Introduction: The association between health care payor source and HbA1c in patients with type 2 diabetes (T2D) treated at federally qualified health centers (FQHCs) has been evaluated only in cross-section. FQHCs provide an opportunity to compare the association of glycemic control between populations with or without public or private insurance followed over time.
Methods: In this observational study of primary care data, we compared HbA1c values by antecedent insurance status among adults with T2D, before and after adjustment for age, sex, and primary spoken language.
Results: Among 9,848 patients evaluated, mean HbA1c differed (P<.05 for each pair except Medicaid vs self-pay) by payor source with Medicare patients having the lowest (7.44%), Medicaid the highest (8.01%), and privately insured (7.84%) and self-pay patients (7.99%) intermediate. Greater age and being female (P<.001) were associated with lower HbA1c. Language was independently associated with HbA1c (P<.001), with Spanish-speaking patients having the highest HbA1c (7.97%), English-speakers intermediate (7.92%), and others lowest (7.46%) (Spanish vs English not significant, others P<.05). Age, sex, language, clinic location, time between first and last visits, and number of visits were each associated with HbA1c, but in a fully adjusted model, significant differences by payor group persisted.
Conclusion: In this study of FQHCs patient data, HbA1c measured after nearly 2 years of payor source observation differed by payor. Measured covariates did not fully explain the differences. Uninsured patients and those with Medicaid had worse HbA1c than those with Medicare or private insurance. These results may be used to inform another study with more available variables to determine what specific factors may mediate the association between payor source and HbA1c.
Health care in the United States is paid for by private insurance, public insurance (mainly Medicare and Medicaid), and patients themselves. Publicly insured patients are more likely to report having chronic conditions than privately insured patients.1
Hemoglobin A1c (HbA1c) is used as a management indicator in patients with type 2 diabetes (T2D).2 Routinely testing HbA1c can aid patients in preventing and delaying complications.3-6 Maintaining HbA1c below 7% is associated with reduced rates of T2D-related complications.7
Data from the NHANES 2017 - March 2020 showed insured adults with T2D had greater health care utilization and better glycemic control compared to uninsured adults with T2D.8 Specifically in federally qualified health centers (FQHCs), where many patients have public insurance or are uninsured, diabetes education can help lower HbA1c.9
To our knowledge, while others have examined insurance status and quality of diabetes care cross-sectionally in FQHCs,9,10,11 no study evaluates glycemia by antecedent payor source. Here we report on an observational study of patient record data in which we evaluated HbA1c and payor source prior to the HbA1c determination.
We collected data from the electronic medical record (EMR) on all adult (>18 years old) patients with T2D seen at least twice for primary care between January 1, 2018, and December 31, 2021, within the Valleywise Health system of 12 FQHCs, in the Phoenix, Arizona area. This date range was chosen due to clinic consolidations outside of this period.
Each participant must have had at least two visits, with an HbA1c drawn at the last visit, which was the end date for our observation. To account for the longitudinal effects of coverage on HbA1c, we used the payor listed in the EMR at the first visit as the payor on record and for any subsequent models. We also assessed the association between changes in payor source over the observed period and HbA1c. We categorized payors into four groups: Medicare (including Medicare Advantage and dual eligible), Medicaid, self-pay (uninsured), and private insurance. Other collected variables included HbA1c, age, sex, primary spoken language, payor, clinic location, and visit dates.
We used analysis of variance (ANOVA) to determine if there was a significant difference between unadjusted HbA1c values by categorical variables (payor, sex, language, clinic). We used t tests to assess pairwise differences in HbA1c between payor groups. We used linear regression to determine if age is correlated with HbA1c. Variables showing independent association with HbA1c were included in a general regression model of payors and HbA1c. To optimize estimation of the population parameters during the limited time window, we used all available data. We considered P<.05 to be significant.
This project was reviewed and approved by the Valleywise Health Institutional Review Board. We used STATA version 14.2 software (Stata Corp, College Station, TX) for all analyses.
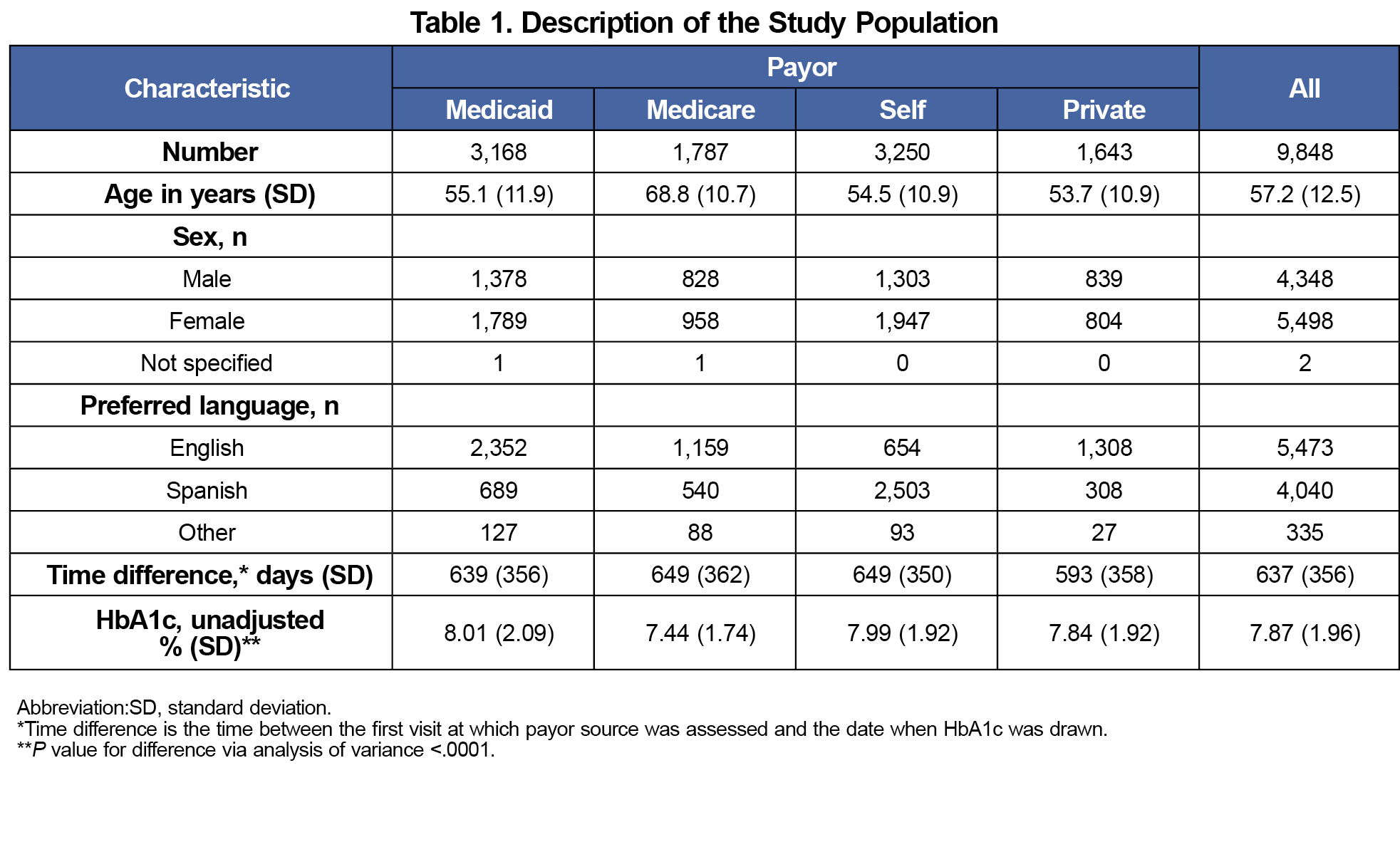
Our data includes 9,848 patients with T2D who met inclusion criteria and for whom full data are available. The population is described in Table 1.
Medicare patients had the lowest unadjusted HbA1c (7.44%), followed by privately insured (7.84%), uninsured (7.99%), and Medicaid (8.01%). Pairwise differences in HbA1c between each pair were significant at P<.05, except for the uninsured and Medicaid pair.
Greater age was associated with lower HbA1c (P<.001). Women had lower HbA1c (7.82%) than men (7.94%; P=.005). Spanish-speaking patients had the highest HbA1c (7.91%), followed by English-speakers (7.87%), and others (7.41%). Pairwise differences were significant at P<.001 between the other-speaking group and both English- and Spanish-speakers, but there was no significant difference between English- and Spanish-speaking groups (P=.42). Change in payor source during the observational period was not associated with different HbA1c (P=.25).
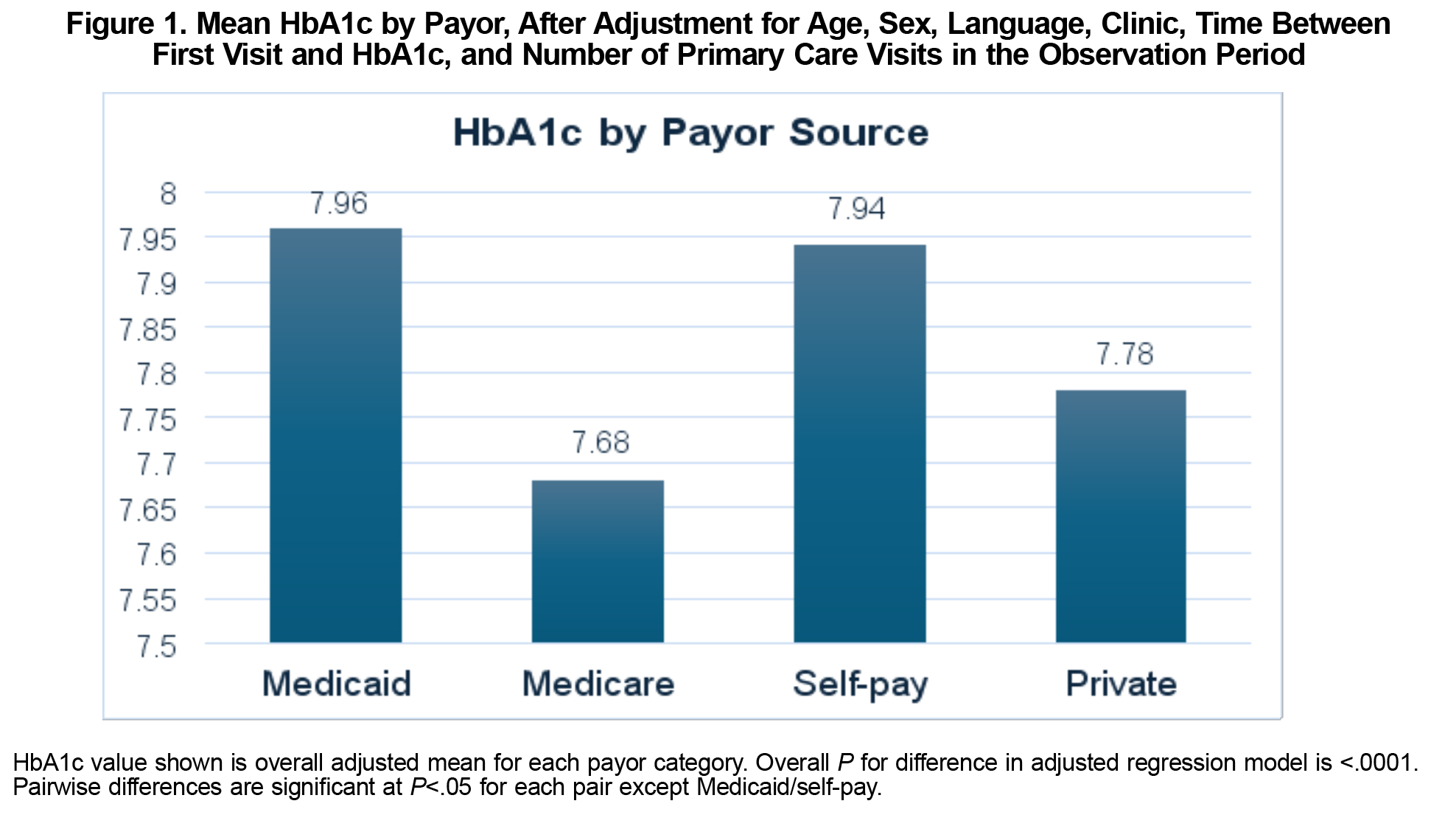
After adjusting for multiple covariates, payor source remained significantly associated with HbA1c (P<.001, F=44.12) as shown in Figure 1. Pairwise differences were significant at P<.05 for each combination of fully adjusted mean HbA1c except for Medicaid and self-pay, which were not significantly different.
In this large FQHC patient sample, followed for a mean of nearly 2 years, patients with Medicaid or no insurance prior to HbA1c assessment had higher HbA1c than those with private insurance or Medicare. Whether or not these differences are an indication of differential care by payor source is not clear, but the differences persisted after adjustment for other available variables. The higher HbA1c in the uninsured population seems intuitive as cost could limit access to care. However, higher HbA1c in Medicaid patients compared with privately insured patients is less intuitive.
While the HbA1c differences seen were statistically significant, and there appears to be no glycemic threshold below which complication risk plateaus,12 the maximum difference in adjusted means (0.28% point difference between Medicare and Medicaid groups) was short of the accepted 0.5% clinically meaningful difference.13
Age, sex, and language were independently associated with HbA1c. However, after adjustment for each of these variables, differences by payor source persisted.
In another study of adults aged 18-64 years with T2D, Hispanics had a significantly lower prevalence of health insurance coverage compared to non-Hispanic Whites and Asians.8 It was also found that members of racial and ethnic minority groups are disproportionally affected by diabetes compared with non-Hispanic Whites.14 While we did not include race or ethnicity in our analysis, our Spanish-speaking population is Hispanic to a greater degree than other language groups. Minority groups suffer a greater burden of disease, exhibit poor self-management abilities, and experience more diabetes-related complications, and thus higher rates of mortality.14, 15 Therefore, social determinants of health (SDOH) could explain some of these differences in HbA1c. Given the limited variables available to us we were unable to construct a model that fully explained the differences in HbA1c between payor groups.
Our study is limited by being an observational study of clinical data and by not including other potentially important variables (eg, medications, duration of diabetes, HbA1c prior to the last visit, income). So, while this study did not specifically measure SDOHs, this could have been done by assessing zip codes and the average income of a home in that region or having patients check-box which SDOHs they felt affected by.
The next step to address the disparity in HbA1c among patients by different payors should be a study including variables to which we did not have access (income, comorbidities, patient-provider cultural/language congruity, food insecurity, etc) to determine the most observationally explanatory factors. A model with better explanatory power, including more highly predictive variables, may inform a prospective trial aimed at reducing the HbA1c disparity.
Acknowledgments
Conflicts of Interest: The authors have no conflicts of interest to disclose.
References
- Smolen JR, Thorpe RJ Jr, Bowie JV, Gaskin DJ, LaVeist TA. Health insurance and chronic conditions in low-income urban whites. J Urban Health. 2014;91(4):637-647. doi:10.1007/s11524-014-9875-6
- Gallagher EJ, Le Roith D, Bloomgarden Z. Review of hemoglobin A(1c) in the management of diabetes. J Diabetes. 2009;1(1):9-17. doi:10.1111/j.1753-0407.2009.00009.x
- Ikeda Y, Inomata T, Fujita T, et al. Higher hemoglobin A1c levels are associated with impaired left ventricular diastolic function and higher incidence of adverse cardiac events in patients with nonischemic dilated cardiomyopathy. Heart Vessels. 2017;32(4):446-457. doi:10.1007/s00380-016-0895-x
- MacDonald MR, Petrie MC, Varyani F, et al; CHARM Investigators. Impact of diabetes on outcomes in patients with low and preserved ejection fraction heart failure: an analysis of the Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity (CHARM) programme. Eur Heart J. 2008;29(11):1377-1385. doi:10.1093/eurheartj/ehn153
- Yong PH, Weinberg L, Torkamani N, et al. The presence of diabetes and higher HbA1care independently associated with adverse outcomes after surgery. Diabetes Care. 2018;41(6):1172-1179. doi:10.2337/dc17-2304
- Škrha J, Šoupal J, Škrha J Jr, Prázný M. Glucose variability, HbA1c and microvascular complications. Rev Endocr Metab Disord. 2016;17(1):103-110. doi:10.1007/s11154-016-9347-2
- Boye KS, Thieu VT, Lage MJ, Miller H, Paczkowski R. The association between sustained HbA1c control and long-term complications among individuals with type 2 diabetes: a retrospective study. Adv Ther. 2022;39(5):2208-2221. doi:10.1007/s12325-022-02106-4
- Casagrande SS, Park J, Herman WH, Bullard KM. Health Insurance and Diabetes. 2023 Dec 20. In: Lawrence JM, Casagrande SS, Herman WH, Wexler DJ, Cefalu WT, editors. Diabetes in America. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK); 2023.
- Lee D, DeRoeck J, Ritchie ND. Reach and effectiveness of diabetes self-management education and support in a network of federally qualified health centers. J Health Care Poor Underserved. 2022;33(1):374-384. doi:10.1353/hpu.2022.0028
- Zhang JX, Huang ES, Drum ML, et al. Insurance status and quality of diabetes care in community health centers. Am J Public Health. 2009;99(4):742-747. doi:10.2105/AJPH.2007.125534
- Ali AM, Cobran EK, Young HN. Individual, interpersonal, and community factors associated with health outcomes in patients with type 2 diabetes mellitus treated at federally qualified health centers. J Diabetes Metab Disord. 2024;23(1):1071-1080. doi:10.1007/s40200-024-01388-5
- Stratton IM, Adler AI, Neil HAW, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405-412. doi:10.1136/bmj.321.7258.405
- Fokkert M, van Dijk P, Edens M, et al. Improved well-being and decreased disease burden after 1-year use of flash glucose monitoring (FLARE-NL4). BMJ Open Diabetes Res Care. 2019;7(1):e000809. doi:10.1136/bmjdrc-2019-000809
- Walker RJ, Strom Williams J, Egede LE. Influence of race, ethnicity and social determinants of health on diabetes outcomes. Am J Med Sci. 2016;351(4):366-373. doi:10.1016/j.amjms.2016.01.008
- Ding X, Kharrazi H, Nishimura A. Assessing the impact of social determinants of health on diabetes severity and management. JAMIA Open. 2024;7(4):ooae107. doi:10.1093/jamiaopen/ooae107



There are no comments for this article.