Background: The quality of and access to care by lesbian, gay, bisexual, transgender, queer, intersex, asexual, and other sexual and gender diverse (LGBTQIA+) patients is often compromised by physician knowledge deficits, bias, and inadequate training in LGBTQIA+ health. Emergency medicine physicians must be prepared to care for LGBTQIA+ patients, but there is a lack of standardized training in LGBTQIA+ health across emergency medicine residencies. We sought to assess current practices and perform a needs assessment of LGBTQIA+ health teaching across a sample of emergency medicine residencies.
Methods: Residents from five geographically diverse emergency medicine residencies in the United States were invited to complete an online Qualtrics survey between April 2024 and June 2024. The survey included questions regarding the scope of LGBTQIA+ health exposure in residency as well as delivery preferences to improve LGBTQIA+ health teaching within residency curricula.
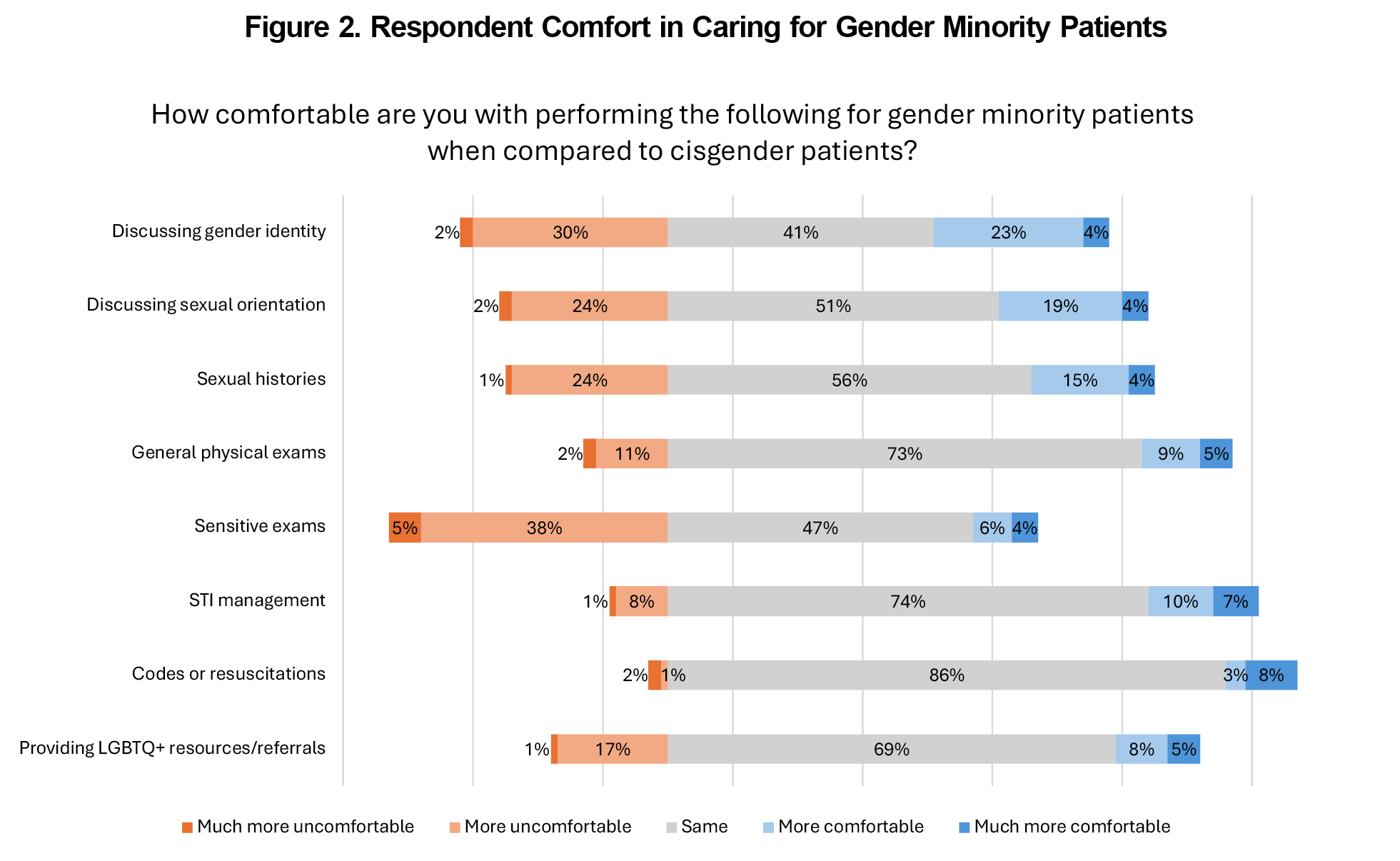
Results: One hundred residents across the five programs participated in the survey (37% response rate). Most residents reported some exposure to gender-affirming language practices and LGBTQIA+ health disparities. Topics with the least reported coverage were pediatric considerations, legal considerations, and taking an organ inventory. Overall, participants were more comfortable performing clinical care for sexual minority patients than gender minority patients. Suggestions for improving LGBTQIA+ health education emphasized the necessity of incorporating LGBTQIA+ health into the core curriculum and including LGBTQIA+ community members and patients into curricular design and delivery.
Conclusions: The results of this study can guide future educational assessment and curricular development efforts to improve LGBTQIA+ health content delivery during emergency medicine residency training.
Lesbian, gay, bisexual, transgender, queer, intersex, asexual, and other sexual and gender diverse (LGBTQIA+) individuals represent a significant minority population facing unique historical and ongoing barriers to equitable health care.1–4 Previous research suggests that stigma, discrimination, and deficits in provider knowledge and competence in caring for LGBTQIA+ populations contribute to patient dissatisfaction, mistrust, and avoidance.5–10 This is especially important in primary care and emergency department settings, which may represent a health care safety net or entry point for patients.
Improving provider education has been proposed as a key mechanism for addressing these disparities.5,11 Within emergency medicine (EM), the EM Model of Clinical Practice began including sexual orientation and gender identity considerations in its guidelines for residency curricula in 2019.12 While the median LGBTQIA+ health curricular time across EM residencies increased from 0 minutes in 2013 to 2 hours in 2020, the follow-up survey revealed that only 75% of programs offered LGBTQIA+ health teaching.13,14
Despite its inclusion in the EM Model, there is a lack of general guidance on delivering LGBTQIA+ health content to EM residents.14,15 Through a pilot needs assessment of resident experiences, comfort and attitudes, and learning preferences, we aim to offer resident-informed recommendations to improve LGBTQIA+ health education.
This cross-sectional study assessed LGBTQIA+ health education within EM residency didactics (ie, conference or classroom based) by surveying EM resident physicians at five large, geographically distinct programs across the United States. While likely underestimates, the 2023 LGBTQIA+ adult population in these programs’ states ranged from 4.5% to 6.5%, with a national average of 5.5%.4 The author-developed survey, modeled after prior instruments,13,14,16,17 evaluated teaching hours, resident comfort and attitudes, covered and desired topics, education modalities, and suggestions for curriculum improvement. Residents were recruited by email from April 2024 to June 2024 and completed the anonymous online survey. The survey instrument and full procedures are available in the Appendix. Study protocols were deemed exempt by the Institutional Review Boards at all sites.
Data management and analysis were performed using STATA 18.0 and Microsoft Excel software. We present descriptive statistics and bivariate analyses conducted using Kruskal-Wallis tests followed by post-hoc Dunn’s pairwise comparisons with Bonferroni correction, as well as multivariate analyses via ordered logistic regression. We summarized free-text suggestions for LGBTQIA+ health curricular development.
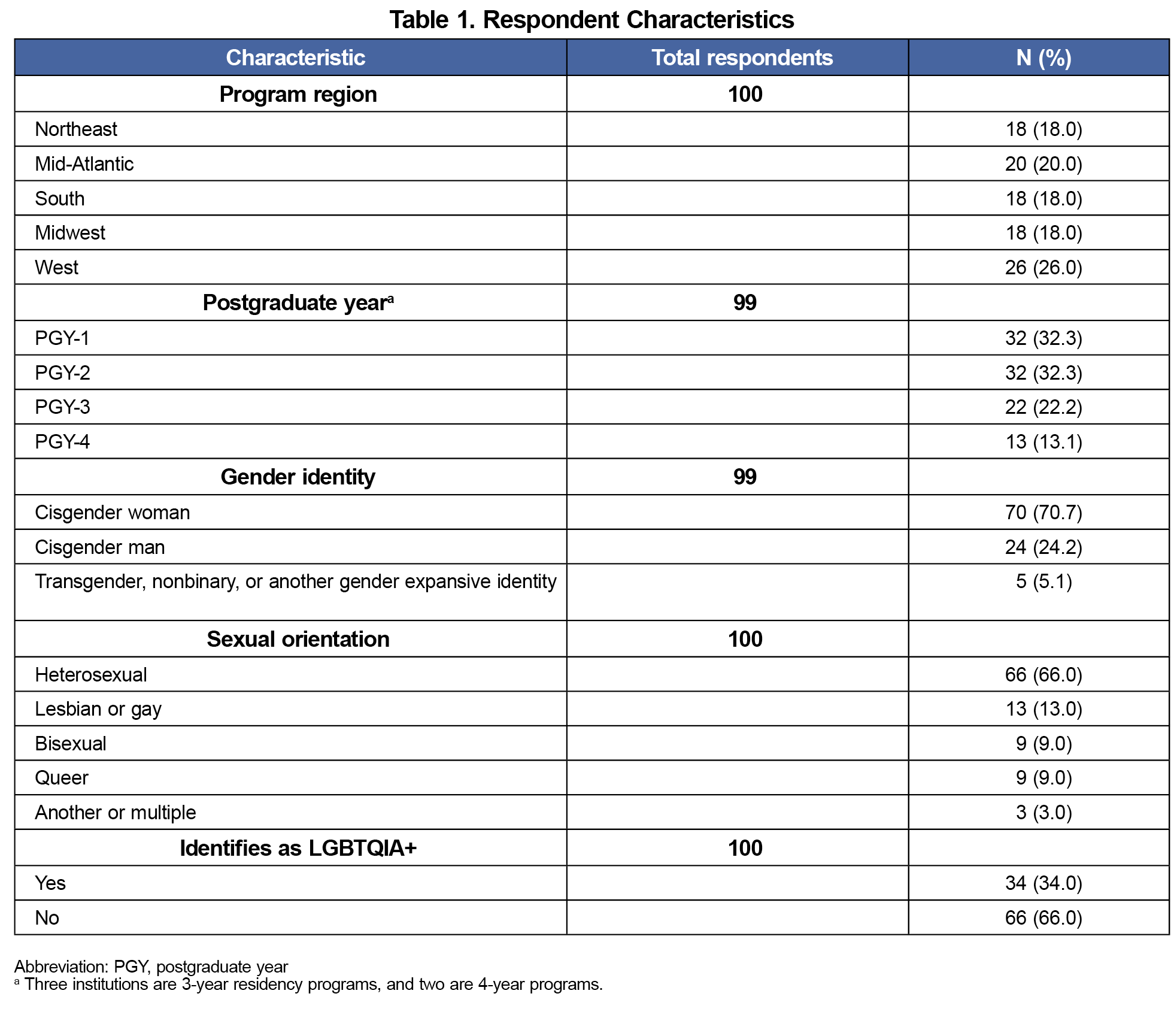
A total of 100 residents participated in the survey, with an overall response rate of 37.0% (range across institutions: 30.5%-48.8%). Most participants were residents in postgraduate year (PGY) 1 or 2 (64.7%), cisgender women (70.7%), and heterosexual (66.0%, Table 1).
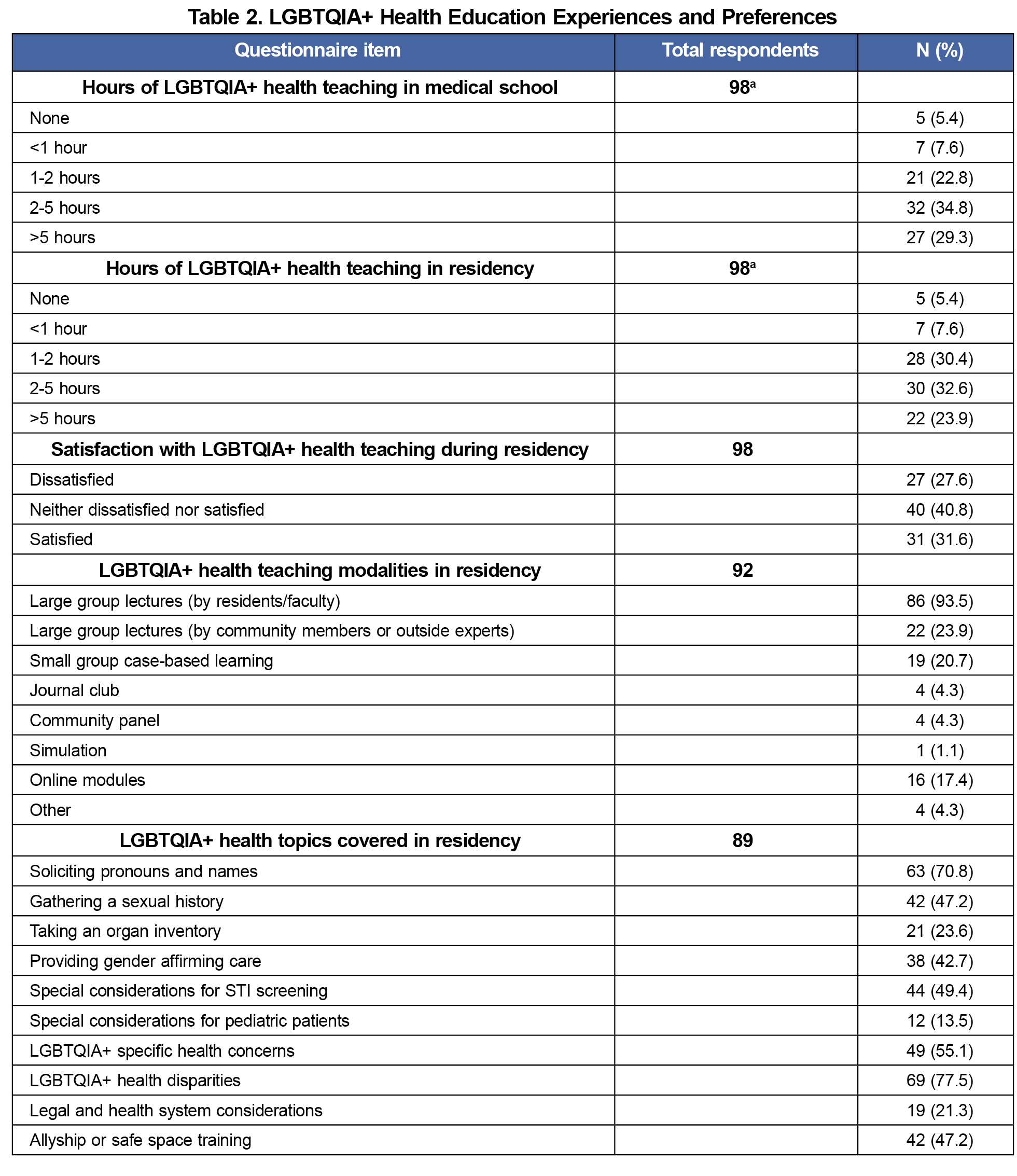
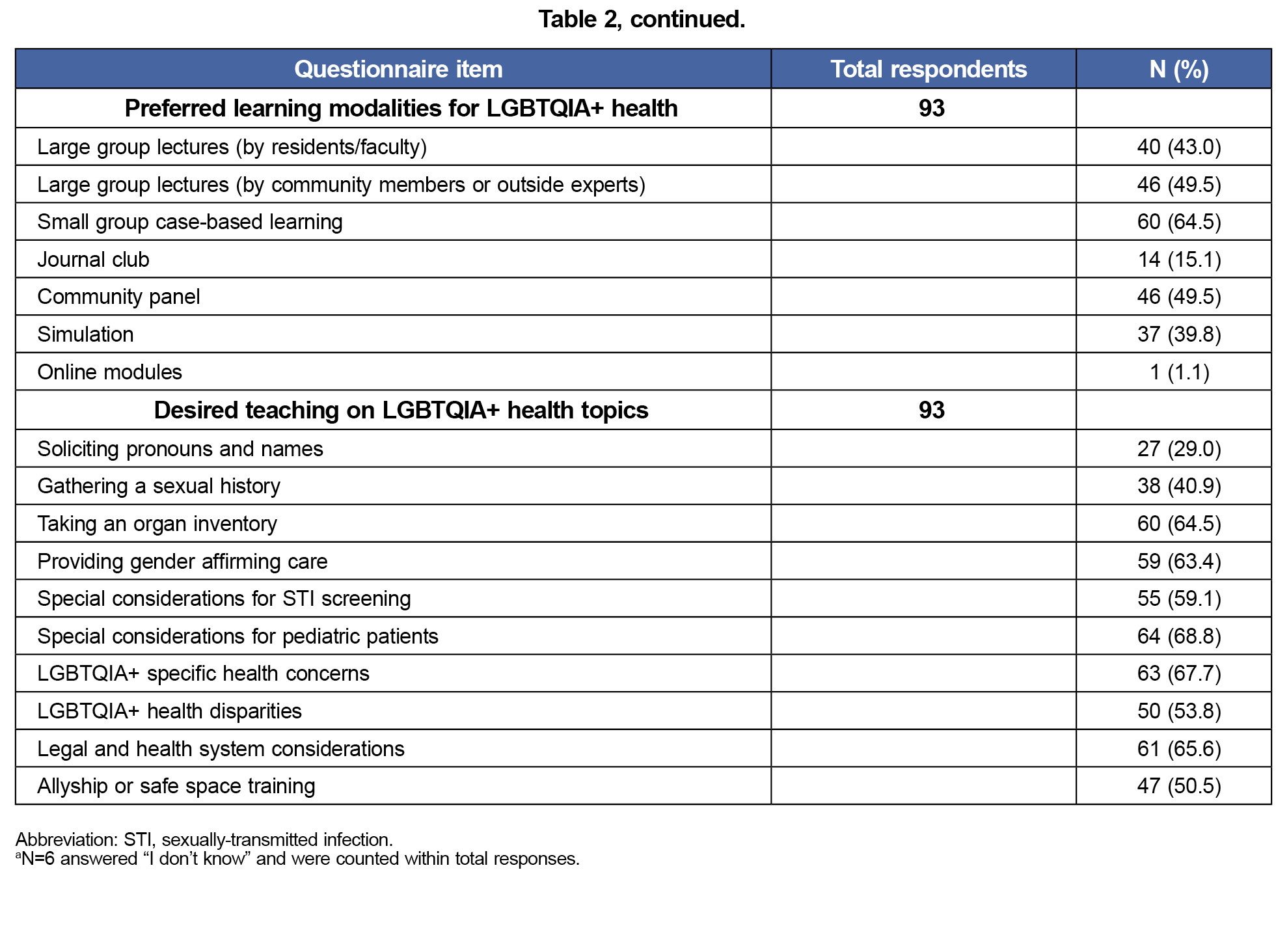
Resident experiences and preferences regarding LGBTQIA+ health content and education modalities are shown in Table 2. Participants reported a median range of 2-5 hours of LGBTQIA+ health teaching in residency; 5.4% reported 0 hours. Residency hours differed by program (H[4] = 17.22, P=.002) and PGY level (H[3] = 27.08, P<.001), but differences in the latter were only significant when comparing PGY-1s to more senior residents. Increased hours were associated with higher satisfaction with LGBTQIA+ health teaching (H[4] = 37.78, p<.001). Satisfaction was not associated with PGY level or gender identity.
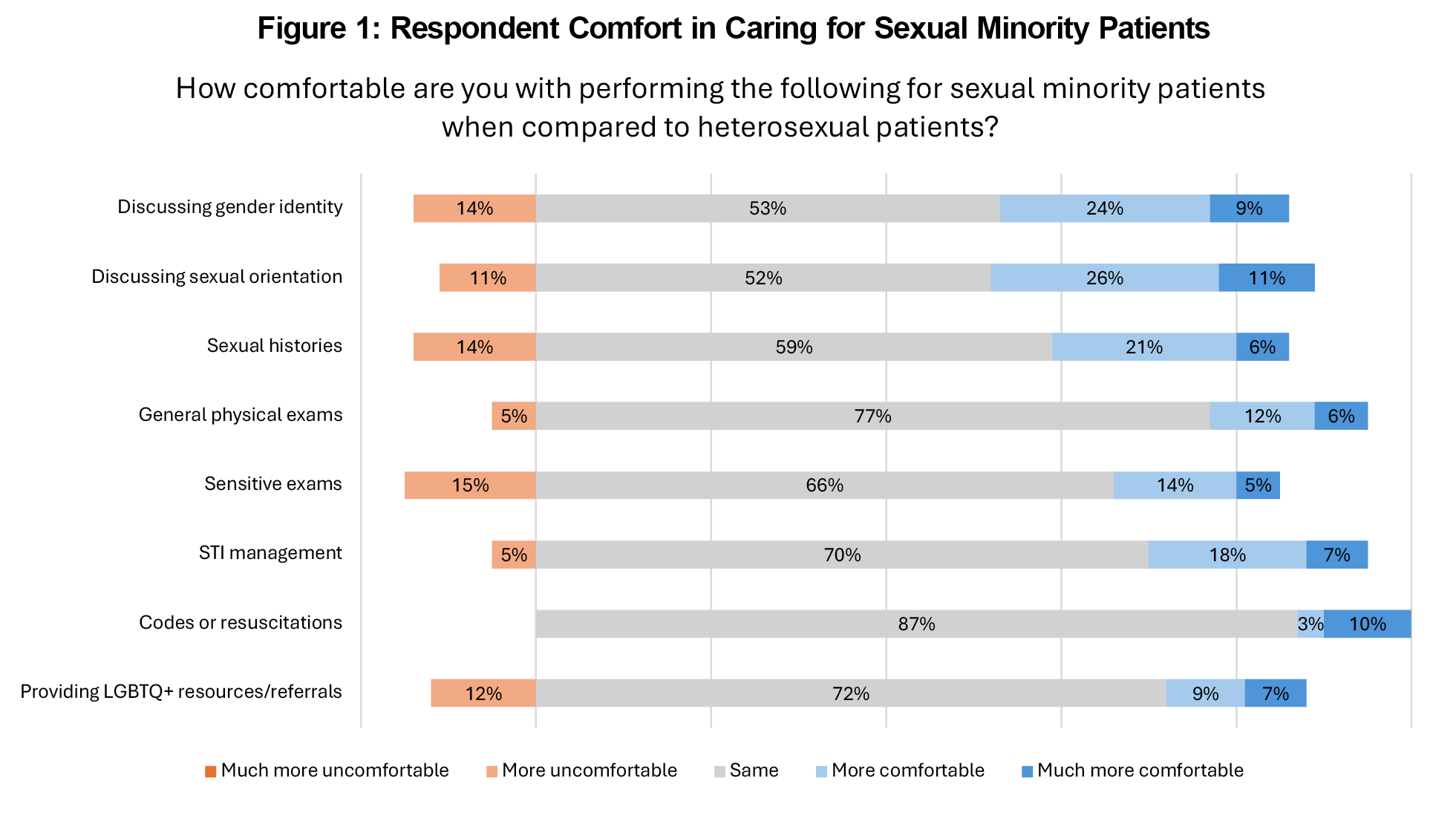
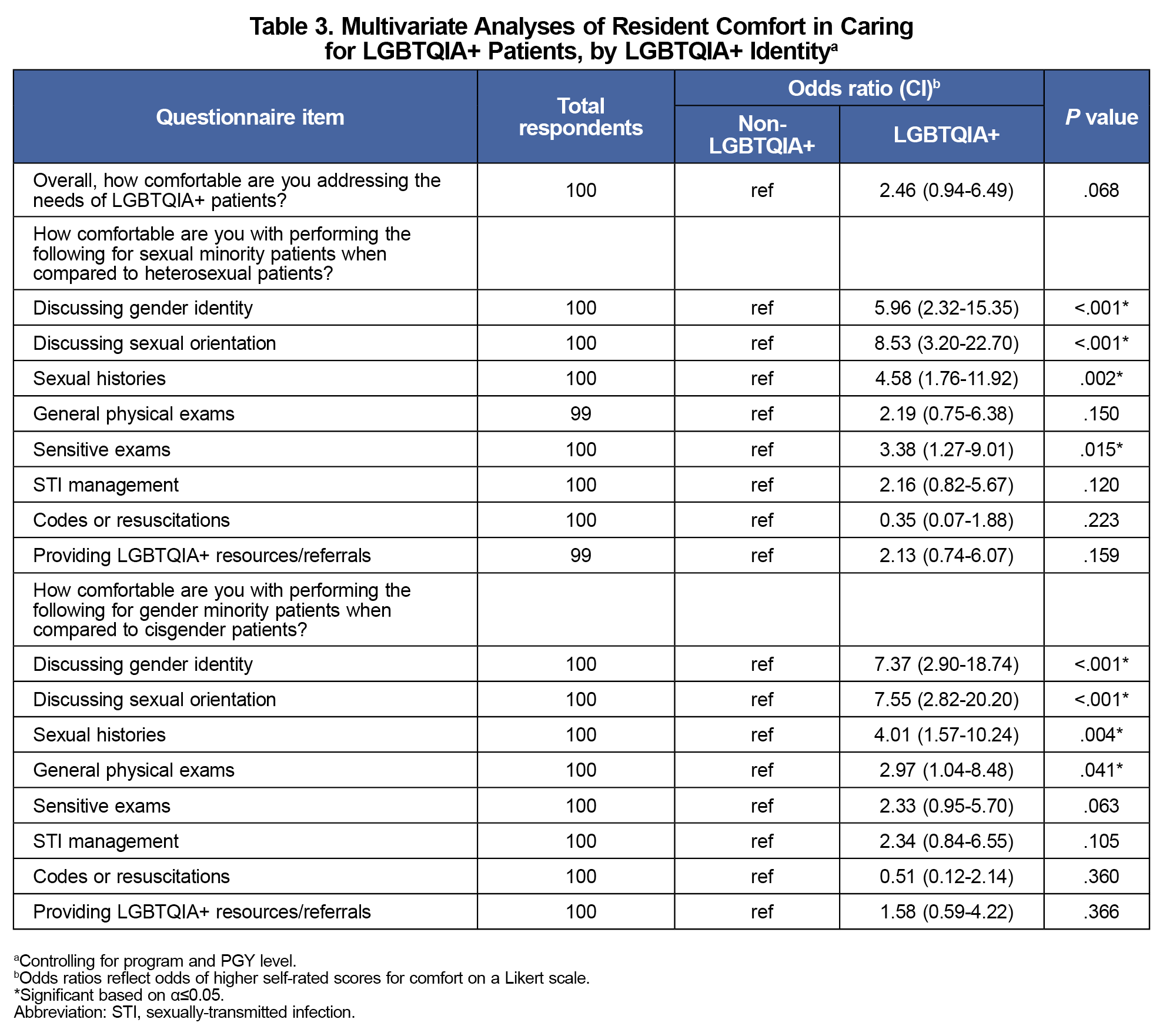
Overall, participants were more comfortable performing clinical care activities for sexual minority patients than gender minority patients (Figures 1 and 2). Multivariate analyses for LGBTQIA+ status controlling for program and PGY level show an overall trend of increased comfort caring for LGBTQIA+ patients among LGBTQIA+ residents (Table 3).
Free-text suggestions (n=18) advocated to increase LGBTQIA+ health content and make core curricula inclusive of sexual and gender minorities. Respondents recommended including LGBTQIA+ community members in curriculum design and delivery, such as through panels, small group discussions, and direct patient interactions. Several called for enhancing transgender health education through further training on organ inventories, gender-affirming care, and sensitive exams.
Our study builds on previous work in EM and internal medicine to facilitate LGBTQIA+ curricular implementation and offers resident-facing preferences and recommendations.13,14,16,17
Less than one-third of residents were satisfied with their LGBTQIA+ health education in residency, with increased satisfaction linked to more reported training hours. However, curricular hours must be interpreted with caution, as didactic hours alone may not ensure preparedness or quality education.18
Residents had varying levels of comfort across skills related to the care of LGBTQIA+ patients, but were overall more comfortable caring for sexual minority patients than for gender minorities, as seen in previous research.16 This underscores the need for dedicated education and training in transgender health and gender-affirming care, especially when education interventions aggregate sexual and gender minorities but omit transgender health.11,19
Our subgroup analyses revealed higher comfort levels among LGBTQIA+ respondents across multiple provider tasks when caring for sexual or gender minorities, which may be related to shared experiences and considerations. Improved patient satisfaction and health outcomes related to patient-provider identity concordance has primarily been explored with respect to race, gender, and language; however, emerging research suggests LGBTQIA+ patient-provider identity disconcordance may be related to health care discrimination and care avoidance.20–22 Additionally, areas with low reported comfort among all groups, such as knowledge of LGBTQIA+ resources and referrals, present opportunities for targeted education.
Based on the survey responses and open-ended suggestions, several themes for future curricular development emerged:
- Expand extracurricular basics. Training should move beyond gender-affirming language practices (eg, pronouns) and taking a sexual history. Residents in our sample desired more knowledge particularly in transgender health, pediatric considerations, legal considerations, and LGBTQIA+ specific health concerns.
- Prioritize interactive learning. Whereas large-group lectures are most commonly reported, residents preferred hands-on, interactive modalities, including small-group, case-based learning, simulation, and patient panels. Despite the rising availability of online, asynchronous content, online modules were not a highly desired format. Of note, previous studies showing online modules as a preferred teaching modality are reflective of program director and faculty opinions.23–25
- Integrate content. LGBTQIA+ health considerations should be incorporated throughout the curricula rather than taught in isolation. For example, genitourinary content should not assume a sex binary or heterosexuality.
- Engage external experts and the LGBTQIA+ community. Programs should consider the involvement of external LGBTQIA+ health experts and community members. The lack of content experts is a known barrier to LGBTQIA+ health education.13,26–29
Limitations
This study has several limitations, including the risks of recall and social desirability bias from self-reported data; nonresponse bias due to lower response rates; and effects from residency didactic absences. Our sample overrepresented LGBTQIA+ (34%) and women (70%) compared to 2020 national averages (6.3% and 35%, respectively), and was limited to urban academic centers, which may affect generalizability.30 Using subjective metrics such as comfort may not accurately reflect knowledge and competency. While our survey was EM-specific, these findings may be relevant and applicable to other fields with special interests in population health and health promotion, such as primary care and other ambulatory care settings. Lastly, responses (or the lack thereof) may be affected by the national landscape of increasing anti-LGBTQIA+ legislation.
This pilot needs assessment identifies potential content gaps in education being delivered and suggests that for LGBTQIA+ health education to be more effective in residency programs, it should be comprehensive, community-engaged, and practice-oriented. These findings can guide future research and curricular development efforts for LGBTQIA+ health in graduate medical education.
Acknowledgments
Presentations: Results from this manuscript were presented at the annual CORD Academic Assembly on March 3, 2025 in Seattle, Washington.
Conflict of Interest Disclosure: The authors have no conflicts of interest to report.
References
- Kates J, Ranji U, Beamesderfer A, Salganicoff A, Dawson L. Health and access to care and coverage for lesbian, gay, bisexual, and transgender individuals in the U.S. Kais Fam Found. Published online May 3, 2018. Accessed October 2, 2025. https://www.kff.org/report-section/health-and-access-to-care-and-coverage-lgbt-individuals-in-the-us-the-lgbt-community/
- LGBT - Healthy People 2030. Health.gov. Accessed July 15, 2024. https://health.gov/healthypeople/objectives-and-data/browse-objectives/lgbt
- National LGBTQIA+ Health Education Center. Understanding the Health Needs of LGBT People. The Fenway Institute; 2016. Accessed December 16, 2024. https://www.lgbtqiahealtheducation.org/publication/understanding-health-needs-lgbt-people/
- Flores AR, Conron KJ. Adult LGBT Population in the United States. Williams Institute. Accessed December 16, 2024. https://williamsinstitute.law.ucla.edu/publications/adult-lgbt-pop-us/
- Kruse MI, Bigham BL, Voloshin D, Wan M, Clarizio A, Upadhye S. Care of sexual and gender minorities in the emergency department: a scoping review. Ann Emerg Med. 2022;79(2):196-212. doi:10.1016/j.annemergmed.2021.09.422
- Jalali S, Sauer LM. Improving care for lesbian, gay, bisexual, and transgender patients in the emergency department. Ann Emerg Med. 2015;66(4):417-423. doi:10.1016/j.annemergmed.2015.02.004
- Bauer GR, Scheim AI, Deutsch MB, Massarella C. Reported emergency department avoidance, use, and experiences of transgender persons in Ontario, Canada: results from a respondent-driven sampling survey. Ann Emerg Med. 2014;63(6):713-20.e1. doi:10.1016/j.annemergmed.2013.09.027
- Campbell J, Nathoo A, Chard S, Messenger D, Walker M, Bartels SA. Lesbian, gay, bisexual, transgender and or queer patient experiences in Canadian primary care and emergency departments: a literature review. Cult Health Sex. 2023;25(12):1707-1724. doi:10.1080/13691058.2023.2176548
- Nowaskie DZ, Sowinski JS. Primary care providers’ attitudes, practices, and knowledge in treating LGBTQ communities. J Homosex. 2019;66(13):1927-1947. doi:10.1080/00918369.2018.1519304
- Casey LS, Reisner SL, Findling MG, et al. Discrimination in the United States: experiences of lesbian, gay, bisexual, transgender, and queer Americans. Health Serv Res. 2019;54(Suppl 2)(suppl 2):1454-1466. doi:10.1111/1475-6773.13229
- Streed CG Jr, Davis JA. Improving clinical education and training on sexual and gender minority health. Curr Sex Health Rep. 2018;10(4):273-280. doi:10.1007/s11930-018-0185-y
- Beeson MS, Ankel F, Bhat R, et al; 2019 EM model review task force; american board of emergency medicine. The 2019 model of the clinical practice of emergency medicine. J Emerg Med. 2020;59(1):96-120. doi:10.1016/j.jemermed.2020.03.018
- Moll J, Krieger P, Moreno-Walton L, et al. The prevalence of lesbian, gay, bisexual, and transgender health education and training in emergency medicine residency programs: what do we know? Acad Emerg Med. 2014;21(5):608-611. doi:10.1111/acem.12368
- Moll J, Vennard D, Noto R, et al. The prevalence of lesbian, gay, bisexual, and transgender health education and training in emergency medicine residency programs: where are we now? AEM Educ Train. 2021;5(2):e10580. doi:10.1002/aet2.10580
- Hsiang E, Ritchie AM, Lall MD, et al. Emergency care of LGBTQIA+ patients requires more than understanding the acronym. AEM Educ Train. 2022;6(S1)(suppl 1):S52-S56. doi:10.1002/aet2.10750
- Moll J, Krieger P, Heron SL, Joyce C, Moreno-Walton L. Attitudes, behavior, and comfort of emergency medicine residents in caring for lgbt patients: what do we know? AEM Educ Train. 2019;3(2):129-135. doi:10.1002/aet2.10318
- Suarez S, Lupez E, Demers L, Streed CG Jr, Siegel J. gender and sexual diverse health education: a needs assessment among internal medicine residents. LGBT Health. 2022;9(8):589-594. doi:10.1089/lgbt.2022.0058
- Pregnall AM, Churchwell AL, Ehrenfeld JM. A call for LGBTQ content in graduate medical education program requirements. Acad Med. 2021;96(6):828-835. doi:10.1097/ACM.0000000000003581
- Dubin SN, Nolan IT, Streed CG Jr, Greene RE, Radix AE, Morrison SD. Transgender health care: improving medical students’ and residents’ training and awareness. Adv Med Educ Pract. 2018;9:377-391. doi:10.2147/AMEP.S147183
- Liu M, Patel VR, Sandhu S, Reisner S, Keuroghlian AS. Health care discrimination and care avoidance due to patient-clinician identity discordance among sexual and gender minority adults. Ann Fam Med. 2024;22(4):329-332. doi:10.1370/afm.3130
- Takeshita J, Wang S, Loren AW, et al. Association of racial/ethnic and gender concordance between patients and physicians with patient experience ratings. JAMA Netw Open. 2020;3(11):e2024583. doi:10.1001/jamanetworkopen.2020.24583
- Lor M, Martinez GA. Scoping review: definitions and outcomes of patient-provider language concordance in healthcare. Patient Educ Couns. 2020;103(10):1883-1901. doi:10.1016/j.pec.2020.05.025
- Jia JL, Nord KM, Sarin KY, Linos E, Bailey EE. Sexual and gender minority curricula within us dermatology residency programs. JAMA Dermatol. 2020;156(5):593-594. doi:10.1001/jamadermatol.2020.0113
- Grimstad FW, Satterwhite CL, Wieneke CL. Assessing residency program approaches to the transgender health CREOG objective. Transgend Health. 2016;1(1):69-74. doi:10.1089/trgh.2015.0011
- Goetz TG, Nieman CL, Chaiet SR, Morrison SD, Cabrera-Muffly C, Lustig LR. Sexual and gender minority curriculum within otolaryngology residency programs. Transgend Health. 2021;6(5):267-274. doi:10.1089/trgh.2020.0105
- Bunting SR, Goetz TG, Gabrani A, Blansky B, Marr M, Sanchez NF. Lesbian, gay, bisexual, transgender, and queer (LGBTQ+) health education in primary care graduate medical education programs: a national survey of program directors. Ann LGBTQ Public Popul Health. 2022;3(4):242-259. doi:10.1891/LGBTQ-2021-0027
- Guerrero-Hall KD, Muscanell R, Garg N, Romero IL, Chor J. Obstetrics and gynecology resident physician experiences with lesbian, gay, bisexual, transgender and queer healthcare training. Med Sci Educ. 2021;31(2):599-606. doi:10.1007/s40670-021-01227-9
- Vinekar K, Rush SK, Chiang S, Schiff MA. Educating obstetrics and gynecology residents on transgender patients: a survey of program directors. Obstet Gynecol. 2019;133(4):691-699. doi:10.1097/AOG.0000000000003173
- Donovan M, VanDerKolk K, Graves L, McKinney VR, Everard KM, Kamugisha EL. Gender-affirming care curriculum in family medicine residencies: A CERA study. Fam Med. 2021;53(9):779-785. doi:10.22454/FamMed.2021.764850
- Lall MD, Bilimoria KY, Lu DW, et al. Prevalence of discrimination, abuse, and harassment in emergency medicine residency training in the US. JAMA Netw Open. 2021;4(8):e2121706. doi:10.1001/jamanetworkopen.2021.21706



There are no comments for this article.