Introduction: Physicians frequently face challenging conversations, yet medical education often inadequately prepares them for discussions on health literacy, behavior change, and end-of-life care. To bridge this gap, the Medical College of Wisconsin created the "Mastering the Difficult Conversations" online elective for senior medical students. This study analyzes the course's effectiveness in enhancing communication skills training.
Methods: A 4-week, online elective utilized interactive workshops and formative Objective Structured Clinical Examinations (OSCEs) addressing four themes: overcoming health literacy barriers, managing agitated patients, inspiring behavior change, and delivering bad news. Students engaged in prereading, role play, and reflection. Zoom-based OSCEs with standardized patients and faculty provided immediate feedback. We analyzed qualitative data from 35 reflection papers over 4 years and quantitative standardized assessment data.
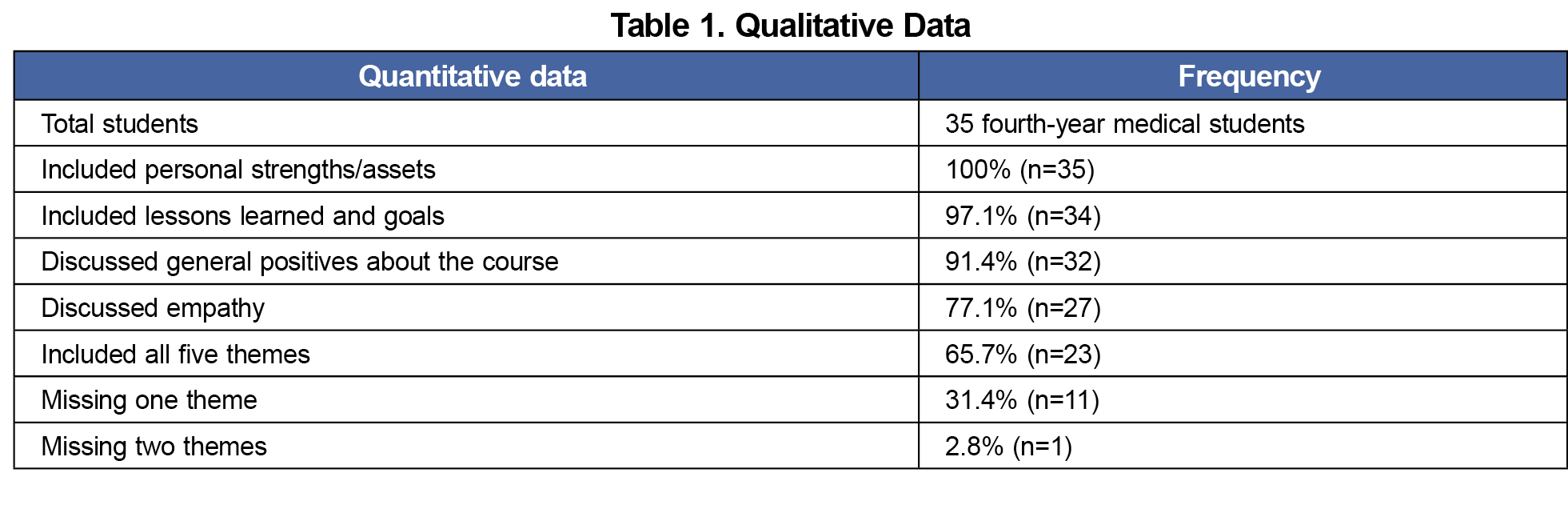
Results: Results indicated five primary themes from reflection papers: goals, empathy, lessons learned, identified strengths, and positive remarks. Anonymous evaluations showed high student satisfaction, with the course meeting its objectives of enhancing communication skills and professionalism.
Conclusion: This study confirms that a structured communication program with interactive discussions and formative OSCEs improves medical students' preparedness for difficult patient interactions. The Zoom-based format proved a viable and favorably rated educational tool, replicable across distances. Despite limitations such as sample size and the need for longitudinal data, these findings highlight the importance of expanding structured communication curricula to enhance patient outcomes and physician well-being.
Physicians frequently engage in challenging conversations with patients, yet most learn these skills informally during residency. While some medical schools include communication curricula, these are often limited to didactic lectures on communication "pearls," leaving graduates underprepared for real-world interactions.1 A national survey found that fewer than one-third of physicians received formal training in discussing end-of-life care, and many overestimate their competence without structured training.2
Evidence supports the effectiveness of communication skills training in improving patient care outcomes.3 Research demonstrates that training enhances physician empathy, reduces burnout, and improves treatment adherence.4,5 Physicians who communicate effectively foster better patient understanding, leading to improved health outcomes, stronger physician-patient relationships, and increased patient satisfaction.5,6
In light of these established benefits, a concerning gap was identified at the Medical College of Wisconsin through exit interviews with its fourth-year students. Many expressed feeling unprepared for common challenging patient interactions anticipated in residency, citing insufficient practical experience with scenarios such as managing agitated patients, inspiring behavior change, overcoming health literacy barriers, and conducting serious illness conversations—interactions they had often only witnessed. This feedback directly spurred the creation of a new curriculum aimed at providing this essential hands-on experience. This initiative developed into the “Mastering the Difficult Conversations” online elective at the Medical College of Wisconsin. In this study, we provide an analysis of the student-perceived effectiveness of the online “Difficult Conversations” course in enhancing communication skills.
Designed for senior medical students who had completed core clerkships, this online elective featured a weekly, interactive workshop and two formative Objective Structured Clinical Examinations (OSCEs), all delivered via the Zoom web meeting platform. Initially adopted due to COVID-19 restrictions, Zoom was retained for its logistical efficiency. This virtual approach not only facilitated simultaneous participation for students across main and rural campuses but also provided consistent training by granting access to highly-trained standardized patients. The Zoom-based format significantly reduced operational costs by eliminating the need for a physical simulation center and associated staff.
Each week started with a workshop on communication strategies including faculty guidance, best practice modeling, and interactive role-play with peer feedback. Students completed assigned readings and a reflection paper before each workshop. "Door notes" for the OSCEs, provided after the workshop gave students background on simulated patients, allowing them to prepare.
OSCEs occurred 2 days postworkshop. Following a brief orientation and an opportunity for preparatory questions, students engaged in a 20-minute OSCE, then received 10 minutes of feedback from standardized patients and faculty. Both assessors completed a Qualtrics-based OSCE assessment before giving verbal feedback, rating communication, patient management, activation, and professionalism. Students then completed a second OSCE case in the same format as above. A group reflection concluded the session, and students submitted an exit survey weekly.
Weekly themes and OSCE scenarios included:
- Week 1 (overcoming health literacy barriers): an illiterate patient with uncontrolled diabetes and coronary artery disease and a cancer patient unaware they were on palliative chemotherapy.
- Week 2 (caring for angry/agitated patients): an angry patient with medication side effects and a manic, tangential patient.
- Week 3 (inspiring behavior change): a manipulative patient with opioid use disorder and an obese patient with psychosocial challenges.
- Week 4 (breaking bad news): a patient discovering an undesired pregnancy preoperatively and an HIV disclosure during a PrEP visit.
Following completion of all OSCEs and workshops, all students completed an ungraded 500-word minimum final reflection paper. Students also completed a required anonymous course evaluation upon completion of the elective.
All course materials, including PowerPoint presentations, OSCE cases, door notes, and assessments, are provided in the STFM CONNECT Medical Student Education Collaborative Library.7
This course study received approval from the Medical College of Wisconsin’s Institutional Review Board. Students were informed about the research via an informational letter and had the option to exclude their data, though none chose to do so. No demographic data were collected; all students were in their final year of training, pursuing a diverse range of specialties.
We conducted a qualitative analysis on 35 mandatory, ungraded final reflection papers (500-word minimum) collected over 4 years. These papers were deidentified prior to analysis. Four independent coders—two faculty members involved with the course and two preclinical students who had not yet taken it—used open coding strategies for a thematic analysis of these reflections.8 The interrater reliability for coding was 0.81, demonstrating very good alignment.9
Content analysis of the students' reflection papers revealed five primary themes: goals, empathy, lessons learned, identified strengths, and general positive remarks about the course (Table 1).
Goals
Most students identified future goals that they would like to pursue as a result of participating in this course. Students often remarked on their need to improve their skill sets in educating patients, taking a history, and agenda setting with a patient. Students also highlighted the need to improve on their tone and style and to work on “self-scripting.” Representative quotes include:
“I also recognize that I need to work on partnering more with my patients when it comes to shared decision making rather than presenting them with a laundry list of options and having them shoot them down one by one.”
“I intend to work on being more tactful, reducing fillers, using open-ended questions to understand where the patient is coming from, and say words or sentences without interruptions so they flow well and convey confidence.”
Empathy
Many students spotlighted empathy as a patient care strength in their response.
“I think one of my strengths that seemed to be mentioned a few times is that I am able to communicate with empathy and let the patient know that I really do care. That makes me happy, because I personally feel that is extremely important in building a strong and successful doctor-patient relationship.”
Other students remarked on the need to work on how they demonstrate empathy to their patients.
“However, I recognize that I do need to work on finding a balance between being empathetic and caring but also making sure that my patient encounters are productive and meet all of their objectives.”
Lessons Learned
The students noted themes around several key lessons learned such as the importance of emotional intelligence and the need to be mindful about timing, shared decision making, and agenda setting.
“Address what the patient wants. It’s easy to be narrowed in on our agenda, but the patient will do what they want to do when they leave and it’s critical to do and answer what the patient wants to know. They will feel unheard if even one small thing that they wanted to know wasn’t addressed. Give them the time and space to express themselves and explain their story.”
Assets/Strengths
All students remarked on assets, most of which focused on their communication skills, empathy, and ability to actively listen as their greatest strengths. Many students also shared that their personal physician-patient style put the patient at ease.
“Expressing empathy and understanding to patients. It was something I was very nervous about, especially in ‘Telemedicine.’ I am glad I was able to express that and remain unbiased.”
General Positive Comments About the Course
Students’ overall satisfaction with the course was positive from a qualitative standpoint. Many students shared that they felt the course should be required (rather than an elective). Students also remarked that the course had an impact on their confidence and, overall, the course was well designed and implemented.
“We learn so much information in medical school, but I feel like we lack in the areas that truly matter. We could all be better medical students/future doctors if we knew how to most effectively communicate with patients, so I think this is a course that we could all benefit from.”
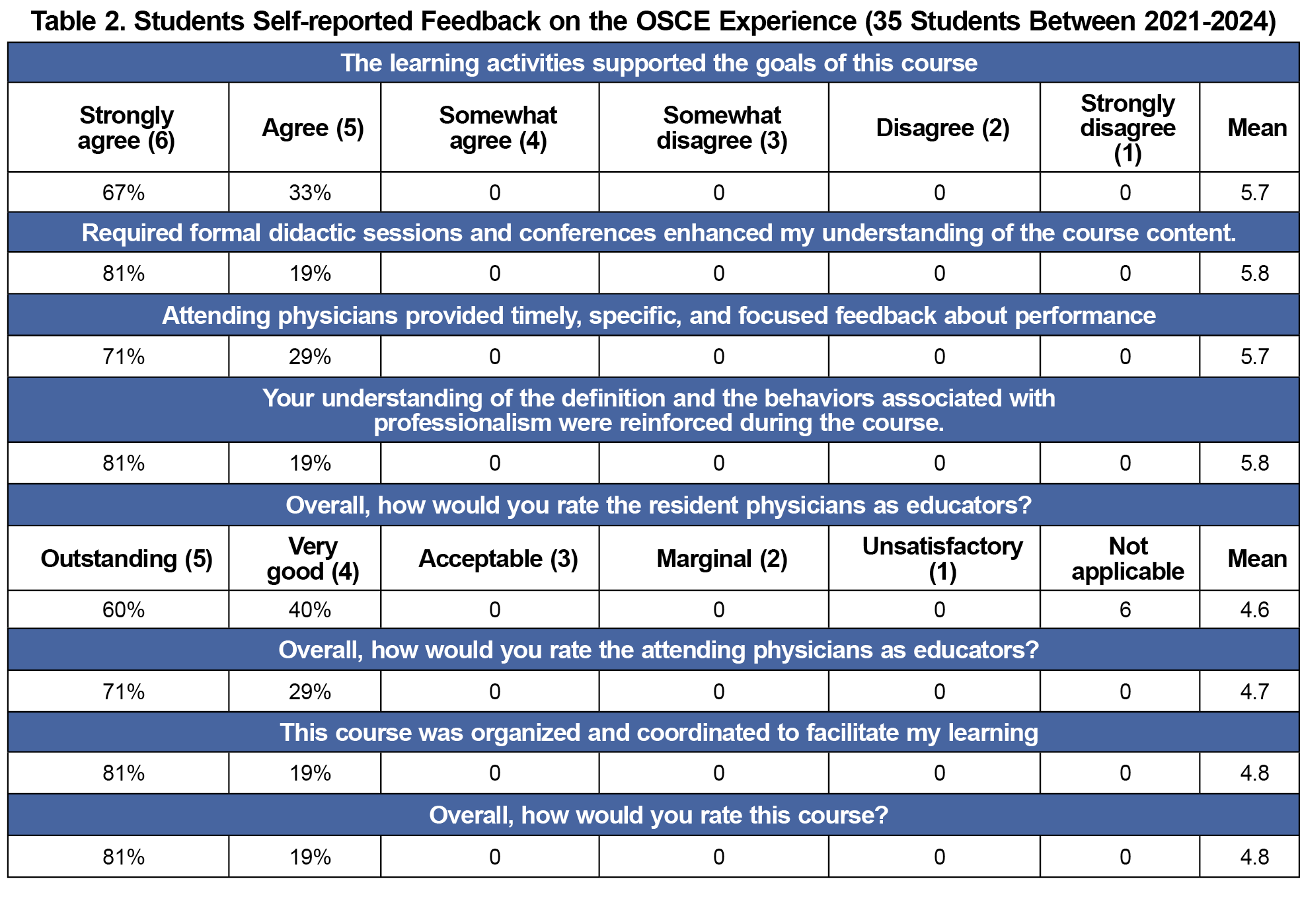
Table 2 presents Likert scale data from MCW's standard anonymous course evaluations. Submitting this evaluation is mandatory for students to receive a grade in any MCW course. Student feedback indicated high ratings for the overall course, faculty members, and organization. Students reported that the course successfully met its educational objectives of enhancing communication skills and that the course reinforced behaviors associated with professionalism.
Our study confirms that a structured communication training program helps medical students feel prepared for difficult patient interactions. The combination of interactive discussions and formative OSCEs allows students to gain hands-on experience and receive targeted feedback in a controlled environment. We also demonstrated that a Zoom-based communication skills course was rated favorably by medical students, indicating that this is a viable educational tool that can be replicated over large geographic distances.
The primary limitation of this study was the small sample size, which may limit generalizability. Additionally, participation was voluntary, introducing potential selection bias. Future research should assess the longitudinal impact of this training, explore its integration at different stages of medical education, and evaluate scalability for broader implementation. Larger sample sizes and multi-institutional studies could help validate the effectiveness of this approach across diverse educational settings.
The course assessed multiple aspects of communication skills using a standardized rubric for each OSCE. However, no statistically significant improvement in these rubric scores was observed over the 4-week elective. This outcome is likely due to two main factors: each OSCE presented a distinct scenario with difficulty levels that varied based on individual students' prior training experiences; and as an elective, students who selected the course likely already possessed stronger baseline communication skills.
Another limitation was the lack of long-term follow-up data to assess how students apply these skills in clinical practice. Future studies should consider tracking students over time to evaluate whether the improvements observed during the course translate into lasting changes in their patient interactions.
Addressing communication training gaps is essential for improving both patient outcomes and physician well-being. Expanding structured communication curricula could better equip future physicians for the challenges they will encounter in clinical practice. As patient-centered care remains a fundamental pillar of medical practice, ensuring that trainees are proficient in difficult conversations is critical to fostering trust, enhancing patient experiences, and ultimately improving health care delivery.
Acknowledgments
Presentations:
- Johnson S. Hayes J. Building the Mastering the Difficult Conversations OSCE course. Academy of Communication in Healthcare: Research Forum. Milwaukee, WI. June 2020 Also presented at . Innovations in Healthcare Education Research Forum, Milwaukee, WI. September 2020
- Hayes J, Diehr S, Ark T, Martens H, Wayne E, Coon L. Lessons Learned From the Mastering Difficult Conversation Course. Innovations in Healthcare Education Research Forum. Virtual. September 2021
- Hayes J, Diehr S, Coon L, Ruffalo L. Mastering the Difficult Conversation OSCEs: How to Prep Students for the Challenges of Real-Life Medicine. Society of Teachers of Family Medicine: Medical Student Education Conference: Virtual. January 2022
Conflict of Interest Statement: The authors have no conflicts of interest to disclose.
References
- Baessler F, Zafar A, Schweizer S, et al. Are we preparing future doctors to deal with emotionally challenging situations? Analysis of a medical curriculum. Patient Educ Couns. 2019;102(7):1304-1312. doi:10.1016/j.pec.2019.02.024
- Fulmer T, Escobedo M, Berman A, Koren MJ, Hernández S, Hult A. Physicians’ views on advance care planning and end-of-life care conversations. J Am Geriatr Soc. 2018;66(6):1201-1205. doi:10.1111/jgs.15374
- Tavakoly Sany SB, Behzhad F, Ferns G, Peyman N. Communication skills training for physicians improves health literacy and medical outcomes among patients with hypertension: a randomized controlled trial. BMC Health Serv Res. 2020;20(1):60. doi:10.1186/s12913-020-4901-8
- Zolnierek KB, Dimatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47(8):826-834. doi:10.1097/MLR.0b013e31819a5acc
- Tallman K, Janisse T, Frankel RM, Sung SH, Krupat E, Hsu JT. Communication practices of physicians with high patient-satisfaction ratings. Perm J. 2007;11(1):19-29. doi:10.7812/TPP/06-106
- Boissy A, Windover AK, Bokar D, et al. Communication skills training for physicians improves patient satisfaction. J Gen Intern Med. 2016;31(7):755-761. doi:10.1007/s11606-016-3597-2
- Hayes J. Mastering the Difficult Conversation OSCE course. STFM CONNECT Medical Student Education Collaborative Library. February 5, 2025. Accessed July 8, 2025. https://connect.stfm.org/viewdocument/mastering-the-difficult-conversatio?CommunityKey=6acfd258-7198-4057-ac5e-d3f1b41620eb&tab=librarydocuments
- Creswell JW. Educational Research: Planning, Conducting, and Evaluating Quantitative and Qualitative Research.Pearson Education Inc; 2008.
- McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22(3):276-282. doi:10.11613/BM.2012.031



There are no comments for this article.