Quality improvement collaboratives (QICs) are increasingly used in graduate medical education to enhance clinical outcomes and meet educational objectives. While they offer potential benefits, such as driving systemic change and developing best practices, multi-institutional QI efforts face unique challenges, and no consolidated guidance exists to help faculty navigate them. Drawing on literature and personal experience, we outline six steps to help educators overcome hurdles associated with launching a QIC: (1) choose a goal aligned with organizational priorities; (2) recruit a multidisciplinary team; (3) craft a clear and generalizable aim statement; (4) select preexisting, nationally-recognized metrics; (5) navigate institutional review board requirements; and (6) plan meetings around key milestones. These steps will help medical educators anticipate common hurdles, secure administrative support, and foster effective collaboration across institutions. Personal illustrations accompany each step. By following this framework, educators can more confidently lead QICs to engage learners and improve patient care.
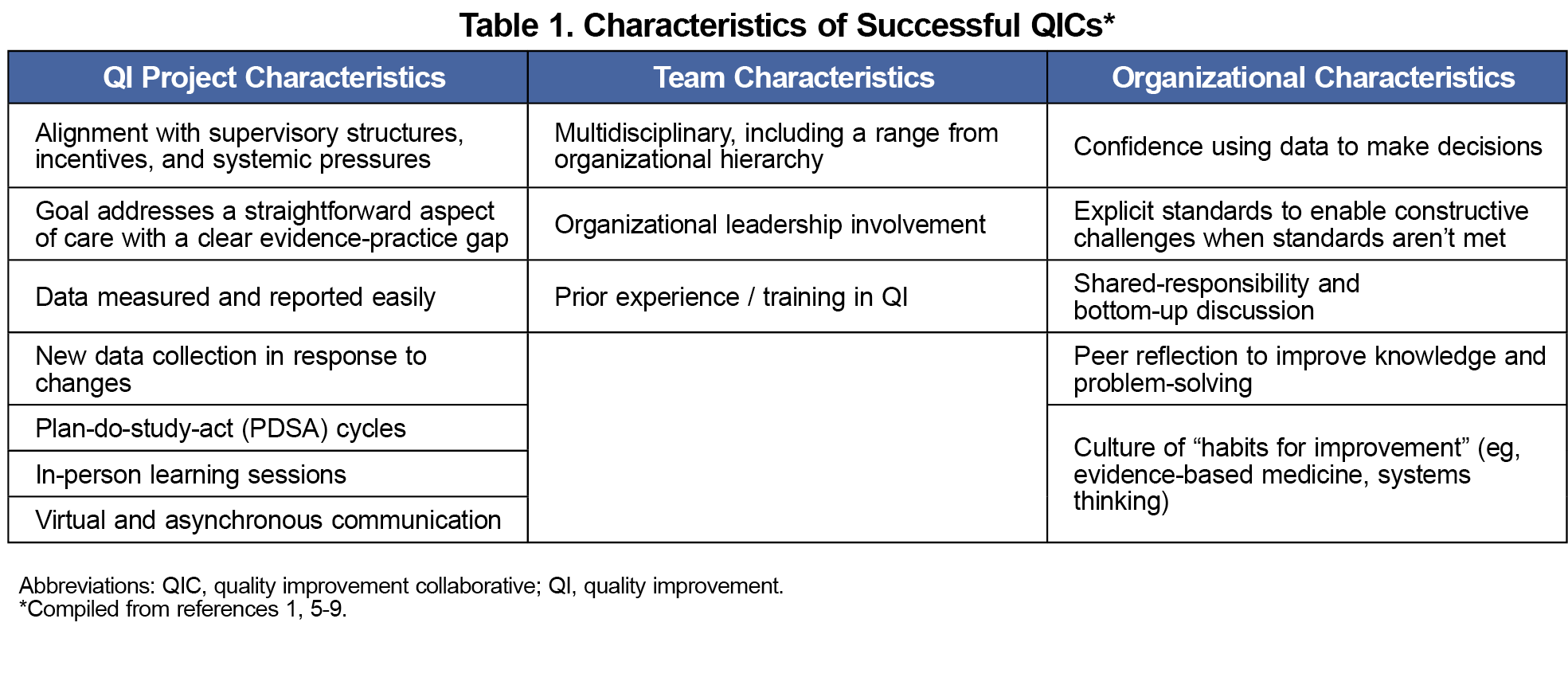
Learning collaboratives benefit multiple clinical and educational aims, including quality improvement (QI).1 In fact, the Accreditation Council for Graduate Medical Education’s requirements for family medicine specifically promote quality improvement collaboratives (QICs) to “enhance population care across regions by sharing best practices to deliver high-quality patient care.”2 QIC benefits include learning from different practice styles, encouragement to overcome systemic resistance to change, development of generalizable procedures, and dissemination of practice-changing discoveries.3,4 While others have described characteristics of successful QICs1,5-9 (Table 1) and QI curriculum,8,10,11 there are no existing guides to help new collaboratives avoid pitfalls unique to beginning a QIC.
From 2022 to 2023, we participated in a QIC through a faculty development fellowship. Our collaborative included family medicine departments from seven academic institutions affiliated with community or tertiary hospital systems. We encountered hurdles to collaborative QI, for which we found little guidance. We address these hurdles in the six steps outlined in this article, which are based on literature12 and personal experience. They assume familiarity with QI principles13-15 and the Model for Improvement.13,16 We hope this framework helps educators better train learners and improve patient care.
Step 1: Choose a Goal That Aligns With Organizational Initiatives.
The most important decision facing a QIC is its goal.7 While single-institution QI may address smaller-scale problems such as patients’ wait time at a specific clinic, successful QICs should choose goals that align with organizational initiatives.5 Without alignment, QICs risk losing crucial administrative support.10,11 While organizational initiatives are not always glamorous, they are usually rooted in evidence and tied to financial or recognition incentives.5,10 A 2018 systematic review of QIC effectiveness concluded, “Collaboratives reporting success generally addressed relatively straightforward aspects of care, had a strong evidence base, and noted a clear evidence-practice gap in an accepted clinical pathway or guideline.”1
While QICs might be tempted to improve an area of personal or emerging interest, consider the following example. Our goal was to improve rates of lung cancer screening. Screening is undeniably important, but it was not an organizational goal at our institutions. Furthermore, the screening guideline is difficult to apply due to the need to calculate pack-years and time since one quit smoking.17 Our success was therefore hampered from the outset by organizational backing and a complicated clinical pathway. We should have considered a shared organizational initiative, perhaps from a Healthcare Effectiveness Data and Information Set (HEDIS) measure.
Step 2: Recruit a Multidisciplinary Team.
To launch a collaborative, people must first discover that they share a common goal.18 State meetings and virtual networks, such as STFM Connect,19 are suitable meeting spaces. Once representatives from various institutions commit to a collaborative, it is time to form local teams. Successful teams include members from various backgrounds.5,6,9 At a minimum, recruit the following (one person can serve multiple roles).14
- Team lead: oversees all aspects of the QI project; guides the team to key personnel and systems
- Technical expert: has a detailed understanding of systems (eg, a QIC planning to use the electronic medical record [EMR] should include someone from information technology).
- Systems leader: possesses the authority to implement change; foresees the impact of changes on seemingly unrelated systems (eg, the medical director of an ambulatory clinic)
- Improvement advisor: is trained in QI; advises the team and helps interpret data.
- Executive sponsor: secures resources and removes barriers (eg, medical director, department chair).
An experienced member of our collaborative served as both team lead and a common improvement advisor. Institutional representatives served as local team leads and systems leaders, since most held leadership roles (eg, medical director). Each local team included a technical expert. For most, this was a technology expert who built reports to identify smokers who had completed lung cancer screening. Lastly, department chairs or program directors served as executive sponsors.
Step 3: Craft a Clear Aim Statement That Allows for Local Variation.
The aim statement defines success and, second only to the goal, directs the team’s improvement efforts. An effective aim statement promotes clear objectives by being SMARTIE (Specific, Measurable, Achievable, Relevant, Time-bound, Inclusive, and Equitable).20 Since the aim applies to multiple organizations, it should allow for local variation in patients and processes.
Our collaborative chose to “increase lung cancer screening rates among eligible, current smokers by 25% within one year.” This aim statement allowed for local variation by classifying the goal in relative, not absolute, terms. It also clearly defined the target population (current smokers). Former smokers also qualify for screening, but identifying them is complicated due to EMR inaccuracy.21 By starting the improvement initiative with current smokers, our QIC made progress toward its goal without having to consider variations in our diverse EMRs.
Step 4: Select Preexisting, Nationally-Recognized Metrics.
We strongly encourage QICs to use pre-existing, nationally recognized metrics, since institutions cannot collaborate without common measures of success. HEDIS measures are an example. Successful QICs report data regularly,5,6 so the collaborative should choose metrics that can be sampled easily and iteratively. A good metric can also be improved within the project’s expected timeline.8 Consider outcome, process, structure, and/or balancing metrics, to gauge initiatives’ success and to explore unforeseen effects.22,23
If a common metric does not exist, the QIC must develop a new one, which could be an arduous process. Considering our example, only one of our institutions tracked lung cancer screening. Most of our members therefore had to collect data through manual queries done by busy technology experts.
Step 5: Navigate the Institutional Review Board (IRB).
QI projects are generally exempt from IRB oversight, since they do not involve research or human subjects activity.24,25 However, QICs might not be exempt, because they may share identifiable data and disseminate results,26 which fall under the purview of the IRB. IRB representatives and experienced colleagues provide excellent guidance through local board procedures.27 Our members consulted both to streamline approval, though we had vastly different experiences. Some members secured approval in a matter of weeks, while others had to engage executive sponsors.
Be sure to engage the IRB early in the project with specific details about what data is being collected, whether data will be de-identified, how interventions will affect patient care and local systems, and whether the collaborative’s findings will be disseminated. We chose to analyze our data locally, which lessened IRB concerns about data sharing, since shared data was aggregated and de-identified. Use a data use agreement if sharing identifiable data between institutions.
Step 6: Plan Meetings to Coincide With Important Milestones.
Team communication is critical for success,28 and geographic separation makes communication more difficult. Our QIC spanned the continental United States, meaning we had to communicate across multiple time zones. This required thoughtful use of in-person, virtual, and asynchronous communication.6
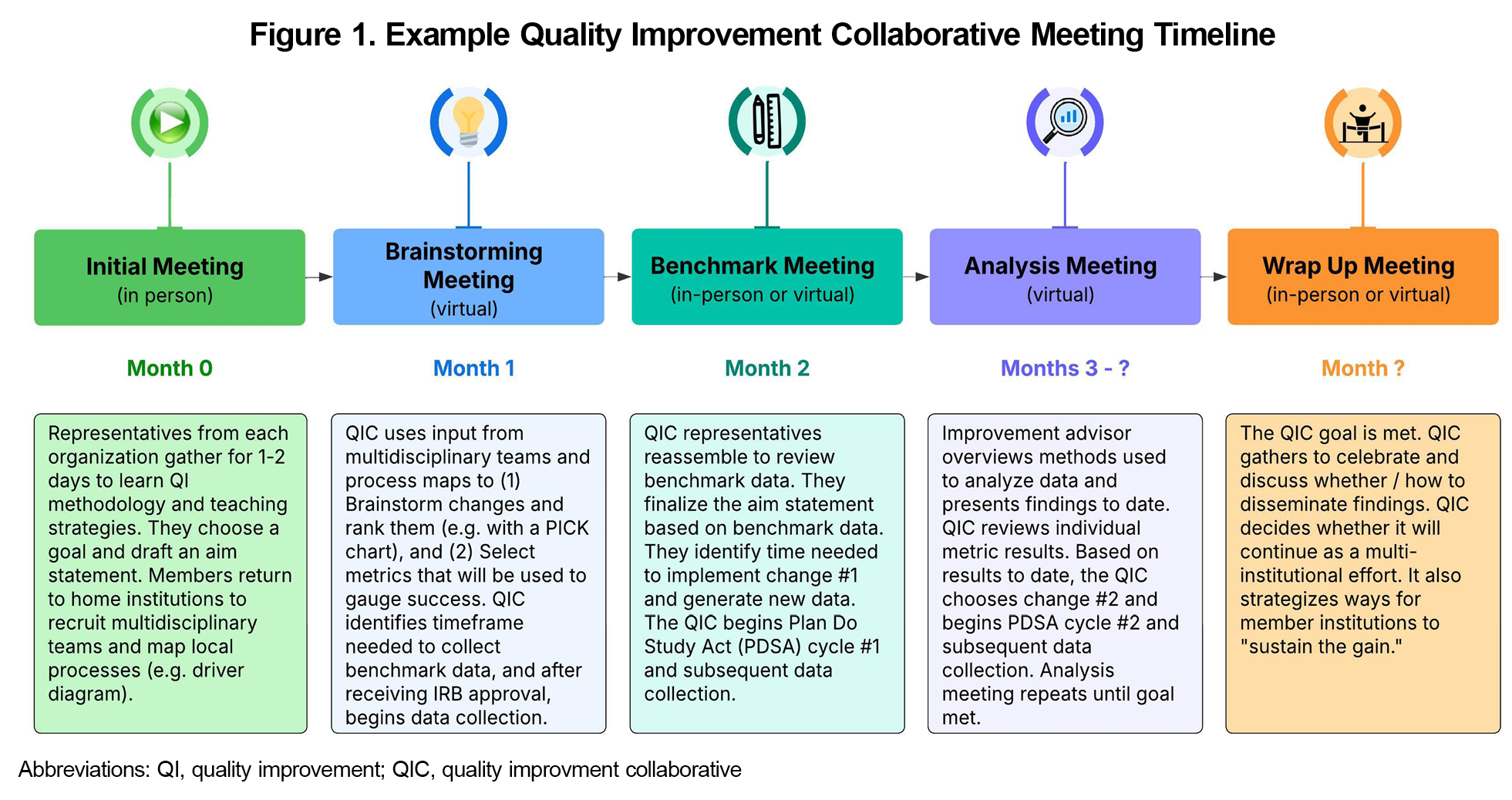
At the outset, the collaborative should define its expectations for communication and the frequency with which it will meet for various project milestones. The Institute for Healthcare Improvement recommends a mixture of “learning sessions” and “action periods.”7 Learning sessions provide the team with the knowledge and skills to carry out improvement activities, whereas action periods provide time to implement change and gather data. Based on our experience, we propose a loose framework for meetings in Figure 1.
At the beginning of the project, the QIC should plan to meet frequently for education and to address unexpected challenges. During the implementation portion of the project, the frequency of data collection will likely dictate how often the QIC meets. Lastly but importantly, QIC members should secure protected time from executive sponsors to participate in the QI endeavor.10,11
Quality improvement collaboratives offer substantial benefits to institutions and patients, but multi-institutional efforts come with unique challenges. The steps outlined here will help medical educators anticipate hurdles, guide learners, and ultimately launch QICs to enhance patient care.
Acknowledgments
The authors would like to acknowledge Carrie Gray, DO; Christina Lincoln, DO; Nailah Adams Morancie, MD; Signe O’Neale, MD; and Dawn Morriston, MPH for their partnership in the quality improvement collaborative.
Conflicts of Interest: The authors have no conflicts of interest to disclose.
Prior Presentations: This content was presented in a different form at the Society of Teachers of Family Medicine Conference on Practice & Quality Improvement, Denver, Colorado, September 16, 2024.
Funding Statement: The authors are indebted to their institutions, which provided leave and/or funding for them to attend the 2022-2023 UNC Faculty Development Fellowship.
References
- 1. Wells S, Tamir O, Gray J, Naidoo D, Bekhit M, Goldmann D. Are quality improvement collaboratives effective? A systematic review. BMJ Qual Saf. 2018;27(3):226-240. doi:10.1136/bmjqs-2017-006926.
- ACGME Program Requirements for Graduate Medical Education in Family Medicine. Accreditation Council for Graduate Medical Education. Accessed August 28, 2025. https://www.acgme.org/globalassets/pfassets/programrequirements/120_familymedicine_2023.pdf
- Plsek PE. Quality improvement methods in clinical medicine. Pediatrics. 1999;103(1)(suppl E):203-214. In eng. doi:10.1542/peds.103.SE1.203
- 4. Shaw EK, Chase SM, Howard J, Nutting PA, Crabtree BF. More black box to explore: how quality improvement collaboratives shape practice change. J Am Board Fam Med 2012;25(2):149-57. doi:10.3122/jabfm.2012.02.110090.
- 5. Zamboni K, Baker U, Tyagi M, Schellenberg J, Hill Z, Hanson C. How and under what circumstances do quality improvement collaboratives lead to better outcomes? A systematic review. Implement Sci. 2020;15(1):27. doi:10.1186/s13012-020-0978-z.
- 6. Nadeem E, Olin SS, Hill LC, Hoagwood KE, Horwitz SM. Understanding the components of quality improvement collaboratives: a systematic literature review. Milbank Q 2013;91(2):354-94. doi:10.1111/milq.12016.
- The Breakthrough Series. IHI's Collaborative Model for Achieving Breakthrough Improvement. IHI Innovation Series White Paper. Institute for Healthcare Improvement. Published 2003. Accessed August 28, 2025. https://www.ihi.org/sites/default/files/2023-09/IHIBreakthroughSerieswhitepaper2003.pdf
- Horstman MJ, Tomolo AM, Webb B, Vaclavik L. Selecting a quality improvement project: 5 questions for trainees and mentors. J Grad Med Educ. 2023;15(5):528-531. doi:10.4300/JGME-D-23-00249.1
- Schouten LM, Grol RP, Hulscher ME. Factors influencing success in quality-improvement collaboratives: development and psychometric testing of an instrument. Implement Sci 2010;5:84. (In eng). doi:10.1186/1748-5908-5-84.
- Brown A, Lafreniere K, Freedman D, et al. A realist synthesis of quality improvement curricula in undergraduate and postgraduate medical education: what works, for whom, and in what contexts? BMJ Qual Saf. 2021;30(4):337-352. doi:10.1136/bmjqs-2020-010887.
- Jones AC, Shipman SA, Ogrinc G. Key characteristics of successful quality improvement curricula in physician education: a realist review. BMJ Qual Saf 2015;24(1):77-88. doi:10.1136/bmjqs-2014-002846.
- Wong BM, Levinson W, Shojania KG. Quality improvement in medical education: current state and future directions. Med Educ 2012;46(1):107-19. doi:10.1111/j.1365-2923.2011.04154.x.
- Crowl A, Sharma A, Sorge L, Sorensen T. Accelerating quality improvement within your organization: applying the Model for Improvement. J Am Pharm Assoc (2003) 2015;55(4):e364-74; quiz e375-6. doi:10.1331/JAPhA.2015.15533.
- Silver SA, Harel Z, McQuillan R, et al. How to begin a quality improvement project. Clin J Am Soc Nephrol. 2016;11(5):893-900. doi:10.2215/CJN.11491015
- Cleghorn GD, Headrick LA. The PDSA cycle at the core of learning in health professions education. Jt Comm J Qual Improv. 1996;22(3):206-12. doi:10.1016/S1070-3241(16)30223-1
- The Model for Improvement. (Part 1). Institute for Healthcare Improvement. Published 2024. Accessed August 25, 2025. https://www.ihi.org/education/IHIOpenSchool/resources/Pages/AudioandVideo/Whiteboard3.aspx
- Carter-Harris L, Gould MK. Multilevel barriers to the successful implementation of lung cancer screening: why does it have to be so hard? Ann Am Thorac Soc. 2017;14(8):1261-1265. doi:10.1513/AnnalsATS.201703-204PS.
- Gillner S, Wild EM. How social networks influence the local implementation of initiatives developed in quality improvement collaboratives in health care: A qualitative process study. Health Care Manage Rev. 2024;49(2):148-157. doi:10.1097/HMR.0000000000000400
- STFM Connect Member Forum. Society of Teachers of Family Medicine. Accessed August 28, 2025. https://connect.stfm.org/home
- Creating SMARTIE Goals & Objectives Worksheet. National Council for Mental Wellbeing. Published September 14, 2021. Accessed August 28, 2025. https://www.thenationalcouncil.org/resources/creating-smartie-goals-objectives-worksheet/
- Kukhareva PV, Caverly TJ, Li H, et al. Inaccuracies in electronic health records smoking data and a potential approach to address resulting underestimation in determining lung cancer screening eligibility. J Am Med Inform Assoc. 2022;29(5):779-788. doi:10.1093/jamia/ocac020.
- Jazieh AR. Quality measures: types, selection, and application in health care quality improvement projects. Glob J Qual Saf Healthc. 2020;3(4):144-146. doi:10.36401/JQSH-20-X6
- Quality, Service Improvement and Redesign Tools: A model for measuring quality care. ACT Academy. Accessed August 29, 2025. https://www.med.unc.edu/ihqi/wp-content/uploads/sites/463/2021/01/A-Model-for-Measuring-Quality-Care-NHS-Improvement-brief.pdf
- Quality Improvement Activities FAQs. U.S. Department of Health and Human Services. Accessed August 29, 2025. https://www.hhs.gov/ohrp/regulations-and-policy/guidance/faq/quality-improvement-activities/index.html
- Code of Federal Regulations Title 45 Public Welfare, Part 46 Protection of Human Subjects. Department of Health and Human Services. January 15, 2009. Accessed August 29, 2025. https://www.hhs.gov/ohrp/sites/default/files/ohrp/policy/ohrpregulations.pdf
- Faiman B. Quality improvement projects and clinical research studies. J Adv Pract Oncol. 2021;12(4):360-361. doi:10.6004/jadpro.2021.12.4.1.
- Polito CC, Cribbs SK, Martin GS, et al. Navigating the institutional review board approval process in a multicenter observational critical care study. Crit Care Med. 2014;42(5):1105-9. doi:10.1097/CCM.0000000000000133
- Reinertsen J, Gosfield A, Rupp W, Whittington J. Engaging physicians in a shared quality agenda. IHI Innovation Series White Paper. Institute for Healthcare Improvement. Published 2007. Accessed August 29, 2025. https://www.reinertsengroup.com/publications/documents/IHIEngagingPhysiciansWhitePaper2007.pdf



There are no comments for this article.