Introduction: A person’s sex and/or gender may influence the pathogenesis, presentation, and therapeutic response to disease; yet, the impact of sex and gender is not routinely evaluated in medical research, nor adequately emphasized in medical school curricula. Little is known about medical school faculty knowledge and attitudes regarding sex and gender-based medicine (SGBM).
Methods: We administered an online survey to 158 faculty members at WMU Homer Stryker M.D. School of Medicine. The survey of knowledge on SGBM was adapted from two prior surveys used in medical student and resident populations and modified for faculty participants. Hidden curriculum theory, which proposes students learn through formal curriculum as well as through passive perceptions of faculty and institutional attitudes, was used as a theoretical lens.
Results: Thirty-eight of 158 recipients completed the survey, for a 24% response rate. Respondents answered an average of 48.53% of the knowledge questions correctly; percent correct did not differ significantly between men and women faculty members (P= .2732). Seventy one percent of respondents indicated it was important or very important to consider sex and gender when providing patient care. Only 24% indicated they had some formal or continuing education on the topic. Respondents indicated interest in educational opportunities for SGBM in the form of online modules or lectures.
Conclusion: Though faculty respondents endorsed SGBM, few have had formal education related to the topic. Faculty development on SGBM may close knowledge gaps and facilitate integration of this curriculum. The survey tool developed through this project may be useful for other institutions engaged in similar efforts related to SGBM.
Sex and gender influence underlying risk factors, pathogenesis, presentations, and therapeutic responses to disease states.1-2 The impact of sex and gender is underanalyzed in medical literature and is not universally apparent in medical school curricula. This absence has implications for patient treatment and outcomes.3-5 For example, there are significant differences in presentation of myocardial infarction, efficacy of aspirin, and response to warfarin and tissue plasminogen activator between males and females, thus considerations surrounding sex and gender are important in forming a treatment plan.6-7
Though advocates have made great strides in incorporating sex and gender successfully into some medical school curricula, large-scale, systematic integration of this content appears to be lacking in undergraduate and graduate medical education.8-10 Residents from multiple specialties were surveyed in a study conducted at Mayo Clinic assessing knowledge and experience with sex and gender topics. Of those surveyed, 16% reported having no instruction on how sex and gender impact their treatment of a patients and 55% reported only occasional instruction on this topic.11 Though medical learners (students and residents) see the importance of sex and gender content, it is clear this information is missing throughout training physicians' learning experiences. 12
Much of the work on sex and gender in medical education has focused on curricular reform as the solution to increasing learner knowledgeability on this topic. Currently many curricular change initiatives use a bottom-up approach, depending on learner and faculty advocates to pressure their institutions to incorporate more sex and gender-based medicine (SGBM) topics in the curriculum.13-14 Faculty and institutional attitudes toward SGBM need to be considered to create sustainable change in viewing medicine through a sex and gender lens.5,14
Slow adoption of SGBM topics by medical school curriculum may be explained by Fredric Hafferty’s theory of medical curricular change. According to Hafferty, a curriculum can be implicit, explicit, or hidden. This theory suggests the most effective way to change a curriculum is to first understand and influence the hidden curriculum, or the "set of influences that function at the level of organizational structure and culture."15 The faculty of an institution are main drivers of its values and culture, thus understanding faculty attitudes and knowledge may lead to insight into the hidden curriculum surrounding SGBM and how to begin to shift this paradigm to curricular inclusion of SGBM and to make this curriculum explicit.16
To our knowledge, no study has yet examined the knowledge and attitudes of medical school faculty about SGBM. This knowledge could be critical in further understanding the barriers to incorporation of this information in curriculum and research and inform future approaches. Whether faculty gender plays a role in SGBM teaching and curriculum has not been well explored. Our study sought to describe the knowledge and attitudes about sex and gender curriculum within a single medical school using a pilot survey.
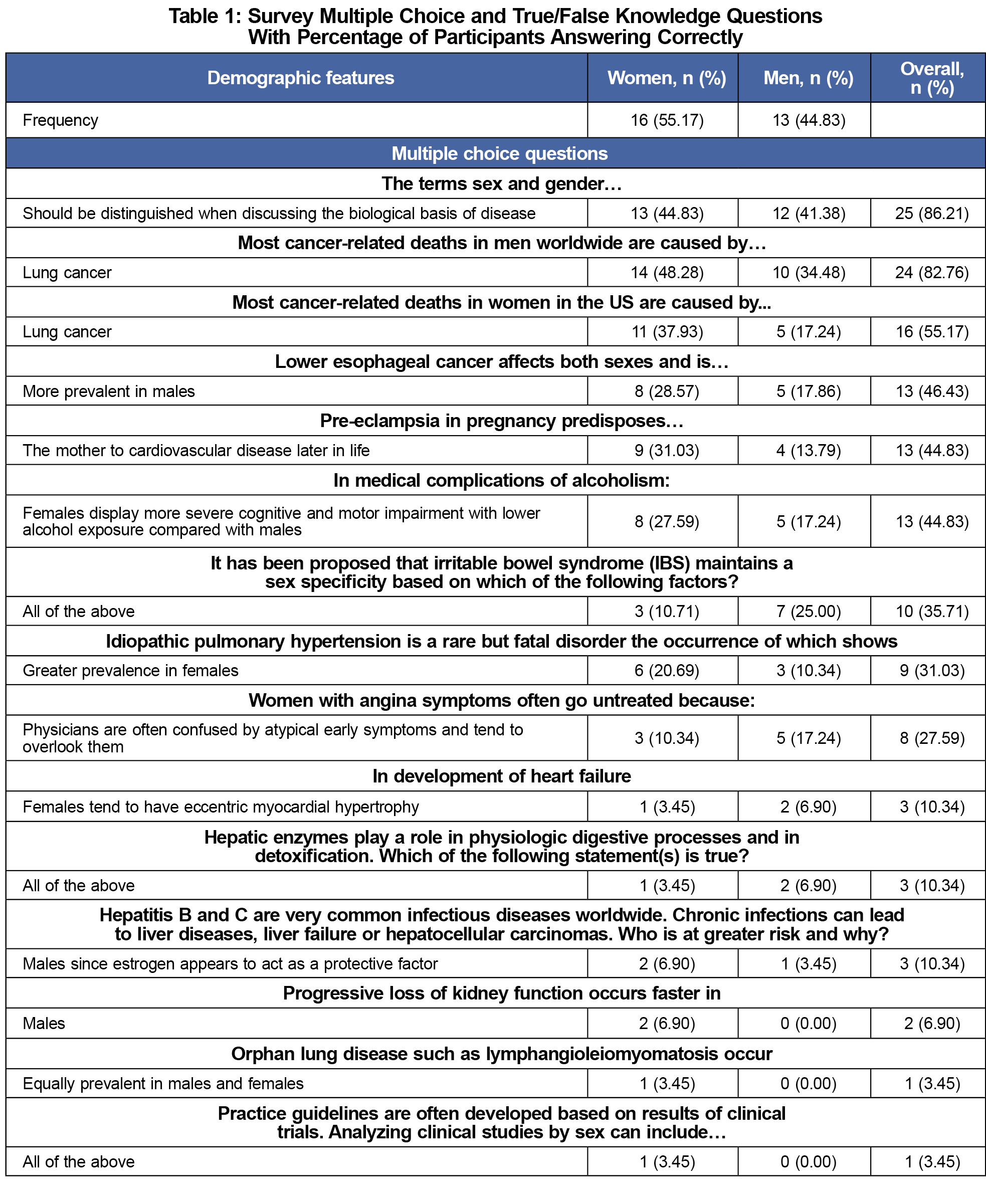
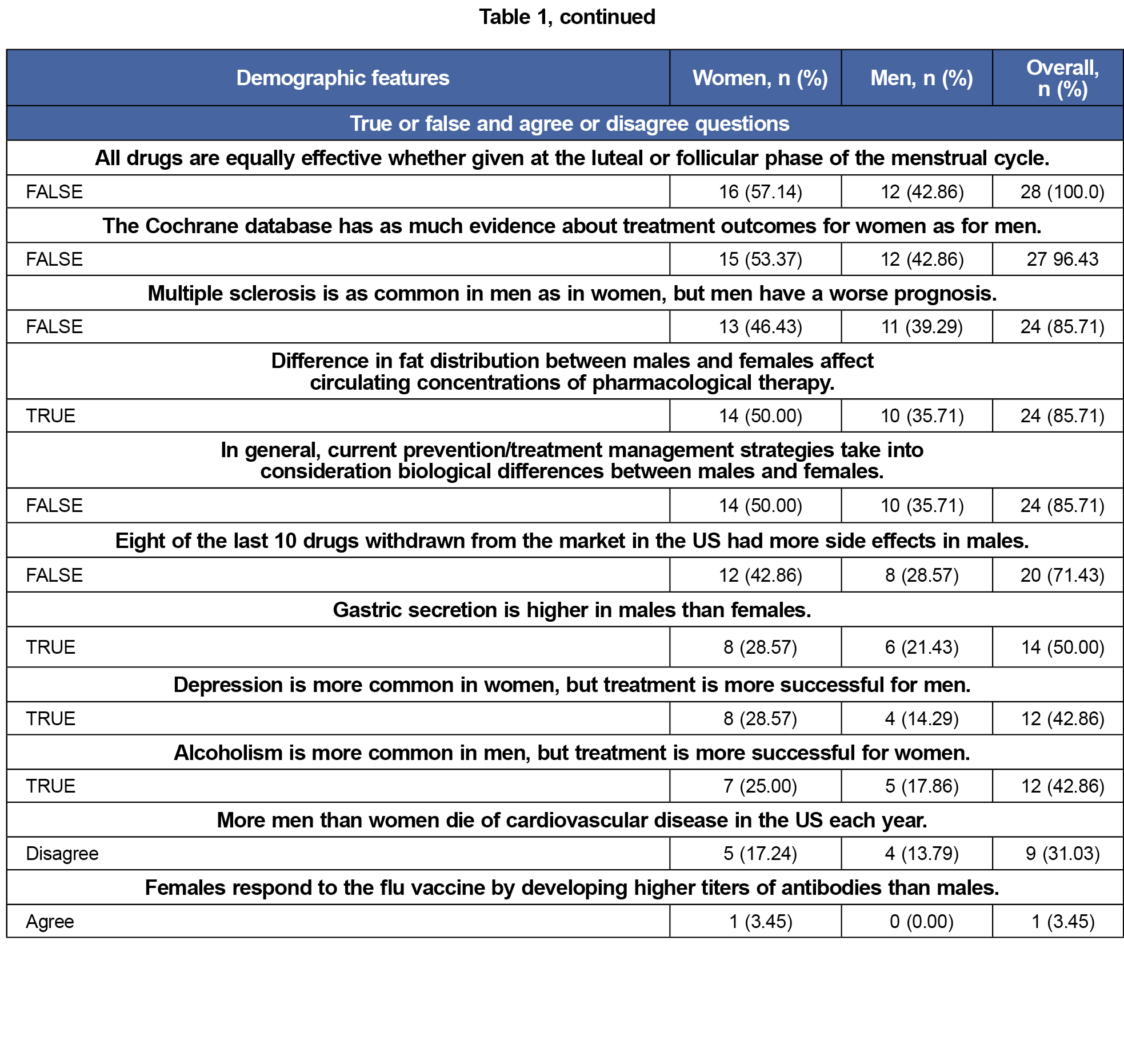
We developed a pilot survey with 39 questions adapted from two previously published survey tools used in medical student and resident populations by one of the study authors.10-11 Since no validated questionnaire existed to test our hypothesis, we developed a new questionnaire. This instrument was refined and validated through an iterative process with input from faculty members who were not part of the study team. The survey consisted of demographic and attitude questions including gender, 17 multiple-choice, knowledge-based questions, and 11 true or false knowledge-based questions. Knowledge questions covered examples of sex and gender differences across systems and specialties.
The survey (available upon request) was administered to all clinical faculty members employed by Western Michigan University Homer Stryker M.D. School of Medicine (WMed). WMed is a private institution located in Kalamazoo, Michigan that has implemented SGBM coursework into the undergraduate curriculum beginning in 2017. The survey was administered by email with an additional follow-up email sent 2 weeks later. We collected and stored responses using REDCap software. This is study was approved by the Institutional Review Board of WMU Homer Stryker M.D. School of Medicine (WMed-2021-0764).
Of 158 pilot surveys, 38 were completed yielding a response rate of 24.05%. Respondents answered an average of 48.53% of the knowledge questions correctly. We performed a two independent samples t test to determine if the overall knowledge score differed between men and women faculty members. With a corresponding P value of 0.2732, there is insufficient evidence that the mean percent knowledge score differs depending on gender.
When asked how important considering sex and gender is when providing patient care, 39.47% of respondents chose very important, 31.58% chose important, and 2.63% chose neutral. Table 1 shows survey question responses. Only 25% of respondents indicated they had some formal or continuing education on SGBM topics. Faculty respondents considered SGBM to be important, with 71% indicating it was important or very important to consider sex and gender when providing patient care. However, only 25% indicated they had some formal or continuing education on the topic.
The pilot survey adapted for faculty was demonstrated as a tool to assess faculty knowledge and attitudes towards SGBM. This complements previous surveys that have examined SGBM in resident and medical student populations. Faculty answered nearly half of the knowledge questions correctly, indicating an opportunity for faculty education surrounding these topics, and they considered the topic to be important. SGBM knowledge did not differ between men and women faculty members, suggesting that this gap is an educational rather than gender-based gap. Few faculty members had formal or continuing education on the topic despite reporting this as an important topic. With high interest levels and relatively low professional exposure and opportunities to improve knowledge, faculty continuing professional development should be considered as an area of focus to advance adoption of an SGBM medical school curriculum. Our study consisted of survey-based research limited to a single institution at a single point in time with a limited response rate. Further exploration of faculty knowledge gaps is needed with a greater response rate and encompassing more than a single medical school to determine generalizability of these findings. Nonetheless, a pilot developed survey has the potential to identify needed professional development to address gaps.



There are no comments for this article.