Introduction: Accreditation Council for Graduate Medical Education common requirements mandate that programs recruit and retain a diverse and inclusive workforce of residents. To achieve this aim and align with corresponding institutional equity goals, we developed a multifaceted intervention to recruit and train residents underrepresented in medicine (URiM) at a large academic residency program.
Methods: We implemented a holistic review of residency applications, including de-emphasizing board scores and recommendation letters, blinding academic information, and integrating behavioral-based interview questions. A departmental diversity, equity, and inclusion (DEI) committee member was added to the recruitment committee, all members of which underwent bias training. Updated curricula included DEI training across family medicine disciplines, integration of an advocacy and health equity curriculum, and quality improvement through a health equity lens, among other initiatives.
Results: Over 4 years preintervention, self-identified URiM residents comprised only 6.25% of our program (3/48). Over 4 years postintervention, this percentage increased to 21.15% (11/52, P=.043). We also saw compliance above national specialty mean in ACGME resident surveys in nearly every DEI measurement.
Conclusions: Holistic changes to our recruitment and training efforts and structure had a direct impact on increasing the number of URiM applicants matching to our program. Curricular and institutional changes highlighting our commitment to DEI+ efforts improved our ability to match a diverse group of applicants. Limitations included self-reporting of Electronic Residency Application Service ethnic minority data and determining which of the several simultaneous interventions was most influential.
The Accreditation Council for Graduate Medical Education (ACGME) common requirements1 stipulate that programs must recruit and retain a diverse and inclusive workforce of residents. While family medicine is among the most diverse specialties, in 2019 only 7.8% of family medicine residents were Black and 9.1% were Hispanic.2
In a study on family medicine recruitment, Hogan et al3 found that holistic application review is among the most widely used programs for improving diversity. Wusu and colleagues4 reported that an intervention focused on increasing outreach to candidates underrepresented in medicine (URiM), revision of interviews to minimize bias, and analysis of recruitment data yielded an increase in both the number of URiM applicants and matches to their program.
Despite efforts to increase URiM in family medicine, the need continues for research on how to expand the number of URiM applicants and those matching into family medicine. The University of Michigan family medicine residency program serves a diverse population at two inpatient training sites, including a community-based hospital and the academic institution. Our program has 39 residents at two primary continuity clinics outside Ann Arbor.
Here we report on efforts to improve diversity and equity within our program through recruitment, curricular, and departmental initiatives. Our curriculum-based interventions included integration of longitudinal advocacy, health equity training, and quality improvement through a health equity lens during a monthly department-wide seminar. We also established a recurring grand rounds series dedicated to diversity, equity, and inclusion (DEI) topics, required a DEI teaching element in resident didactics, and expanded our residency curriculum to include training on gender-affirming care, opiate use disorder, and medication-assisted treatment. Every resident didactic and grand rounds presentation was required to include at least one DEI slide.
This paper focuses on our holistic approach to application review and subsequent evaluation of the impact of these changes on the recruitment of residency candidates.
Our recruitment interventions included using a standard CV score (curriculum vitae; Figure 1), which de-emphasized factors such as board scores and recommendation letters in favor of lived experiences. To determine interview selection, an initial holistic review of all applications considered prior experiences, education, medical student performance evaluations, examination scores, transcripts, personal statements, and letters of recommendation. Consistent with a ballot proposal passed in the state of Michigan in 2006 prohibiting the consideration of race in university admissions, we did not filter for race, ethnicity, or gender identity.
All members of the recruitment committee participated in an institutional training course titled Unconscious Bias in Selection and Hiring.5 In our interviews, we also included a member of our department’s DEI committee, who shared equity-focused departmental initiatives with candidates. During interviews, we used standardized questions, including behavioral-based questions. The recruitment team was blinded to academic information until all interviews were complete.
Subsequently, the CV score was applied to all interviewed applicants and used in conjunction with interview and academic scores to determine a composite score. To strengthen reliability, we reviewed scores during weekly meetings to ensure consistency and internal validity across interviewers. The CV score was used to evaluate candidates’ diverse experiences, skills, and backgrounds, giving weight to nonacademic factors such as community college attendance, prior careers, and leadership roles.
Our recruitment efforts coincided with departmental and institutional DEI initiatives, including revising our department’s mission to explicitly state a commitment to health equity, adding department-wide antiracism training, and creating a DEI dashboard to monitor outcomes metrics for these initiatives.
We used two endpoints for analysis: (a) the percentage of self-identified URiM residents (inclusive of Black, Hispanic, or Indigenous American individuals) and self-identified ethnic minority residents (Asian, Middle Eastern, or North African) matching into our program; and (b) compliance with ACGME requirements as measured by annual ACGME resident surveys. This initiative was reviewed by our university’s institutional review board (HUM00263631) and exempted from ongoing review.
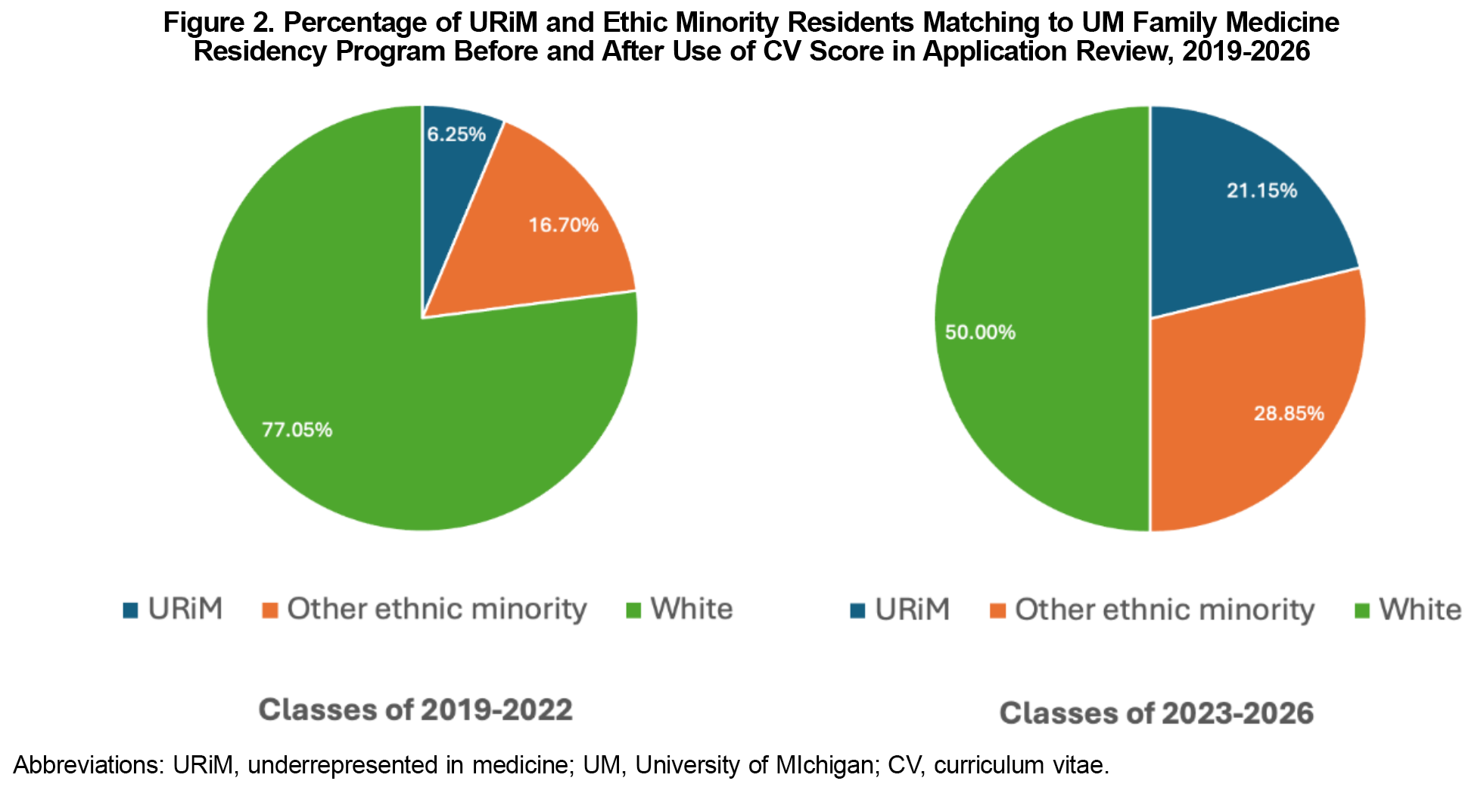
In the 4 preintervention years (2019–2022), URiM residents comprised 6.25% of our 2019–2022 classes (3/48). Over 4 years postintervention, this percentage increased to 21.15% (11/52, P=.043). During the same period, self-identified ethnic minority individuals comprised 22.9% (11/48) of our matched residents preintervention; and postintervention (2023–2026 classes), they comprised 50% (26/52, P=.007; Figure 2).
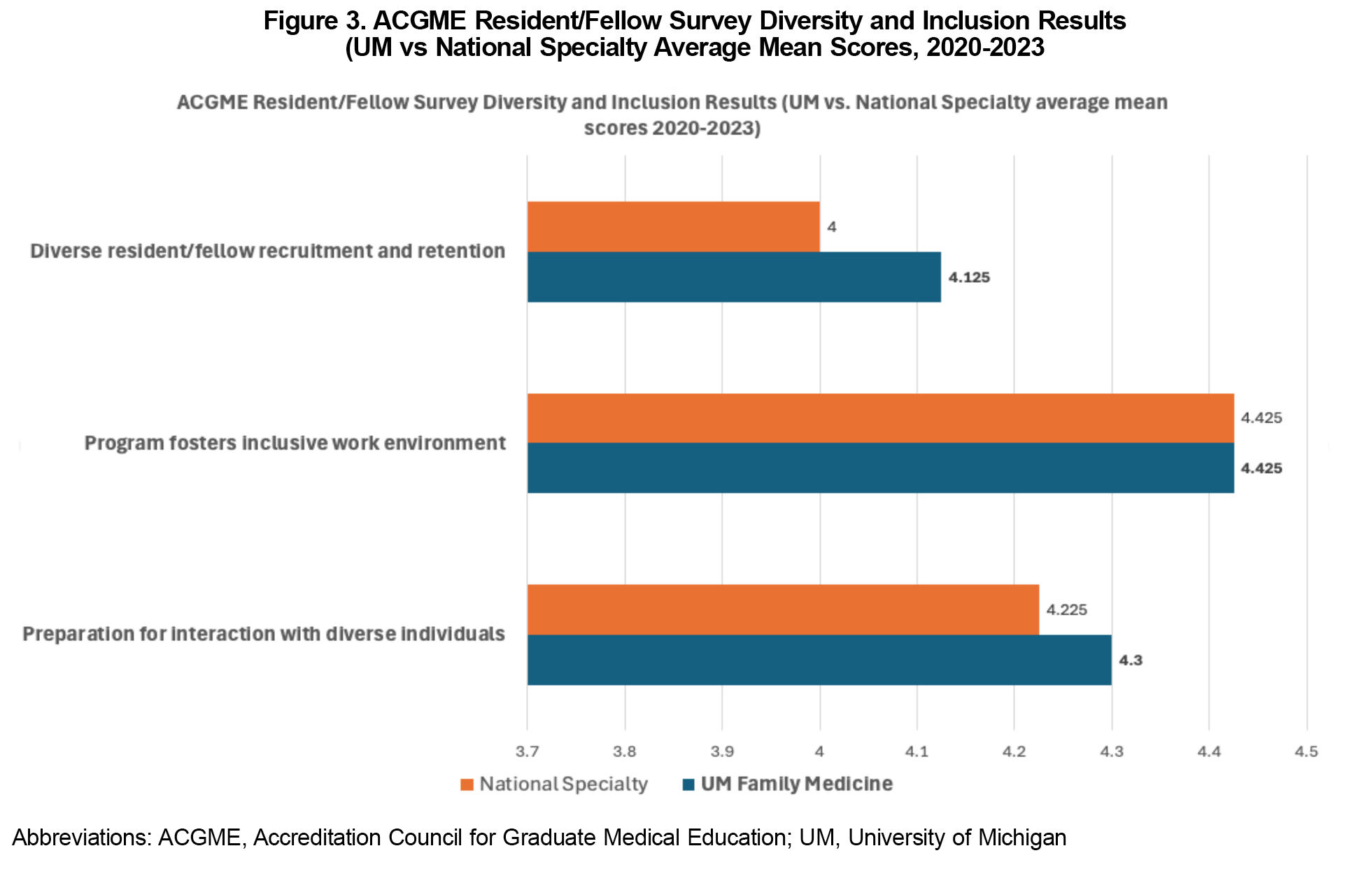
In 2020, the ACGME resident/fellow survey introduced three diversity and inclusion metrics: preparation for interaction with diverse individuals, program fosters inclusive work environment, and diverse resident/fellow recruitment and retention.6 Although comparing these scores pre- and postintervention is not possible, our program scored at or above the national specialty mean in 10 of 12 categories in the 4 years of surveys in the postintervention period (Figure 3).
Our multifaceted intervention, consisting of a holistic review of applications, curriculum changes, and institutional cultural shifts, proved successful in increasing the representation of URiM residents. Our data revealed a cumulative increase from 6.25% URiM residents in the classes of 2019–2022 to 21.15% in the classes of 2023–2026. Overall, ethnic minorities increased from 22.9% to 50%. Including the CV score along with changes in recruitment structure helped directly increase the number of URiM applicants we interviewed. Highlighting our institution’s commitment to DEI+ efforts improved our ability to match a diverse group of applicants.
We recognize the importance of tracking and acknowledging all ethnic groups, especially given the diversity of our patient population. This approach ensures a more inclusive effort toward diversity.
Several limitations existed. In addition to CV scoring, our interventions were multifaceted; attributing causality to individual pieces of our interventions is therefore difficult. Due to the concise nature of this report, we have not provided extensive details on curricular efforts and changes. The impact of these interventions may be diluted if not uniformly adopted or effectively implemented by all facilitators. Successful inclusive teaching seminars and DEI training depend on sustained engagement from faculty and staff. Changing organizational culture and deeply ingrained biases requires ongoing effort that may not yield immediate results. The data are based on Electronic Residency Application Service self-reported ethnic minorities (including Middle Eastern individuals who did not select White), which might affect accuracy. The interventions might not fully address systemic barriers, and determining which aspects of the multiple, simultaneous interventions were most impactful is challenging. A polarized national political landscape and challenges to DEI efforts also pose difficulties for some organizations to implement such changes as easily.
We recommend continued refinement and reinforcement of these interventions. Ensuring consistent implementation is crucial. Maintaining and enhancing engagement through sustained education and training will help solidify gains. Addressing resistance through ongoing dialogue and support also will be essential. Expanding outreach and support systems for URiM and other minority candidates can help mitigate external systemic barriers. Finally, regularly assessing the impact of these interventions using institutional data and climate surveys will ensure that they remain effective and responsive to the evolving needs of our diverse resident population.
Acknowledgments
The authors have no conflicts of interest to declare.
Presentations: This study was presented at the 2024 Society of Teachers of Family Medicine Annual Spring Conference, May 3–8, 2024, in Los Angeles, California.
References
- Accreditation Council for Graduate Medical Education. Common Program Requirements (Residency). ACGME; 2023. Accessed August 19, 2023. https://www.acgme.org/globalassets/pfassets/programrequirements/cprresidency_2023.pdf
- Jabbarpour Y, Westfall J. Diversity in the family medicine workforce. Fam Med. 2021;53(7):640-643. doi:10.22454/FamMed.2021.284957
- Hogan SO, Sangha S, Mason BS. Efforts to recruit diverse resident complements in family medicine. Fam Med. 2023;55(8):518-524. doi:10.22454/FamMed.2023.664616
- Wusu MH, Tepperberg S, Weinberg JM, Saper RB. Matching our mission: a strategic plan to create a diverse family medicine residency. Fam Med. 2019;51(1):31-36. doi:10.22454/FamMed.2019.955445
- University of Michigan Human Resources, Office of Organizational Learning. Unconscious bias in recruiting and hiring. Accessed September 13, 2024. https://hr.umich.edu/working-u-m/professional-development/courses/unconscious-bias-recruiting-hiring
- Artino AR Jr, Malloy K, Miller RS, Kirk LM, Brigham TP. A redesign of the ACGME resident/fellow survey through expert reviews and cognitive interviews. J Grad Med Educ. 2023;15(1):67-73. doi:10.4300/JGME-D-22-00437.1



There are no comments for this article.