Introduction: Infant male circumcision is a common elective procedure in the United States. Complications include bleeding, glans injury, insufficient or excessive skin removal, and adhesions. We assessed percentages and factors associated with complications of circumcisions at our community-based hospital from 2010 to 2020.
Methods: We conducted a retrospective cohort study of male infant patients who had circumcisions performed in the Kaiser Permanente Woodland Hills (KPWH) Medical Center from January 1, 2010, to January 1, 2020. Complications were measured through emergency room visits up to 24 hours postcircumcision, complication codes, and referral appointments to urology within 2 years of age.
Results: Of the total patients (N=2,715), 1.4% were referred to urology for potential complications, and 0.3% required revision surgery. Weight and age at the time of the circumcision and the location of the circumcision (hospital vs clinic) did not have a significant effect on the complication rate. Infants who had a circumcision with a Mogen clamp had an increased percentage of complications compared to the Gomco clamp (2% compared to 0.9%). The number of complications requiring surgery decreased (from 0.4% to 0.17%) when our hospital limited those physicians performing circumcisions by requiring 20 circumcisions per year to maintain privileges.
Conclusions: Infant male circumcision is a safe procedure whether performed in the hospital or clinic. Complications likely can be reduced if circumcisions are completed by physicians who perform them regularly. Further studies are needed to investigate the difference between Mogen and Gomco clamp outcomes.
Circumcision, a procedure involving removal of foreskin from the glans penis, is a common elective procedure performed on male infants in the United States. Studies indicate that risk of complications is minimized if the procedure is completed in infancy.1-8
The three most common and effective techniques for circumcision use the Mogen clamp, the Gomco clamp, and the Plastibell device. The Mogen and Gomco clamps protect the glans as the foreskin is excised, while the Plastibell device induces necrosis, resulting in sloughing of the foreskin within a week. In the United States, the Mogen and Gomco clamp are used more often than the Plastibell device. These techniques are equally effective, and letting the choice of device be guided by operator experience and comfort level is recommended.9-13
In the United States, procedure-related circumcision complication rates, both those requiring surgical revision and those that do not, in infants are low, ranging from 0.2% to 0.6%. Acute complications include bleeding (0.08% to 0.18%), injury to the penis (0.04%), and infection (0.06%). Late complications are rare and include adhesions, meatal stenosis, phimosis, and scarring.2,4,9,11,14-16
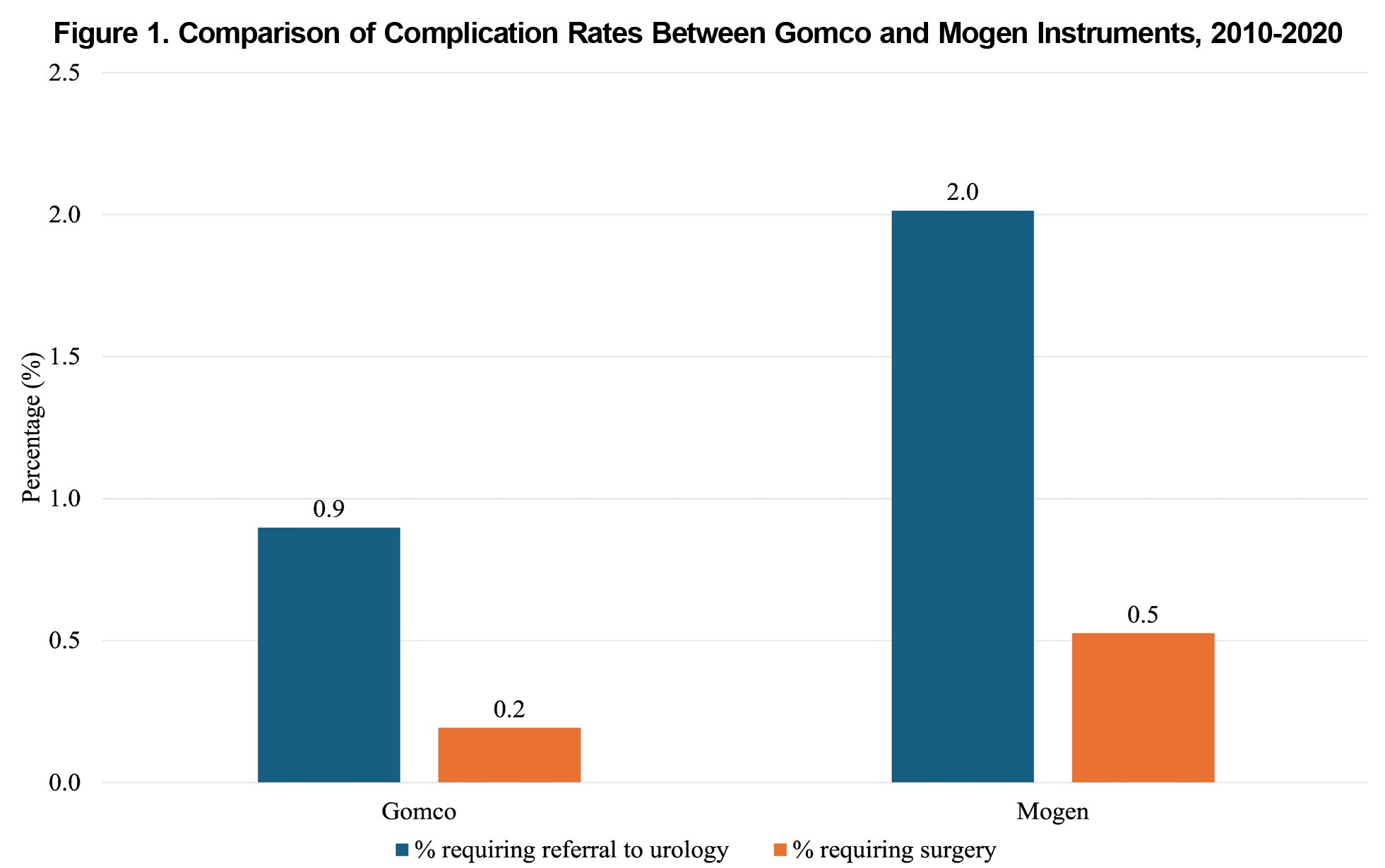
This study analyzes the factors influencing circumcision complications in male infants at our community-based hospital. In our hospital, the Family Medicine Department completed most circumcisions until 2017 and all circumcisions after 2017.
Circumcision complication rates have been studied in various settings; our study is unique in its setting of a family medicine residency department at a community-based hospital. During a time when the scope of family medicine procedures is threatened, data identifying factors that may reduce the risk of complications after circumcision may help support family medicine privileges at certain institutions.
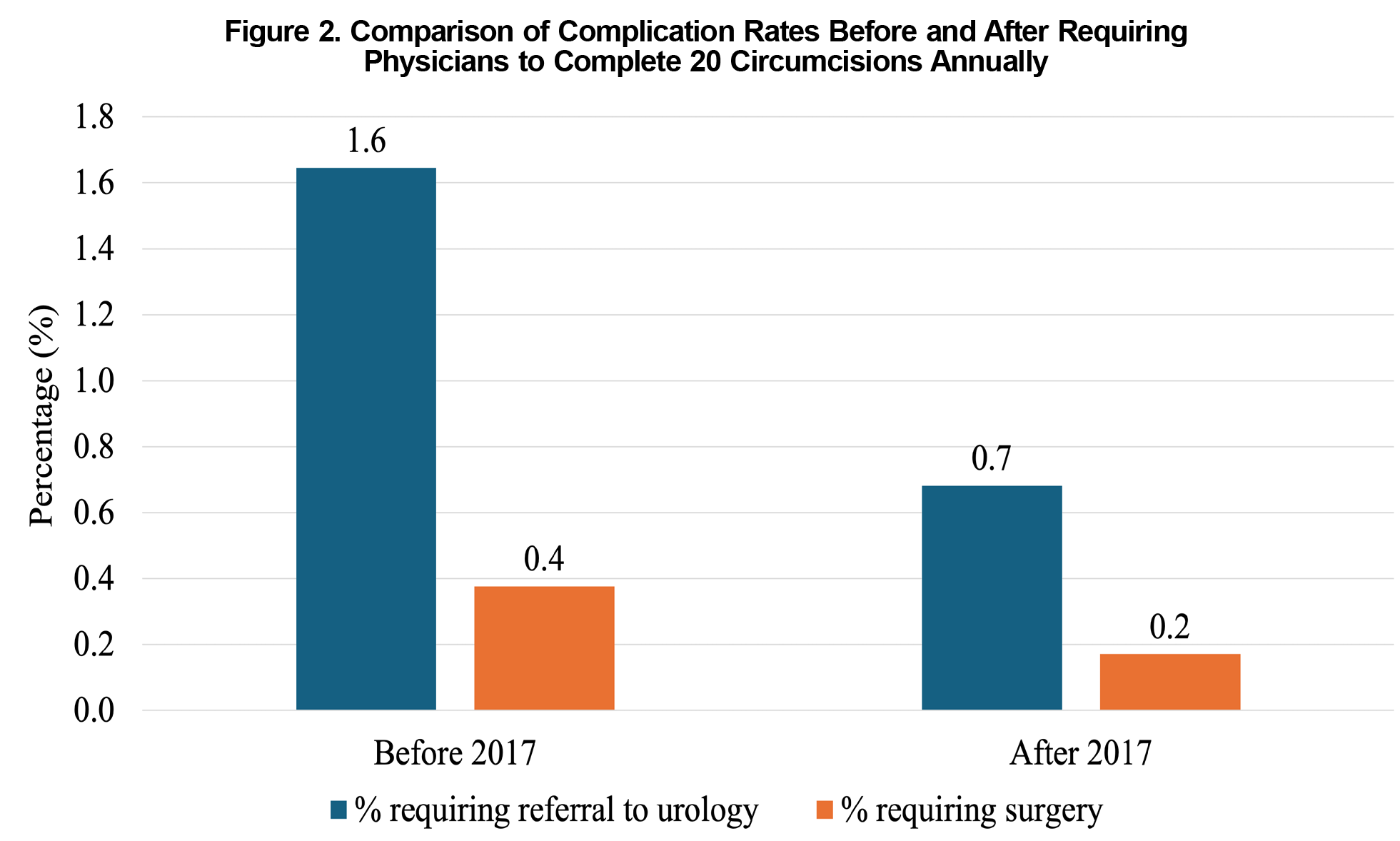
For this retrospective cohort study, we used the electronic medical data of Kaiser Permanente Woodland Hills (KPWH) male pediatric patients who had circumcisions performed by the Family Medicine Department in the KPWH Medical Center from January 1, 2010, to January 1, 2020. A total of 4,372 participants met this criterion. From this group, we excluded patients who did not retain Kaiser Permanente health insurance within 60 days after the birth, who lost their membership before the 2-year follow-up ended, or whose circumcision was not performed by an obstetrics and gynecology physician before 2017 or a family medicine doctor. Consequently, 1,657 patients were excluded, and analysis was completed on the remaining 2,715.
The primary outcome we analyzed were the complications documented during follow-up visits within 2 years of circumcision. Complications were measured by looking at complication codes, emergency room visits within 24 hours of the circumcision to assess bleeding complications, and appointments in urology within 2 years of age to assess for late complications such as adhesions and inadequate circumcisions.
We performed Wilcoxon rank sum tests to assess for differences in age and weight between the two groups—male infant patients who had complications and those who did not. Additionally, we performed χ2 tests to assess the distribution of characteristics (location, presence of hypospadias, prematurity, and clamp type) between the two groups.
This research was reviewed and approved by the Kaiser Permanente Southern California Institutional Review Board.
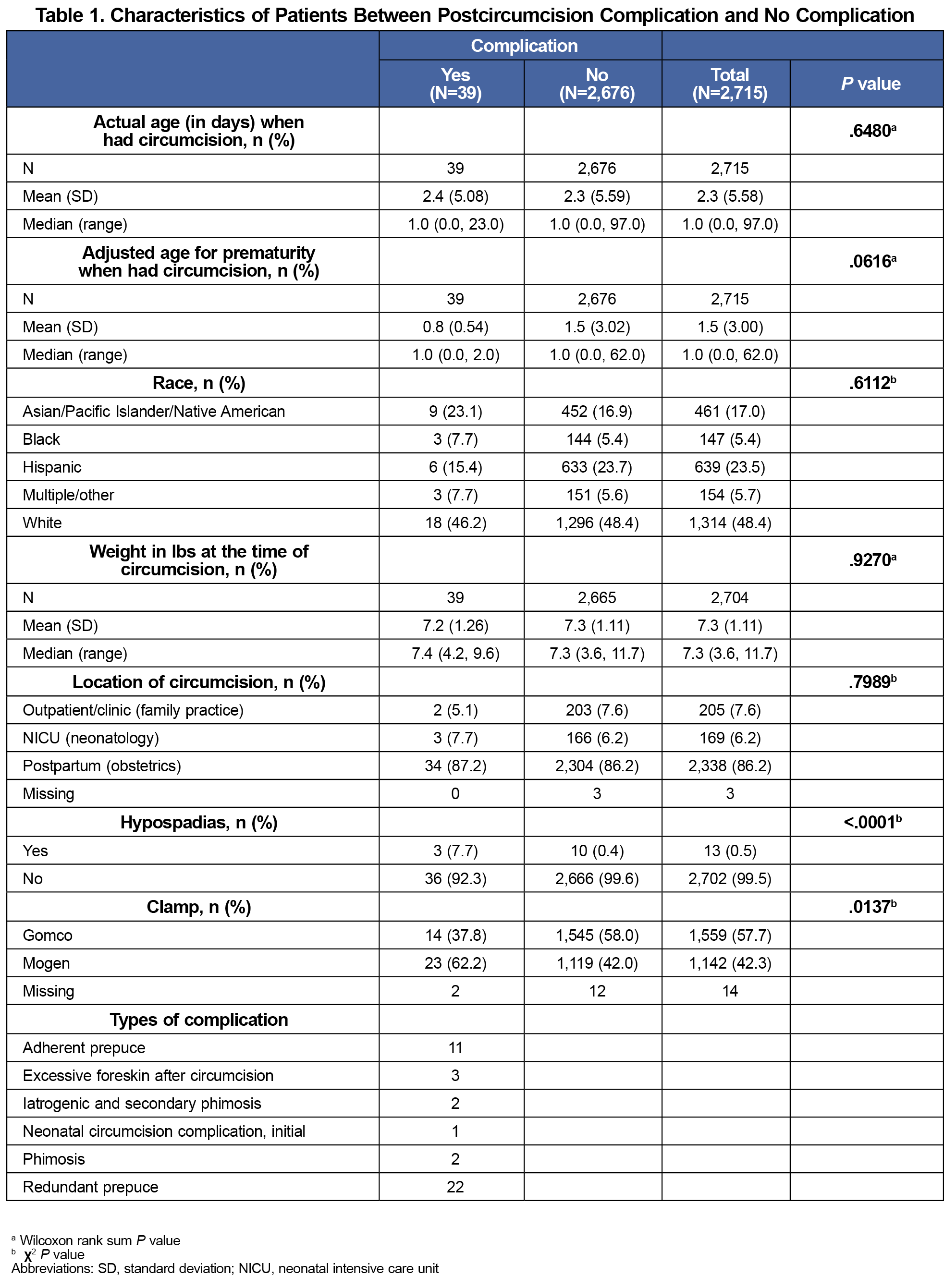
A total of 2,715 male infants met our inclusion criterion for analysis (Table 1). Of this total, most circumcisions were performed with the Gomco clamp (1,559/2,715, 57.7%), and the rest used the Mogen clamp.
No emergency room visits were documented for circumcision-related complications. Review of complication codes indicated no bleeding complications in circumcised patients.
Overall, 1.4% (39/2,715) of infants had complications after completion of the procedure, as measured by referrals to urology for further evaluation. Types of complications included adherent prepuce, excessive foreskin after circumcision, iatrogenic and secondary phimosis, phimosis, and redundant foreskin.
Babies who had a circumcision with a Mogen clamp had an increased rate of complications compared to the Gomco clamp (23/1,142 [2.0%] compared to 14/1,559 [0.9%], P=.0137; Figure 1). When our hospital limited those physicians performing circumcisions by requiring 20 circumcisions per year to maintain privileges, the prevalence of complications decreased (from 1.6% to 0.7%). After this change, the number of complications requiring surgery decreased (from 8/2,128 [0.4%] to 1/587 [0.17%]) as well (Figure 2). Additionally, infants with hypospadias had an increased rate of circumcision complications compared to those infants without (3/13 [23.1%] compared to 36/2,702 [1.3%], P<.0001).
Weight or age at the time of the circumcision, the infant’s race, and the location of the circumcision (hospital vs clinic) did not have a significant effect on the complication rate.
After urology consultation, some infants required no further intervention, some were treated with topical steroids, and 9 of 2,715 (0.3%) underwent revision surgery.
Male circumcision, when performed in infancy by physicians, is a safe procedure.8 In the United States, the prevalence of complications of circumcision in newborns requiring surgical revision is 0.4%, and our study found that at our community-based hospital, prevalence of circumcision complications requiring surgical revision was 0.3%.14 All complications at KPWH involved redundant skin, phimosis, or adhesion. No acute complications involving excessive bleeding or trauma to the glans were noted.
Though studies indicate similar complication rates after use of the Mogen or Gomco clamp, our data showed an increased chance of complications after use of the Mogen clamp. Further studies need to be completed to investigate the difference between Mogen and Gomco clamp outcomes.
Our results indicated that circumcisions can be safely performed by family physicians and that circumcision training should be offered as part of residency training. In the United States, parents who want their child circumcised in the first month of life can face barriers, including issues in access such as hospitals that do not offer the procedure or lack of available providers who have experience with the procedure.17-19 As such, training that includes observation and use of different methods as well as training both inpatient and outpatient can help build capacity in this procedure and minimize barriers to access.20
Our data had several strengths, notably reliable follow-up visits within the Kaiser Permanente health care system that allows for effective tracking of complications over years. Among our limitations was that our center does not use the Plastibell device. Future research could incorporate training data from institutions where the Plastibell device is used in addition to the Mogen and Gomco clamps.
Acknowledgments
Presentations: Complications Associated With Infant Male Circumcision in a Community-Based Hospital, 40th Annual University of Los Angeles Family Medicine Research Day Forum, Los Angeles, California, June 2024.
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Blank S, Brady M, Buerk E, et al; American Academy of Pediatrics Task Force on Circumcision. Circumcision policy statement. Pediatrics. 2012;130(3):585-586. doi:10.1542/peds.2012-1989
- Shabanzadeh DM, Clausen S, Maigaard K, Fode M. Male circumcision complications—a systematic review, meta-analysis and meta-regression. Urology. 2021;152:25-34. doi:10.1016/j.urology.2021.01.041
- Zeitler M, Rayala B. Neonatal circumcision. Prim Care. 2021;48(4):597-611. doi:10.1016/j.pop.2021.08.002
- Hutcheson JC. Male neonatal circumcision: indications, controversies and complications. Urol Clin North Am. 2004;31(3):461-467. doi:10.1016/j.ucl.2004.04.011
- Tiryaki S, Issi Y. The association of meatal stenosis and infant circumcision. Turk J Pediatr. 2023;65(4):661-666. doi:10.24953/turkjped.2023.46
- Morris BJ, Wamai RG, Henebeng EB, et al. Estimation of country-specific and global prevalence of male circumcision. Popul Health Metr. 2016;14(1):4. doi:10.1186/s12963-016-0073-5
- American College of Obstetricians and Gynecologists, Committee on Obstetric Practice. ACOG Committee opinion. circumcision. number 260, October 2001. Obstet Gynecol. 2001;98(4):707-708.
- Morris BJ, Waskett JH, Banerjee J, et al. A ‘snip’ in time: what is the best age to circumcise? BMC Pediatr. 2012;12(1):20. doi:10.1186/1471-2431-12-20
- Krill AJ, Palmer LS, Palmer JS. Complications of circumcision. Sci World J. 2011;11:2,458-2,468. doi:10.1100/2011/373829
- Earp BD, Mishori R, Rotta AT. Newborn circumcision techniques and medical ethics. Am Fam Physician. 2021;103(2):69-70.
- Omole F, Smith W, Carter-Wicker K. Newborn circumcision techniques. Am Fam Physician. 2020;101(11):680-685.
- Prabhakaran S, Ljuhar D, Coleman R, Nataraja RM. Circumcision in the paediatric patient: a review of indications, technique and complications. J Paediatr Child Health. 2018;54(12):1,299-1,307. doi:10.1111/jpc.14206
- Abdulwahab-Ahmed A, Mungadi IA. Techniques of male circumcision. J Surg Tech Case Rep. 2013;5(1):1-7. doi:10.4103/2006-8808.118588
- El Bcheraoui C, Zhang X, Cooper CS, Rose CE, Kilmarx PH, Chen RT. Rates of adverse events associated with male circumcision in U.S. medical settings, 2001 to 2010. JAMA Pediatr. 2014;168(7):625-634. doi:10.1001/jamapediatrics.2013.5414
- Weiss HA, Larke N, Halperin D, Schenker I. Complications of circumcision in male neonates, infants and children: a systematic review. BMC Urol. 2010;10(1):2. doi:10.1186/1471-2490-10-2
- Heras A, Vallejo V, Pineda MI, Jacobs AJ, Cohen L. Immediate complications of elective newborn circumcision. Hosp Pediatr. 2018;8(10):615-619. doi:10.1542/hpeds.2018-0005
- Corona LE, Rosoklija I, Walton RF, et al. COVID-19 pandemic adversely affects the provision of desired newborn circumcision: perinatal physician perspectives. Front Health Serv. 2022;1:799647. doi:10.3389/frhs.2021.799647
- Otto R, Evans G, Boniquit C, Peppas D, Leslie J. Why desired newborn circumcisions are not performed: a survey. Urology. 2016;97:188-193. doi:10.1016/j.urology.2016.06.054
- Johnson EK, Rosoklija I, Walton RF, Matoka DJ, Seager CM, Holl JL. Physician perspectives on performing newborn circumcisions: barriers and opportunities. Matern Child Health J. 2024;28(1):144-154. doi:10.1007/s10995-023-03822-1
- Rosen J, Rosoklija I, Walton RF, et al. Recommendations to improve neonatal circumcision training. Hosp Pediatr. 2024;14(6):e249-e253. doi:10.1542/hpeds.2023-007696



There are no comments for this article.