Introduction: Accurate blood pressure (BP) measurement is essential for hypertension diagnosis and management. While automated office blood pressure (AOBP) readings are increasingly used in many primary care settings, the challenges of implementing automated readings have not been fully explored in lower-resource settings. Our study compared patient processing times using standard care versus AOBP when indicated.
Methods: We collected data on the processing times of patients at an urban community health center for 1 month using standard care, including data on a second BP taken when the initial BP was >140/90 mmHg. The following month, we piloted a protocol wherein an initial BP of >140/90 would be followed by AOBP. We then compared average patient processing times between the two groups.
Results: Of the 157 adult BP measurements taken during the study, 20% (32/157) had an initial BP >140/90. During the month of standard care, the mean processing time was 8.25 minutes (SD=3.6), which was not significantly different during the month of AOBP use, 8.38 minutes (SD=3.6; P=.84). Most patients in the AOBP group had an AOBP measurement of <140/90 (60%, n=27). Most (80%, n=12) of the patients whose AOBP remained >140/90 had their treatment plan discussed and revised.
Conclusions: The literature has established that AOBP may reduce clinical inertia by increasing confidence in BP accuracy. We conclude that AOBP protocol can be incorporated into clinic workflow without significantly impacting overall processing time.
Background
Blood pressure (BP) is an important, modifiable risk factor for cardiovascular disease, and accurate BP measurement is essential to diagnosing and managing hypertension.1 Automated office blood pressure (AOBP) refers to a protocol in which a fully automated blood pressure cuff records three sequential readings while the patient sits quietly. The machine then averages these values to provide a more accurate BP value—unlike the standard BP measurement, which typically uses one manual or automated reading by clinic staff.2 Averaged AOBP measurements are reliable, often lower than standard office measurements, and valid across multiple clinical settings.2-8
AOBP offers several advantages over traditional BP measurement methods, including reduced human interaction during readings, which minimizes the white coat effect and yields more reproducible BP values.2 These advantages help avoid overtreatment and are especially relevant in primary care settings, where efficiency and precision are critical.
AOBP measurement correlates well with the gold standard of 24-hour ambulatory BP monitoring and has been used in standard-setting studies such as the Systolic Blood Pressure Intervention Trial.2-4, 9-12 While the popularity of AOBP is rising in primary care settings, implementation challenges have not been fully explored in high-volume, lower-resourced settings.13,14
Objectives
This study compares the processing times for patients at an urban federally qualified health center (FQHC) using standard care versus AOBP protocol. AOBP has been validated in multiple settings as more accurate than the standard protocol.15 Few studies have examined its feasibility in high-volume, low-resource environments such as FQHCs. Such clinics face staffing shortages and workflow constraints that make adopting new protocols challenging. This study aimed to evaluate the practical impact of implementing AOBP on clinic processing times in an FQHC, addressing a gap in the operational feasibility literature.
Setting and Design
The patient population included a sample of 157 adults during appointments at the FQHC. Patients younger than 18 years of age were excluded. Month 1 and Month 2 refer to specific data collection periods: the standard care period (Month 1) was measured over 5 clinic days, while the AOBP protocol was implemented over 9 clinic days (Month 2). Days were selected based on the primary author’s availability to observe clinic operations and collect data. The sample represents all eligible adult patients processed by the certified medical assistant (CMA) during these selected days. All were routine days with no known changes in staffing, scheduling, or procedures.
Participants and Variables
During Month 1, the CMA followed standard procedure, checking one additional BP reading for any systolic BP (SBP) >140 mmHg or diastolic BP (DBP) > 90 mmHg. This procedure followed the 2022 American Academy of Family Physicians guidelines, defining hypertension as BP ≥140/90 mmHg.16 At the beginning of patient visits, all vital signs were collected using a Welch Allyn Conax 7300 sphygmomanometer.
For Month 2, the sphygmomanometer was programmed to perform the AOBP protocol, and the CMA was trained on how to use it. This protocol, implemented by pressing a symbol on the machine, begins with a 30-second waiting period, followed by a BP measurement, a 60-second pause, a second measurement, another 60-second pause, and then a third BP reading. The meter then displays the average of these three readings. Specific details of the protocol can be found in Appendix A.
During Month 2, the AOBP protocol was implemented instead of an additional standard reading when the first BP reading was SBP >140 or DBP >90. Due to clinic workflow and space limitations, the CMA remained in the room during the AOBP protocol. In three cases, the physician implemented AOBP when the CMA was unavailable.
Data Collection
The lead author recorded processing times each month. Processing times were measured using a standardized data collection sheet. Time was recorded by the primary author via a stopwatch at three points: when the patient checked in, when the CMA and patient entered the processing room, and when the patient left the processing room to see the physician. The primary measure of processing time was calculated as the duration between the patient entering the processing room and leaving it to see the physician.
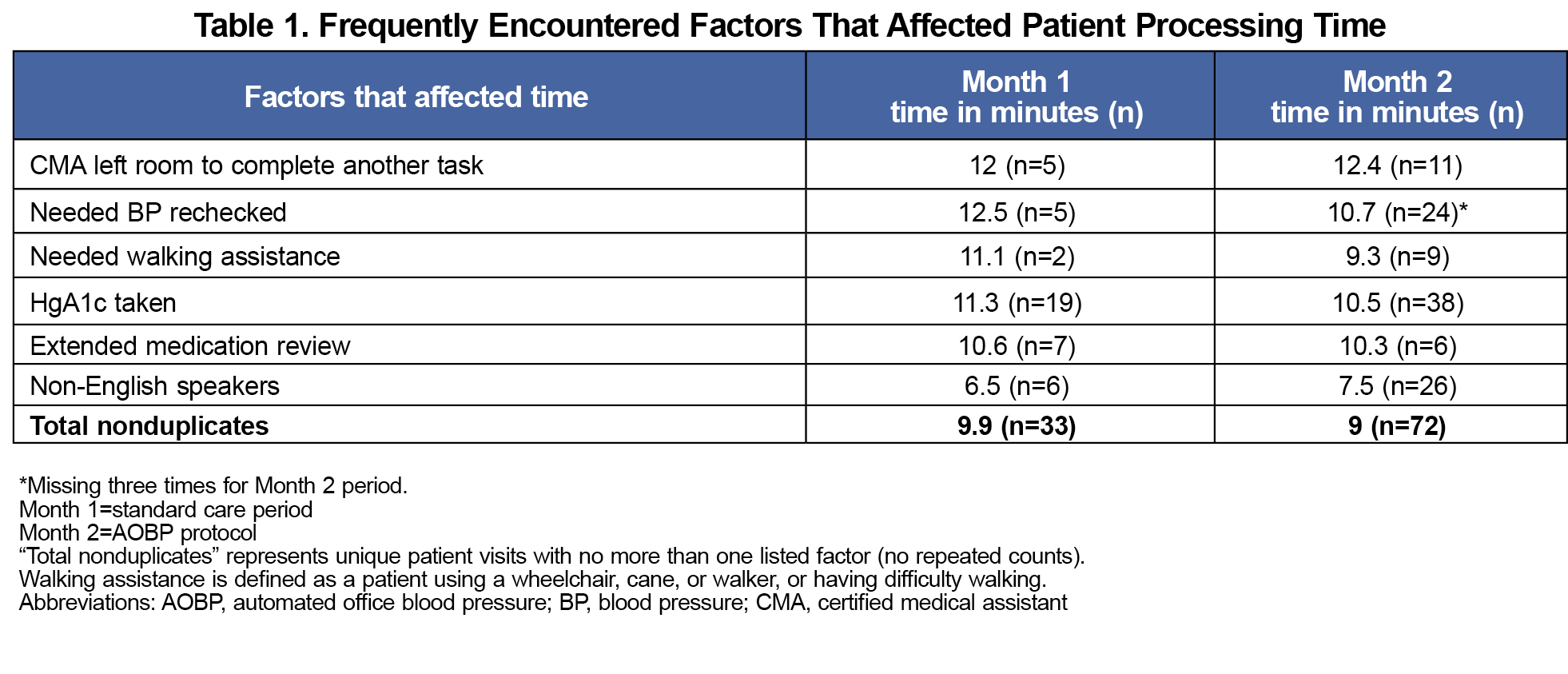
While in the processing room, the primary author also recorded potential workflow-related factors that could influence processing time. These observations were documented in real time during clinic operations, using the same standardized data collection sheet as the processing times. These observations included whether the CMA left the room to complete another task, the patient required a blood pressure recheck, needed walking assistance, had an HgA1c drawn, required an extended medication review, or was a non-English speaker. These variables were tracked for each visit and are summarized in Table 1.
Statistical Methods
All descriptive data were entered into a secure, cloud-based collaboration platform and analyzed using Microsoft Excel. We used descriptive statistics to calculate means, standard deviations, and ranges for patient processing times. We used a two-sample t test assuming equal variances to compare mean processing times between the Month 1 (standard care) and Month 2 (AOBP) groups. A P value of less than .05 was considered statistically significant. The Research Advisory Group of the FQHC reviewed and approved this project before implementation. The project received retrospective Institutional Review Board approval by Sterling IRB, ID number: 11699-RAyyagir.
Participants
We collected data on 157 adult patients: 55 during Month 1 with standard care and 102 during Month 2 using AOBP. Only 9% (5 of 55) of patients had an initial BP of >140/90 in Month 1, and 26% (27/102) needed a BP recheck during Month 2 (the AOBP pilot).
Primary Outcomes
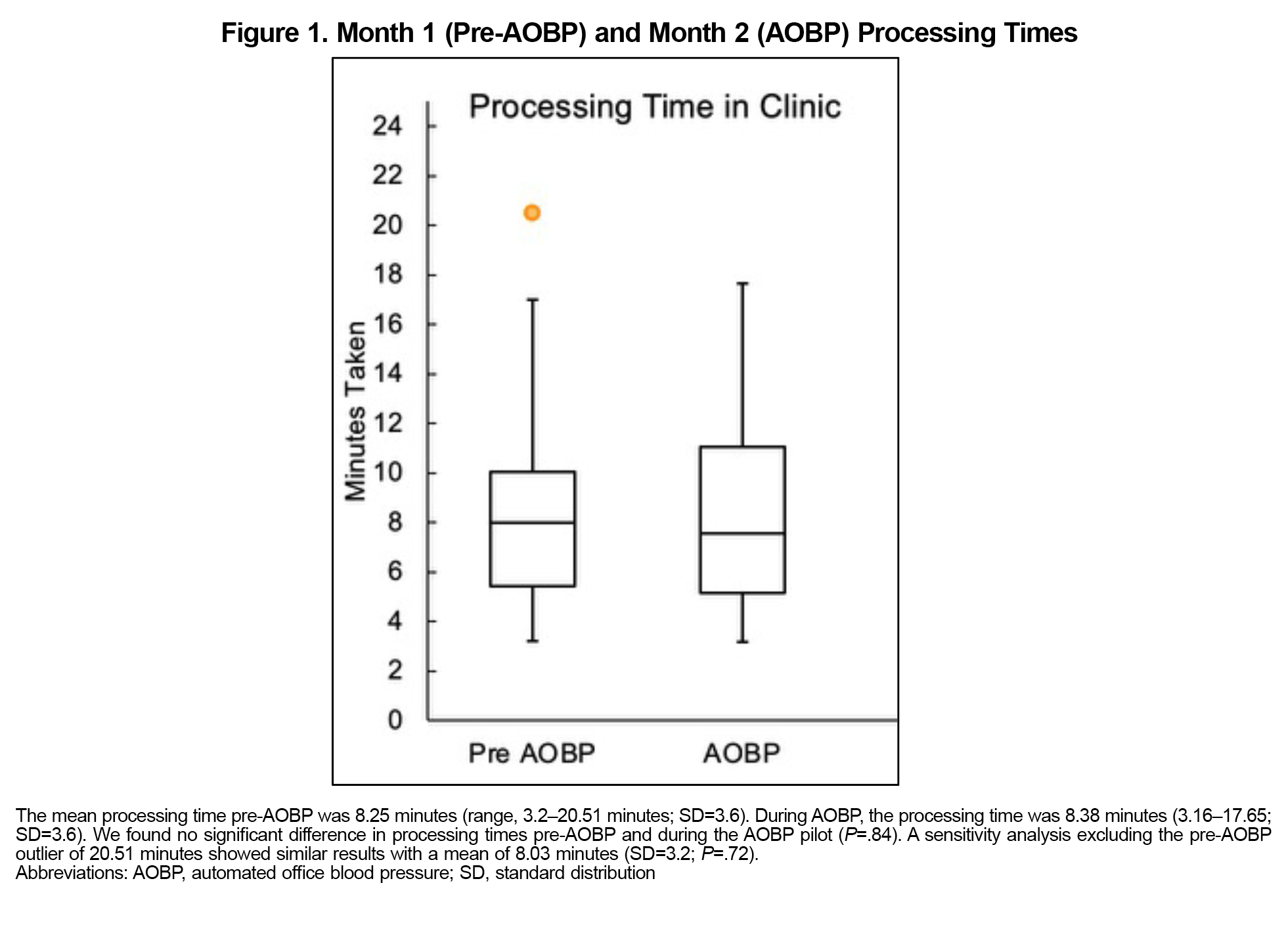
Clinic processing times before and after AOBP implementation were not significantly different at 8.25 minutes (SD=3.6 minutes) and 8.38 minutes (SD 3.6; P=.84; Figure 1). During the study, 20% (32 out of 157) of patients required a BP recheck. One outlier in the Month 1 group had a processing time of 20.51 minutes due to a patient reentering the room for an additional HgA1c test after an initial elevated result. A sensitivity analysis excluding this outlier yielded a similar mean processing time of 8.03 minutes (SD=3.2), and the difference between groups remained nonsignificant (P=.72).
The average AOBP dropped below 140/90 for 40% (10/25) of patients with an initial high BP (mean SBP –8.7 mmHg and diastolic BP –3.8 mmHg). Of the 60% (15/25) of patients whose averaged AOBP remained >140/90, most (80%, 12/15) received a medication adjustment. Reasons for no medication adjustment included patients not yet taking medication that day or declining. The study team forgot to enter the averaged AOBP into the electronic health record for two patients.
Secondary Outcomes
Table 1 provides further detail on workflow-related factors that contributed to variations in processing times. Visits involving a BP recheck, HgA1c testing, or exit of the CMA from the room were associated with the longest average processing times across both groups. Specifically, when the CMA left the room to complete another task, mean processing time rose to more than 12 minutes. Conversely, encounters with non-English-speaking patients had among the shortest average times.
The percentage of patients with an initial BP >140/90 mmHg was 20%. Month 1 (standard care) and Month 2 (AOBP) processing times were comparable (Figure 1), suggesting that AOBP did not increase patient processing time and is feasible in this setting (P=.84). After presenting the data to clinic staff and leadership, the AOBP protocol was adopted into clinic procedures.
This study helped reeducate staff on proper BP measurement and educated them about AOBP accuracy. Optimizing workflow requires considering the layout of clinic rooms, the number of available rooms and vitals machines, and the overall flow of each clinic session. The prevalence of common factors that increase processing time was similar during Months 1 and 2, suggesting these did not confound results (Table 1).
Limitations
Timing the processing of a visit is potentially subject to human error. In three instances, the physician (rather than the CMA) performed the AOBP in the exam room, and this time was not easily tracked. This study also was limited by a small sample size. Additionally, data were collected over only 5 days for standard care and 9 days for AOBP. The data collection days were limited to those when the primary author was available, which may have introduced sampling bias or affected the representativeness and generalizability of the sample. Additionally, while AOBP was conducted with staff present in the room due to clinic constraints, previous research has shown that staff presence during AOBP measurements does not significantly impact the results, with comparable readings found in both attended and unattended settings.4
This study extends prior work by evaluating feasibility through the lens of operational efficiency, a crucial factor for widespread adoption in FQHCs serving vulnerable populations with many medical and social needs. Although conducted in a single FQHC, the clinic’s constraints reflect those in many resource-limited clinical settings. The findings may inform future implementation efforts in similar primary care settings. The consistency in processing times across measurement types suggests the feasibility of broad AOBP integration, provided that clinics accommodate necessary training and workflow adjustments.
Acknowledgments
The authors acknowledge the efforts and contributions of their ACPM faculty and staff advisors: Ayanna Buckner, MD, MPH, FACPM, Principal of Community Health Cooperative; Anita Balan, MPH, CHES, Project Director; and Kate Shreve, MPH, Director of Programs and Grants.
They also acknowledge the support and advice of the Branch Chief of the Program Development and Services Branch in the Division for Heart Disease and Stroke Prevention at the Centers for Disease Control and Prevention: Letitia Presley-Cantrell, PhD, as well as Kaha Ahmed, MPH, CPH, of the same branch. They appreciate the work and dedication of leadership and staff at Lincoln Community Health Center.
Author Contributions
Conceptualization, H.B and M.G.; methodology, M.G., P.C.B., K.I., S.G., T.W., and H.B.; formal analysis, M.G.; writing—original draft preparation, M.G., H.B. P.C.B.; writing—review and editing, M.G., P.C.B., H.B.; visualization, M.G., H.B., P.C.B; supervision, H.B., T.W., K.I., S.G.; data curation, M.G.; investigation, M.G., H.B.; project administration, H.B.; resources, H.B., K.I. All authors read and agreed to the published version of the manuscript.
Funding
This project is partially supported by the American College of Preventive Medicine through a cooperative agreement (CDC-RFA-OT18-1802) with the Centers for Disease Control and Prevention (CDC) of the US Department of Health and Human Services (HHS). The content is solely the responsibility of the authors and does not necessarily represent the official views of, nor an endorsement by, the CDC/HHS or the US Government.
Presentations
Incorporating Automated Office Blood Pressure Into Federally Qualified Health Center Patient Processing. Poster presentation at Annasaheb Chudman Patil Memorial (ACPM) College & Hospital, April 2024, Washington DC.
References
- Kallioinen N, Hill A, Horswill MS, Ward HE, Watson MO. Sources of inaccuracy in the measurement of adult patients’ resting blood pressure in clinical settings: a systematic review. J Hypertens. 2017;35(3):421-441. doi:10.1097/HJH.0000000000001197
- Roerecke M, Kaczorowski J, Myers MG. Comparing automated office blood pressure readings with other methods of blood pressure measurement for identifying patients with possible hypertension: a systematic review and meta-analysis. JAMA Intern Med. 2019;179(3):351-362. doi:10.1001/jamainternmed.2018.6551
- Muntner P, Shimbo D, Carey RM, et al. Measurement of blood pressure in humans: a scientific statement from the American Heart Association. Hypertension. 2019;73(5):e35-e66. doi:10.1161/HYP.0000000000000087
- Jones DW. Implementing automated office blood pressure measurement. Hypertension. 2019;74(3):436-440. doi:10.1161/HYPERTENSIONAHA.118.10966
- Myers MG, Kaczorowski J, Dolovich L, Tu K, Paterson JM. Cardiovascular risk in hypertension in relation to achieved blood pressure using automated office blood pressure measurement. Hypertension. 2016;68(4):866-872. doi:10.1161/HYPERTENSIONAHA.116.07721
- Agarwal R. Implications of blood pressure measurement technique for implementation of systolic blood pressure intervention trial (SPRINT). J Am Heart Assoc. 2017;6(2):e004536. doi:10.1161/JAHA.116.004536
- Chambers LW, Kaczorowski J, O’Rielly S, Ignagni S, Hearps SJ. Comparison of blood pressure measurements using an automated blood pressure device in community pharmacies and family physicians’ offices: a randomized controlled trial. CMAJ Open. 2013;1(1):E37-E42. doi:10.9778/cmajo.20130005
- Andreadis EA, Papademetriou V, Geladari CV, Kolyvas GN, Angelopoulos ET, Aronis KN. Home, automated office, and conventional office blood pressure as predictors of cardiovascular risk. J Am Soc Hypertens. 2017;11(3):165-170.e2. doi:10.1016/j.jash.2017.01.009
- Doane J, Flynn M, Archibald M, Ramirez D, Conroy MB, Stults B. Unattended automated office blood pressure measurement: time efficiency and barriers to implementation/utilization. J Clin Hypertens (Greenwich). 2020;22(4):598-604. doi:10.1111/jch.13840
- Cushman WC, Evans GW, Byington RP, et al; ACCORD Study Group. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362(17):1,575-1,585. doi:10.1056/NEJMoa1001286
- Wright JT Jr, Williamson JD, Whelton PK, et al; SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2,103-2,116. doi:10.1056/NEJMoa1511939
- Myers MG, Kaczorowski J, Paterson JM, Dolovich L, Tu K. Thresholds for diagnosing hypertension based on automated office blood pressure measurements and cardiovascular risk. Hypertension. 2015;66(3):489-495. doi:10.1161/HYPERTENSIONAHA.115.05782
- Andreadis EA, Geladari CV, Angelopoulos ET, Kolyvas GN, Papademetriou V. Morning surge and peak morning ambulatory blood pressure versus automated office blood pressure in predicting cardiovascular disease. High Blood Press Cardiovasc Prev. 2019;26(3):209-215. doi:10.1007/s40292-019-00315-7
- Doane J, Buu J, Penrod MJ, Bischoff M, Conroy MB, Stults B. Measuring and managing blood pressure in a primary care setting: a pragmatic implementation study. J Am Board Fam Med. 2018;31(3):375-388. doi:10.3122/jabfm.2018.03.170450
- Johnston KJ, Wen H, Joynt Maddox KE. Lack of access to specialists associated with mortality and preventable hospitalizations of rural Medicare beneficiaries. Health Aff (Millwood). 2019;38(12):1,993-2,002. doi:10.1377/hlthaff.2019.00838
- American Academy of Family Physicians. Clinical practice guideline: hypertension. July 2022.https://www.aafp.org/family-physician/patient-care/clinical-recommendations/all-clinical-recommendations/highbloodpressure.html



There are no comments for this article.