges related to provider schedules. Long work hours, provider burnout, and worse patient outcomes can all be attributed to task management burden. Team-based care models can provide support through coverage systems and group inboxes. However, more empirical study of these systems may help to inform their implementation in interdisciplinary medical residency outpatient clinics.
Methods: The current study investigated the implementation of a “task buddy” system, which paired providers in teams to manage electronic health record (EHR) tasks. Data were collected on average task age and number of late tasks preimplementation, postimplementation, and 6 months postimplementation. Paired samples t tests were used to compare average task age for each task team. Participation was encouraged through a small monetary reward.
Results: A total of 23 resident physicians and 13 faculty from multiple disciplines participated. Our data demonstrated that the average age of tasks was more than 1 day lower with this system, but total late tasks did not improve.
Conclusions: The task buddy system resulted in quicker response time to complete tasks, but the number of late tasks stayed stagnant. Future studies should assess any correlation between improved patient outcomes with more efficient EHR task management. Additional studies across multiple residencies and specialties could better elucidate generalizability and provider perspectives of this pilot program.
Participants
Participants were 23 family medicine residents, 10 physician faculty, 1 pharmacy faculty, and 2 behavioral health faculty members.
Procedure
This project was granted an exemption from formal review by our institutional review board. We assigned resident task buddies based on their postgraduate year. We paired faculty based on their role to help each other with similar types of tasks, such as pairing a clinical social worker and psychologist. In the instance of an odd number, we made a group of three. We gave groups an anonymous label for data tracking. Participation was encouraged through offering a $5 reward to the group that had the quickest task completion each month.
We implemented the task buddy system in March 2022 and collected data through May 2022. The pilot was launched with an email announcement describing the teams and purpose of the project. The project was also briefly reviewed in a faculty meeting, in a resident didactic session, and in clinic huddles. Due to faculty position restructuring, we paused data collection from June to July and adjusted two of the buddy groups in July. When a new intern class arrived in July, we assigned that class into buddy pairs and collected data in August and September 2022.
The clinical informatics team provided data directly related to task completion in the EHR. Tasks in the EHR system include medication refills, requests for call backs, note management reminders, and communication messages. We calculated the average task age based on the number of days before the task was completed. The percentage of tasks deemed late (defined by our institution as 7 or more days before completion) was calculated by dividing the number of late tasks by the number of total tasks for the month.
The clinical informatics team provided task data per pair of task buddies across several months. To establish a baseline, we obtained data for 3 months before implementing the buddy system. We also obtained data for 3 months following the implementation of the task buddy system as well as 6 months after implementation.
Analytic Plan
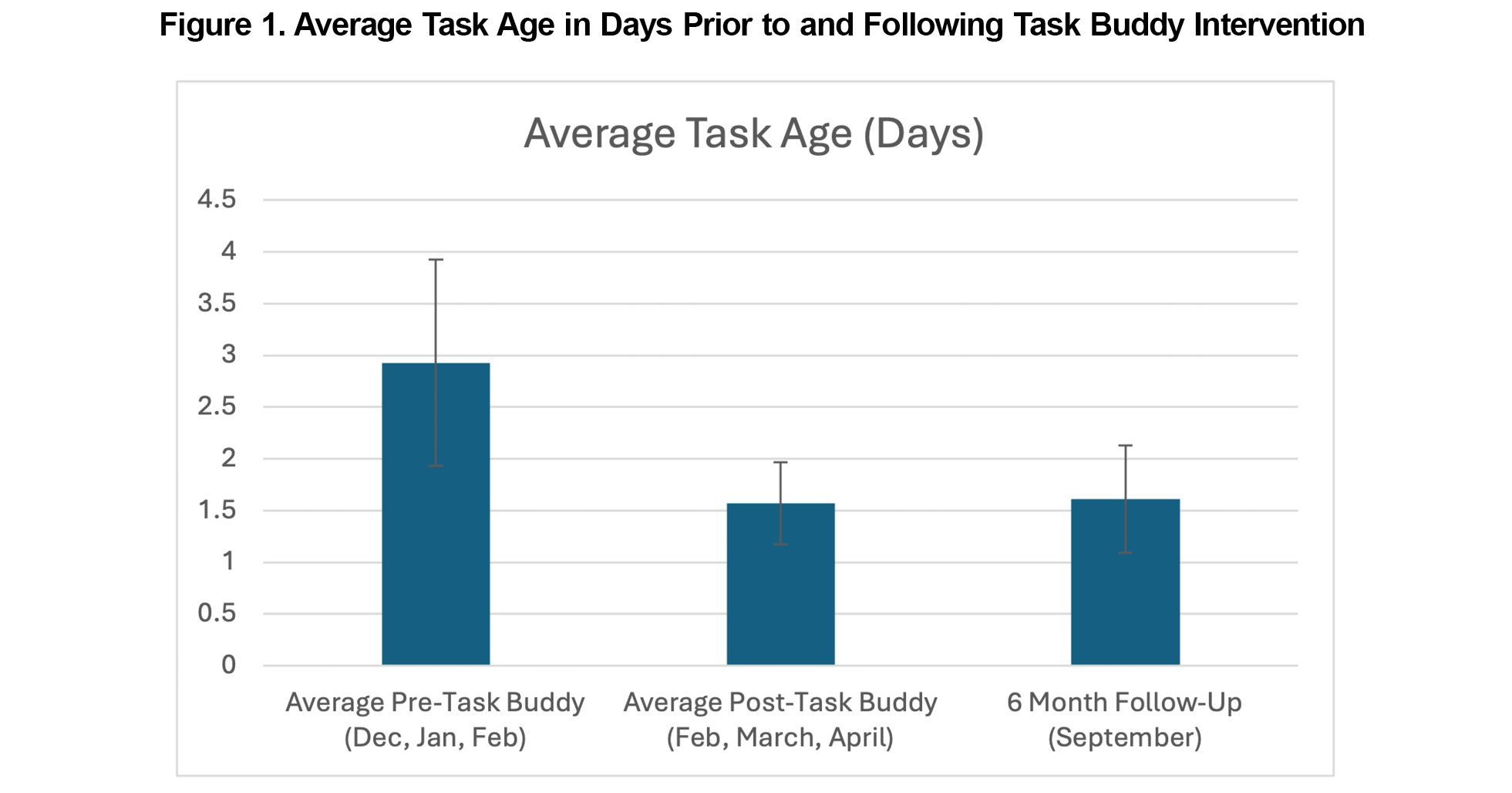
We used paired samples t tests to compare features of administrative tasks for each team of buddies. To account for potential variations, an average was obtained for each team 3 months preimplementation for use as a baseline and 3 months postimplementation. Additionally, we obtained data from 6 months postimplementation to test long-term follow-up. Due to one team representing a significant statistical outlier in average task age (greater than three standard deviations above the mean), that pair was removed from all analyses and results presented in Figure 1. The pattern of results is consistent between their inclusion and removal, and thus results are presented without the outlier for clarity.
Average Task Age
Paired samples t tests indicated that the average age of each team’s tasks was significantly lower (M=1.57 days, SD=0.79) after we implemented the task buddy system compared to before (M=2.93 days, SD=1.99; t=4.06 [95% CI: 0.65, 2.08], P<.01). The average age of tasks was also significantly lower at the 6 month follow-up (M=1.61, SD=1.04) compared to the average of the 3 months before (t=3.37 [95% CI: 0.45, 1.99], P<.01).
Late Tasks
The ratio of late-to-total tasks did not significantly differ before (M=18.1%, SD=10.5) or after (M=19.4%, SD=10.7) we implemented the task buddy system (t=-1.15 [95% CI: -0.04, 0.01], P=.27).
With the task buddy system implemented, tasks were completed more than 1 day quicker on average. However, the overall number of late tasks did not show statistical improvement. Possibly this system improved response times for more directly actionable tasks through the support of a partner. However, more time-intensive tasks that required a response from the original provider may not have been impacted, thus the number of late tasks did not change overall. Additionally, task time remained lower when assessed at a 6-month follow-up. Taken together, this study provides initial evidence from a small-scale implementation suggesting that a task partner system can positively impact efficiency in the academic residency primary care setting. Other studies affirm that high team efficiency can reduce burnout and time spent within the EHR.1,10 One limitation of this study included the possibility that incentive gift cards motivated quicker task completion. Other limitations of this study included small study size and some variance in task buddy groups before and after data collection due to personnel changes. While we performed surveys to obtain opinions on the task buddy system, low response rate limited interpretation. As such, we were not able to analyze provider acceptability ratings of the task buddy system. Expanding this study across multiple residencies and specialties could better elucidate provider acceptability of this task buddy pilot. Further research and replication of the system would be necessary to generalize results to additional practice settings. Future directions could assess correlation among patient outcomes, reduced burnout, and improved work-life balance with more efficient EHR inbox management.
References
- Porter J, Boyd C, Skandari MR, Laiteerapong N. Revisiting the time needed to provide adult primary care. J Gen Intern Med. 2023;38(1):147-155. doi:10.1007/s11606-022-07707-x
- Holmgren AJ, Lindeman B, Ford EW. Resident physician experience and duration of electronic health record use. Appl Clin Inform. 2021;12(4):721-728. doi:10.1055/s-0041-1732403
- Rao SK, Kimball AB, Lehrhoff SR, et al. The impact of administrative burden on academic physicians: results of a hospital-wide physician survey. Acad Med. 2017;92(2):237-243. doi:10.1097/ACM.0000000000001461
- Kutney-Lee A, Brooks Carthon M, et al. Electronic health record usability: associations with nurse and patient outcomes in hospitals. Med Care. 2021;59(7):625-631. doi:10.1097/MLR.0000000000001536
- Li CJ, Shah YB, Harness ED, Goldberg ZN, Nash DB. Physician burnout and medical errors: exploring the relationship, cost, and solutions. Am J Med Qual. 2023;38(4):196-202. doi:10.1097/JMQ.0000000000000131
- Tawfik DS, Scheid A, Profit J, et al. Evidence relating health care provider burnout and quality of care: a systematic review and meta-analysis. Ann Intern Med. 2019;171(8):555-567. doi:10.7326/M19-1152
- Gallegos-Macias A, Pino MD. A team-based approach to electronic in-basket optimization. Fam Pract Manag. 2022;29(6):10-13.
- Robinson KE, Kersey JA. Novel electronic health record (EHR) education intervention in large healthcare organization improves quality, efficiency, time, and impact on burnout. Medicine (Baltimore). 2018;97(38):e12319. doi:10.1097/MD.0000000000012319
- Lieu TA, Altschuler A, Weiner JZ, et al. Primary care physicians’ experiences with and strategies for managing electronic messages. JAMA Netw Open. 2019;2(12):e1918287. doi:10.1001/jamanetworkopen.2019.18287
- Rotenstein LS, Hendrix N, Phillips RL, Adler-Milstein J. Team and electronic health record features and burnout among family physicians. JAMA Netw Open. 2024;7(11):e2442687. doi:10.1001/jamanetworkopen.2024.42687
Lead Author
Kathryn Hawks, DO
Affiliations: Family Medicine Residency, East Tennessee State University, Bristol, TN
Co-Authors
Brandi Dahl, PharmD - Family Medicine Residency, East Tennessee State University, Bristol, TN
Alexander Melkonian, PhD - Family Medicine Residency, East Tennessee State University, Bristol, TN
Laura Helmly, DO - Family Medicine Residency, Mary Washington Healthcare, Fredericksburg, VA
Corresponding Author
Brandi Dahl, PharmD
Correspondence: Family Medicine Residency, East Tennessee State University, Bristol, TN
Email: dahlbk@etsu.edu
Fetching other articles... 
Loading the comment form... 
Submitting your comment... 


There are no comments for this article.