Black women are over three times more likely to die a pregnancy-related death than either White and Hispanic women and are twice as likely to experience severe morbidities during birth compared with those same populations.1 Most of these maternal deaths are preventable.2 Black infants die at twice the rate of White infants within the first year of life.3 Doulas have been shown to improve maternal and infant health outcomes.4–11 The COVID-19 pandemic changed maternal health care practices12–14 and made it harder for doulas to be present during labor.15 Few studies have explored the impact of doulas on Black births in the United States during the COVID-19 pandemic.15–21 In this study, we aimed to compare the experiences of Black mothers during the pandemic who utilized doulas with those who did not, and further, to explore differences between the physical presence of doulas versus virtual doulas and absent doulas.
LEARNER RESEARCH
Impact of Presence of Doulas on Perceived Racism for Black Mothers During the COVID-19 Pandemic
Belainesh Nigeda, DO, MPH | Kiara Patton, DO | Gisselle Pichardo, DO | Sarah E. Rubin, PhD | Sharon Casapulla, EdD, MEd, MPH
PRiMER. 2025;9:28.
Published: 6/18/2025 | DOI: 10.22454/PRiMER.2025.813796
Introduction: Few studies have explored the impact of doulas on Black births in the United States during the COVID-19 pandemic. The goal of this pilot study was to explore the birth experiences of Black mothers in the United States who used doulas and gave birth during the pandemic. More specifically, we aimed to compare the experiences of Black mothers who used doulas with those who did not; and explore differences between the physical presence of doulas, virtual doulas, and absence of doulas.
Methods: We used a cross-sectional descriptive study that utilized an electronic survey administered to participants who gave birth during the COVID-19 pandemic. Participants completed the online survey between March 2021 and August 2021.
Results: Sixty-two survey recipients participated in the study. Many of the participants—both with and without doulas—reported being afraid of enduring pregnancy-related complications (70.9%) or death due to the color of their skin (54.8%). Five of 13 participants with a doula present in the delivery room agreed that their doula decreased their experience with racism during pregnancy (P=.03). Eighty percent of participants with a doula present in the delivery room reported an improved birth experience.
Conclusion: Results of our pilot study suggest that having a doula physically present (not including virtually present) in the delivery room could make a positive difference in Black women’s birth experiences, especially with regards to racism. Our study had a small sample size and further research is needed to draw more generalizable conclusions.
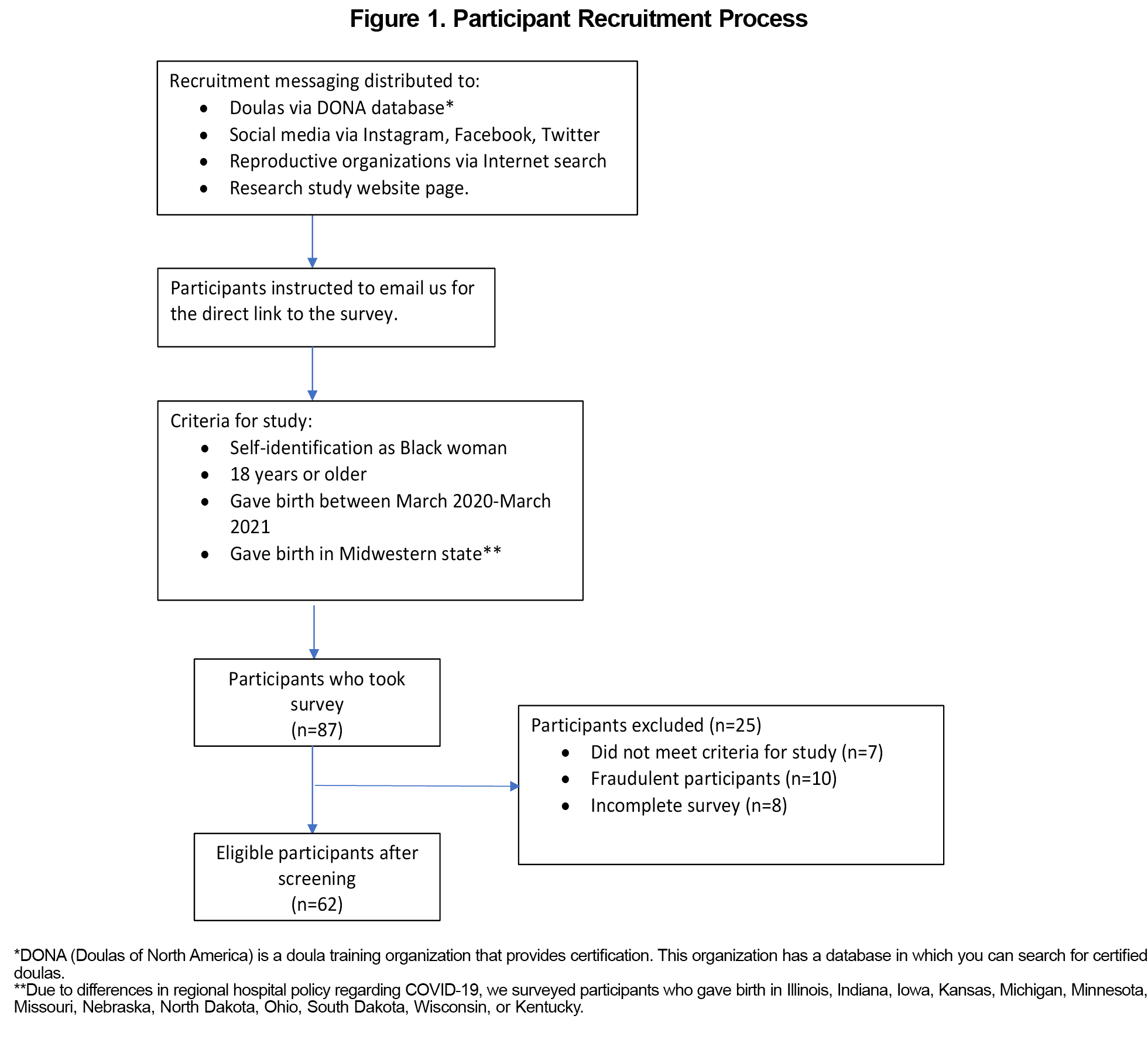
In this pilot study, we developed and distributed a 59-question survey (Appendix Table 1). The research team, which included three medical students of color and two qualitative researchers who are faculty at the medical school, drafted the initial survey items after a thorough review of the literature. A small group of the target population (Black women who had given birth) reviewed the draft survey for content and gave feedback on the wording of questions. The study was limited to people who met the screening criteria (Figure 1). Participants with doulas answered an additional 13 questions and were invited for an interview.22
We gathered survey responses from March 2021 to August 2021. Participants were entered into a drawing for a gift card. This study was funded by the Rural and Urban Scholarly Pathways Program at Ohio University Heritage College of Osteopathic Medicine. The Institutional Review Board at Ohio University approved the research protocol (IRB #20-E-458).
Data Analysis
We calculated descriptive statistics for each variable. For Likert-scale responses, "strongly agree" and "agree" were combined, as well as "strongly disagree" and "disagree," to increase sample size within response categories. As a result, the data were treated as categorical rather than ordinal, making parametric tests such as ANOVA and t tests inappropriate. To assess differences between participants who had a physically present doula versus those who did not, we used χ2 tests, as all variables analyzed were categorical. We conducted all statistical analyses using R, with significance set at P≤.05.
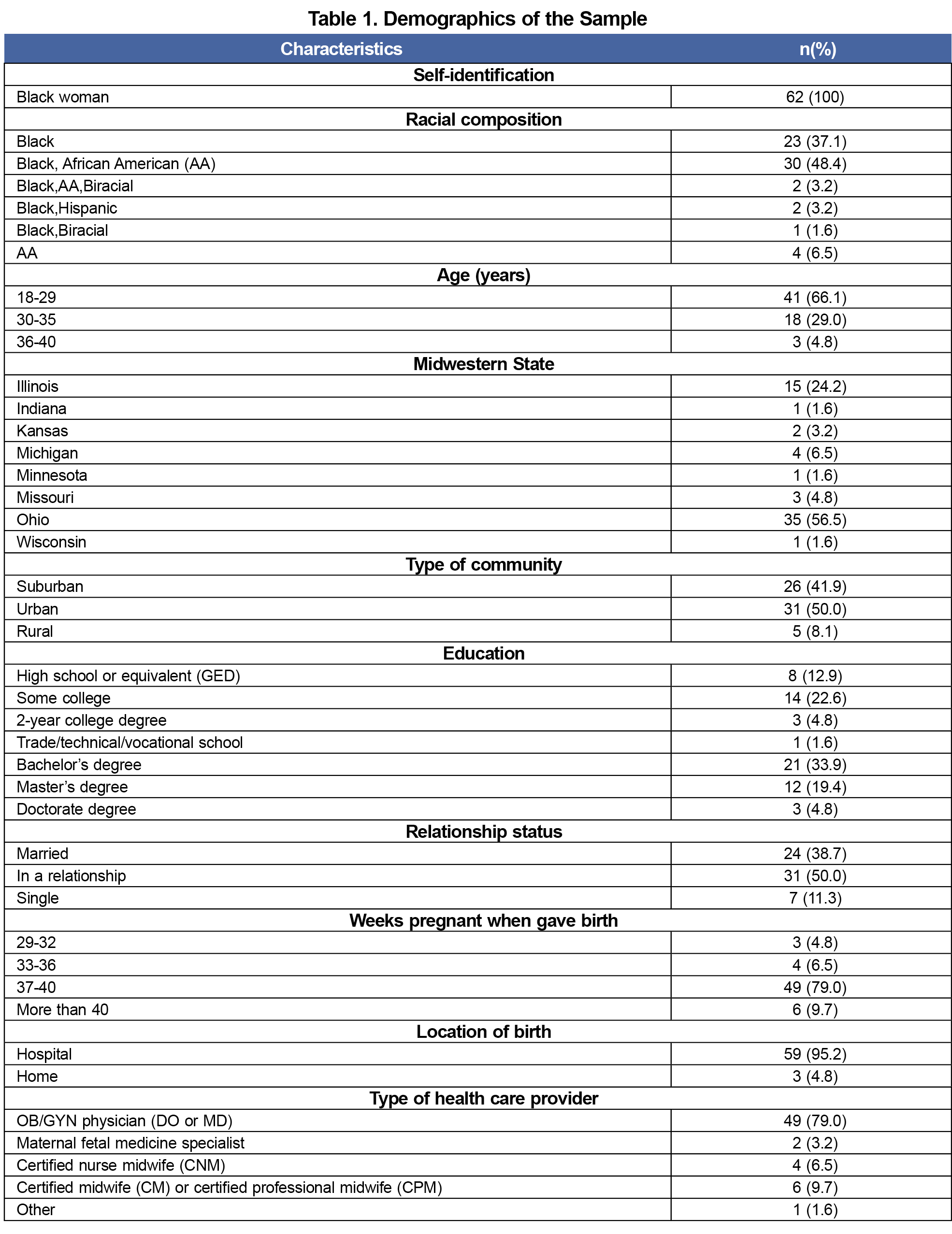
The primary analysis is descriptive in nature due to the small sample size. In total, 62 participants completed the survey (Table 1). Appendix Table 2 includes survey responses. Only 13 (21.0%) participants reported having a doula at any point during their pregnancy. Forty-four (70.9%) strongly or somewhat agreed with the statement, “I was afraid of having a complication during my pregnancy due to the color of my skin.” Thirty-four (54.9%) participants strongly or somewhat agreed, with “I was afraid of dying due to a pregnancy-related issue due to the color of my skin.” Of those who felt this item applied to them (n=27), 17 (62.9%) reported strongly or somewhat agreed with, “I believe that the discrimination I experienced during my pregnancy was due to the color of my skin.”
Of the 13 participants who reported having a doula, five (38.4%) had a doula physically present, five (38.4%) had a doula present virtually, and 3 (23.1%) were not able to have their doula present at all during birth. All five participants who had a doula physically present in the delivery room agreed with the statement, "My doula decreased my experience with racism during my pregnancy." In contrast, only one participant whose doula was either present virtually or not allowed in the room agreed with this statement (χ2=16.64, P=.03, φ=1.1 [large effect size]). Although the result is not statistically significant (P=.15), the large effect size (φ=0.72) suggests a meaningful difference that warrants further exploration with a larger sample size. Specifically, all five participants with a doula physically present in the delivery room agreed with the statement, “My doula improved my birth experience,” compared to five of the eight participants whose doula was either present virtually or not allowed in the room (χ2=6.64). There were no statistically significant differences in reported health outcomes, presence or absence of discrimination, satisfaction, and birth plan between participants who used doulas and those who did not (all P values >.05). 1
Studies have shown the positive effect of having a doula on the birth outcomes of Black women and their newborns. 8,23 The American College of Obstetricians and Gynecologists supports the evidence-based findings that all laborers can benefit from having a doula.23 Consistent with previous studies,24 doulas were underutilized in our overall sample. Our results suggest that having a doula physically present (versus virtually present) in the delivery room positively impacted the mother’s experience by reduced instances of racism during delivery. These findings are important considering the results that 71% of the participants in the study (with or without a doula) feared having a pregnancy complication due to the color of their skin. Furthermore, more than half feared dying from a pregnancy-related issue due to the color of their skin. Even participants who did not report experiencing discrimination, reported anticipatory fear or anxiety. Our results are consistent with a qualitative study of doulas working with low-income Black women that found that doulas may help mitigate the negative effects of institutional racism.20 Further research is needed to draw generalizable conclusions.
Recruitment messaging had potential to reach thousands of Black women, however, we had relatively low participant enrollment. Our study criteria were specific and narrow, which contributed to difficulty in recruitment. These limitations decrease the generalizability of the findings but offer a starting point for future studies. Additionally, due to the lack of studies surrounding Black women and doula use at the time of the study development in 2020, our survey was not validated. Although we used a literature search to guide our questions, we see this as a limitation of our study.
This study offers insight into the birth experiences of Black women who gave birth during the COVID-19 pandemic. We explored health outcomes, satisfaction, presence or absence of discrimination, and changes to birth plan due to COVID-19. The use of a doula, and particularly the physical presence of a doula in the delivery room positively impacted Black women’s birth experiences. Our descriptive analysis demonstrates the need for further research in understanding the relationship between the physical presence of doulas and improved birth experiences for Black mothers, especially with regards to racism. This study is relevant for all clinicians providing obstetric care and adds to the literature about doulas. Although obstetrics in family medicine has declined, 7% of clinicians still attend births. The need for more clinicians providing obstetric care remains.25 Currently, the United States medical curricula are lacking in education about doulas. Clinicians who plan to practice obstetrics should be aware of tools that may positively impact their patient’s birth experience.
References
- Eichelberger KY, Doll K, Ekpo GE, Zerden ML. Black Lives Matter: claiming a space for evidence-based outrage in obstetrics and Gynecology. Am J Public Health. 2016;106(10):1771-1772. doi:10.2105/AJPH.2016.303313
- Centers for Disease Control and Prevention. Deaths P-R. Data from Maternal Mortality Review Committees in 36 US States, 2017–2019. Published September 26, 2022. Accessed April 4, 2023. https://www.cdc.gov/reproductivehealth/maternal-mortality/erase-mm/data-mmrc.html
- Centers for Disease Control and Prevention. Infant Mortality. CDC. Published September 8, 2022. Accessed April 4, 2023. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/infantmortality.htm
- Vonderheid SC, Kishi R, Norr KF, Klima C. Group Prenatal Care and Doula Care for Pregnant Women. In: Handler A, Kennelly J, Peacock N, eds. Reducing Racial/Ethnic Disparities in Reproductive and Perinatal Outcomes: The Evidence from Population-Based Interventions.Springer US; 2011:369-399, doi:10.1007/978-1-4419-1499-6_15.
- Bohren MA, Hofmeyr GJ, Sakala C, Fukuzawa RK, Cuthbert A. Continuous support for women during childbirth. Cochrane Database Syst Rev. 2017;7(7):CD003766. doi:10.1002/14651858.CD003766.pub6
- Klaus M, Klaus P. Academy of breastfeeding medicine founder’s lecture 2009: maternity care re-evaluated. Breastfeed Med. 2010;5(1):3-8. doi:10.1089/bfm.2009.0086
- Kozhimannil KB, Hardeman RR, Alarid-Escudero F, Vogelsang CA, Blauer-Peterson C, Howell EA. Modeling the cost-effectiveness of doula care associated with reductions in preterm birth and cesarean delivery. Birth. 2016;43(1):20-27. doi:10.1111/birt.12218
- Gruber KJ, Cupito SH, Dobson CF. Impact of doulas on healthy birth outcomes. J Perinat Educ. 2013;22(1):49-58. doi:10.1891/1058-1243.22.1.49
- Cattelona G, Friesen CA, Hormuth LJ. the impact of a volunteer postpartum doula program on breastfeeding success: a case study. J Hum Lact. 2015;31(4):607-610. doi:10.1177/0890334415583302
- Edwards RC, Thullen MJ, Korfmacher J, Lantos JD, Henson LG, Hans SL. Breastfeeding and complementary food: randomized trial of community doula home visiting. Pediatrics. 2013;132(suppl 2):S160-S166. doi:10.1542/peds.2013-1021P
- Thullen MJ, McMillin SE, Korfmacher J, et al. Father participation in a community-doula home-visiting intervention with young, African American mothers. Infant Ment Health J. 2014;35(5):422-434. doi:10.1002/imhj.21463
- Combellick JL, Basile Ibrahim B, Julien T, Scharer K, Jackson K, Powell Kennedy H. Birth during the COVID-19 pandemic: what childbearing people in the United States needed to achieve a positive birth experience. Birth. 2022;49(2):341-351. doi:10.1111/birt.12616
- Liu CH, Koire A, Erdei C, Mittal L. Unexpected changes in birth experiences during the COVID-19 pandemic: implications for maternal mental health. Arch Gynecol Obstet. 2022;306(3):687-697. doi:10.1007/s00404-021-06310-5
- DeYoung SE, Mangum M. Pregnancy, birthing, and postpartum experiences during COVID-19 in the United States. Front Sociol. 2021;6:611212. Accessed April 4, 2023. https://www.frontiersin.org/articles/10.3389/fsoc.2021.611212doi:10.3389/fsoc.2021.611212
- Castañeda AN, Searcy JJ. Shifting landscapes of belonging: birth doulas and COVID-19. Pract Anthropol. 2020;42(4):5-10. doi:10.17730/0888-4552.42.4.5
- Adams C. Pregnancy and birth in the United States during the COVID-19 pandemic: the views of doulas. Birth. 2022;49(1):116-122. doi:10.1111/birt.12580
- Carvalho K, Kheyfets A, Lawrence B, et al. Examining the role of psychosocial influences on Black maternal health during the COVID-19 pandemic. Matern Child Health J. 2022;26(4):764-769. doi:10.1007/s10995-021-03181-9
- Nguyen TC, Donovan EE, Wright ML. Doula support challenges and coping strategies during the COVID-19 pandemic: implications for maternal health inequities. Health Commun. 2022;37(12):1496-1502. doi:10.1080/10410236.2021.2012898
- Rivera M. Transitions in black and latinx community-based doula work in the US during COVID-19. Front Sociol. 2021;6:611350. doi:10.3389/fsoc.2021.611350
- Wint K, Elias TI, Mendez G, Mendez DD, Gary-Webb TL. Experiences of community doulas working with low-income, African American mothers. Health Equity. 2019;3(1):109-116. doi:10.1089/heq.2018.0045
- Wheeler JM, Misra DP, Giurgescu C. Stress and coping among pregnant black women during the COVID-19 pandemic. Public Health Nurs. 2021;38(4):596-602. doi:10.1111/phn.12909
- Casapulla S, Rubin S, Nigeda B, Pichardo G, Patton K. “Because Doulas Save Black Women’s Lives”: Black Women’s Strategic Use of Doulas in Anticipation and Experiences of Obstetric Racism. Women’s Reproductive Health. 2025. [Published online: 09 May 2025] 1–21. doi: 10.1080/23293691.2025.2486384
- ACOG Committee Opinion No. ACOG Committee Opinion No. 766: Approaches to Limit Intervention During Labor and Birth. Obstet Gynecol. 2019;133(2):e164-e173. doi:10.1097/AOG.0000000000003074
- Kozhimannil KB, Attanasio LB, Jou J, Joarnt LK, Johnson PJ, Gjerdingen DK. Potential benefits of increased access to doula support during childbirth. Am J Manag Care. 2014;20(8):e340-e352.
- Barreto TW, Eden AR, Petterson S, Bazemore AW, Peterson LE. Intention versus reality: family medicine residency graduates’ intention to practice obstetrics. J Am Board Fam Med. 2017;30(4):405-406. PMID:28720622 doi:10.3122/jabfm.2017.04.170120
Lead Author
Belainesh Nigeda, DO, MPH
Affiliations: Ohio University Heritage College of Osteopathic Medicine, Athens, OH
Co-Authors
Kiara Patton, DO - Ohio University Heritage College of Osteopathic Medicine, Athens, OH
Gisselle Pichardo, DO - Ohio University Heritage College of Osteopathic Medicine, Athens, OH
Sarah E. Rubin, PhD - Department of Social Medicine, Ohio University Heritage College of Osteopathic Medicine, Athens, OH
Sharon Casapulla, EdD, MEd, MPH - Department of Primary Care, Ohio University Heritage College of Osteopathic Medicine, Athens, OH | Office of Rural and Underserved Programs, Ohio University Heritage College of Osteopathic Medicine, Athens, OH
Corresponding Author
Sharon Casapulla, EdD, MEd, MPH
Correspondence: Department of Primary Care, Ohio University Heritage College of Osteopathic Medicine, Athens, OH
Email: casapull@ohio.edu
Fetching other articles... 
Loading the comment form... 
Submitting your comment... 


There are no comments for this article.