Introduction: Hepatitis C virus (HCV) remains a public health concern in the United States. We developed a quality improvement project to address persistent challenges to HCV treatment at one primary care clinic. Challenges addressed included barriers to accessing specialist care to receive antiviral treatment and lack of patient resources, education, and awareness. Recognizing the potential for primary care providers to bridge treatment gaps, our initiative at an urban family medicine residency clinic in a large Midwest city targeted a patient population diagnosed with HCV but who remained untreated.
Methods: Searching the medical record, we identified 40 eligible patients who had not received treatment despite a positive HCV diagnosis. Enrolled participants were asked to report their awareness, perceived barriers, and willingness to receive treatment in a primary care setting via a phone-assisted survey.
Results: A total of 16 patients completed the survey (response rate 40%). Eighty-two percent were aware of their diagnosis, and 68.8% had not completed treatment. Only seven (43.8%) understood what an HCV infection is, while eight (50.0%) were aware that untreated HCV can lead to liver damage and cancer. Six (37.5%) claimed not to understand what an HCV infection is, and five reported that a medical professional had never explained it to them. Most respondents (81.2%) expressed a desire to initiate a treatment regimen and preferred to receive treatment at their primary care clinic.
Conclusion: In an urban primary care residency clinic, HCV treatment is both possible and desired by patients.
Since 2011, the treatment of hepatitis C virus (HCV) has become much more effective and side effects have been reduced.1 However, HCV continues to be a major public health concern in the United States, where only one-third of affected individuals with insurance receive timely treatment, with even lower rates for patients with Medicaid.2 Barriers to treatment for patients diagnosed with HCV include specialist availability, treatment eligibility requirements, patient awareness of diagnosis and disease burden, and stigmatization.3
The Centers for Disease Control and Prevention (CDC) recommends reducing barriers to HCV treatment by increasing the number of providers in primary care treating HCV, providing treatment in as few visits as possible, and removing eligibility restrictions for treatment.2 Treatment of HCV in primary care with providers trained in HCV management is as effective as treatment by a specialist.4
The Bethesda Clinic is an outpatient family medicine residency clinic that serves a diverse population of lower income patients. A number of patients in the clinic were noted to have untreated HCV. The goal of this quality improvement project was to identify untreated patients with HCV in our clinic and explore their barriers to treatment to better understand how to increase treatment among our patient population.
This project was considered “not human research” by University of Minnesota Institutional Review Board (STUDY00021019). Support staff created a data set using electronic medical records (EMR) data by searching for patients with the following inclusion criteria: (1) hepatitis C listed on their problem list, (2) previously tested positive for hepatitis C antibody, or (3) had a positive HCV RNA quantification result without a subsequent negative viral load result. One of the authors, a medical student, conducted a chart review of this list of 590 patients, identifying 40 who had both documented HCV infection and no evidence of completed treatment.
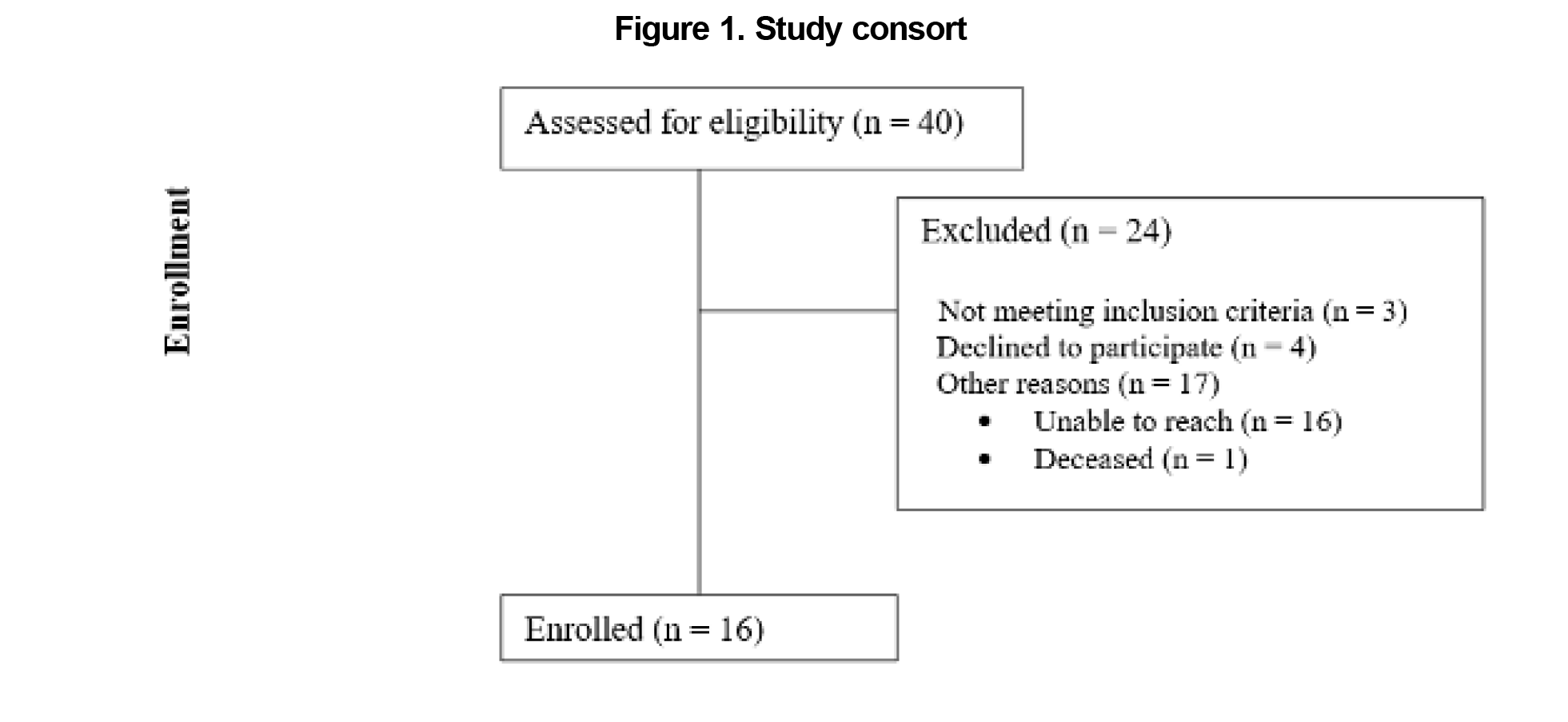
In February 2024, the same author attempted to contact each patient to inform them of their diagnosis, complete a phone-assisted survey, and schedule an appointment at Bethesda clinic. Each attempted contact was documented within the patient’s chart. Four patients declined the survey and 16 patients were not reachable (Figure 1). For patients unable to be contacted after three attempts, a registered letter was sent to their home address informing them of their diagnosis with instructions to schedule an appointment.
Bethesda clinicians developed the survey and included multiple-choice questions about patients’ awareness of diagnosis, previous treatment, barriers to treatment, and whether treatment at their primary care clinic would reduce these barriers (see Appendix A). Individuals who were eligible for treatment by a primary care provider (ie, not pregnant, without cirrhosis, no previous failed treatment) were scheduled at the end of the survey for an intake visit for HCV treatment at our clinic. Referrals to hepatology were made for those not meeting criteria for primary care treatment.
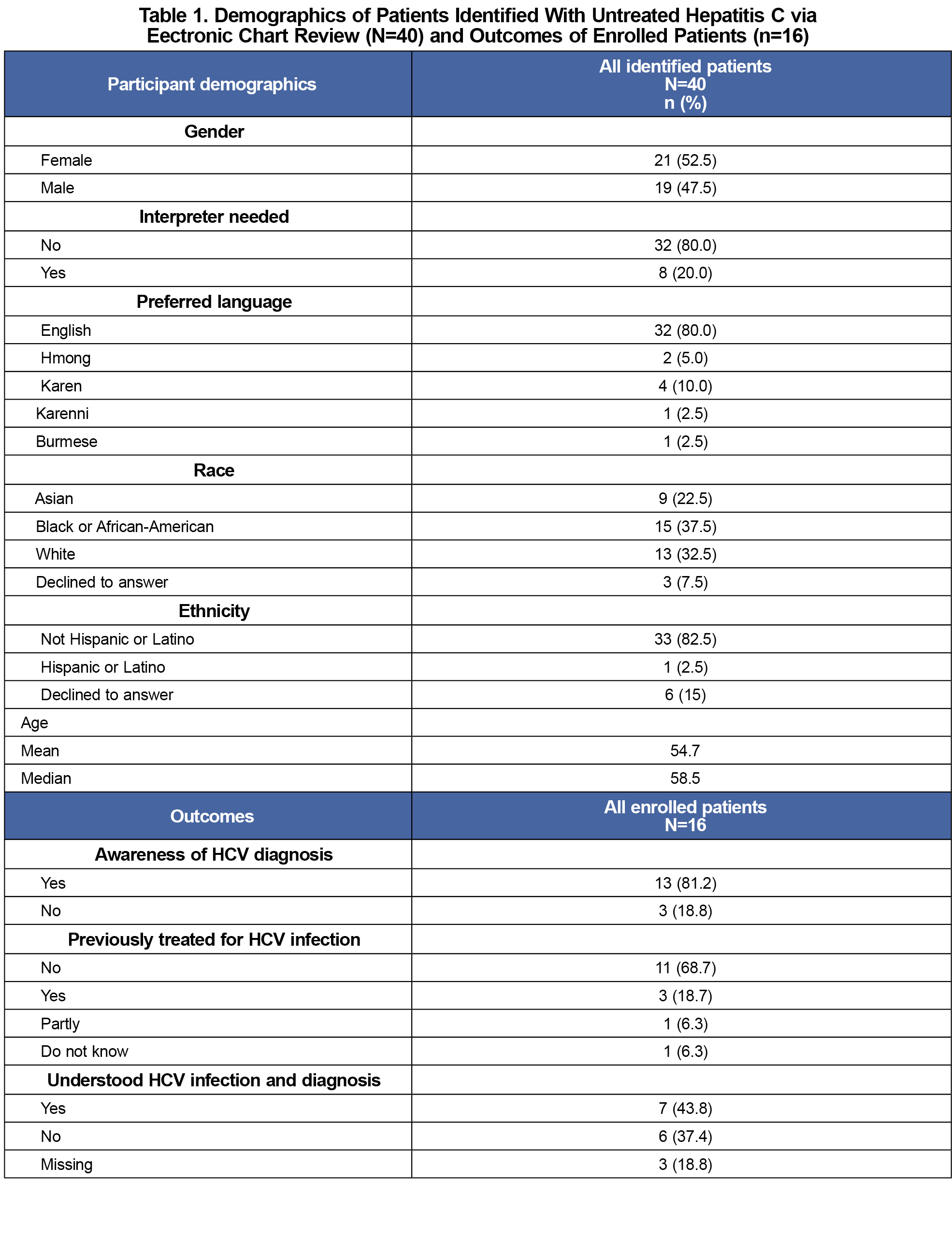
Our team collected demographic data for factors such as gender, preferred language, and race/ethnicity from patients’ EMRs. We calculated descriptive frequencies for demographic characteristics and for patients’ awareness of HCV diagnosis, previous treatment, and their understanding of HCV infection and diagnosis.
We identified forty patients with chronic HCV and no documentation of treatment (Figure 1). Of these patients most did not need an interpreter (n=32, 80.0%), spoke English (n=32, 80.0%), and were not Hispanic or Latino (n=33, 82.5%). Of the 40 patients, 37.5% identified as Black or African-American, 32.5% as White, and 22.5% as Southeast Asian (Table 1). Of the forty patients contacted, 16 responded and completed the survey, resulting in a response rate of 40.0%. Among all respondents, most were aware of their HCV diagnosis (n=13, 81.2%) and had not completed treatment (n=11, 68.8%). Only seven (43.8%) stated that they understood what an HCV infection is and eight (50%) were aware that untreated disease can lead to liver damage and cancer (Table 1). Six (37.4%) did not understand what an HCV infection is and, of those, five reported that a medical professional had never explained it to them.
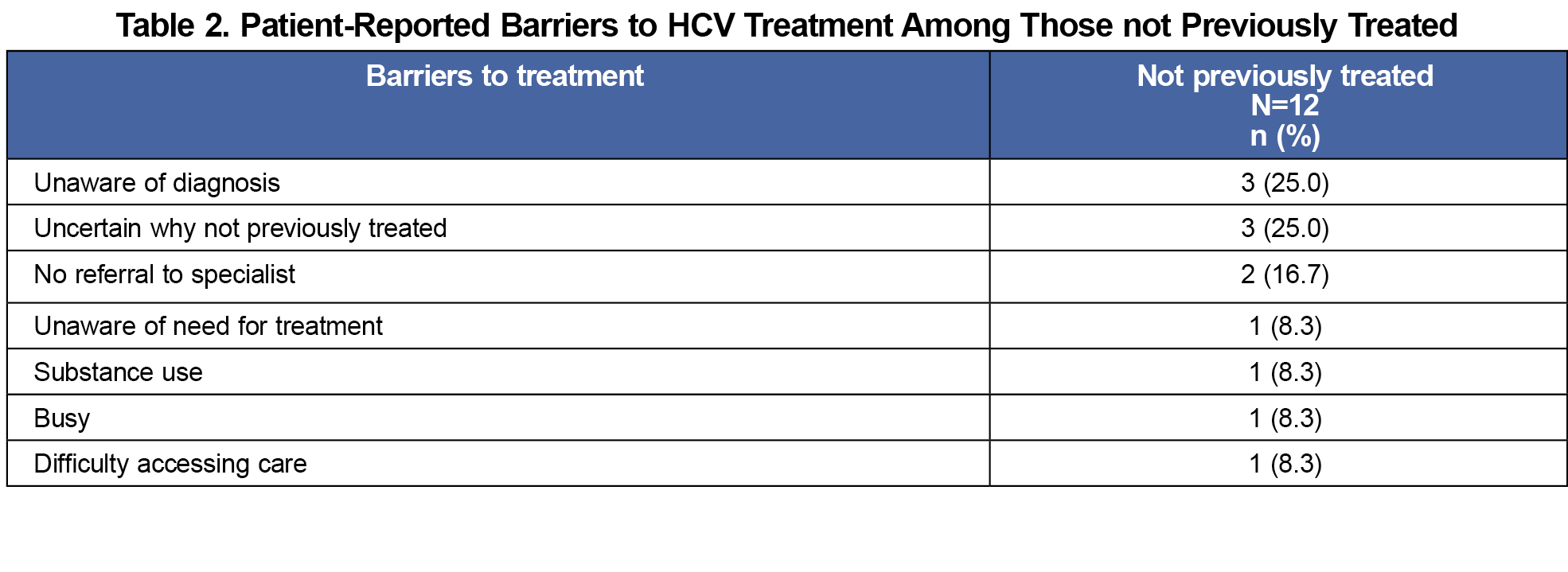
Participants identified three main reasons for not receiving treatment previously: (1) not being aware of their diagnosis (n=3, 25%), (2)not being informed or uncertain about the reason for lack of treatment (n=3, 25%), and never receiving a referral (n=2, 16.7%; Table 2). Most respondents desired to initiate treatment (n=13, 81.2%) and preferred receiving treatment at their primary care clinic (n=13, 81.2%), citing proximity, transportation, and familiarity with providers as positives. Eleven respondents (68.8%) scheduled a follow-up encounter to initiate treatment.
We completed a clinic-based QI project to identify patients with untreated HCV and understand the barriers to treatment for these individuals. Most participants were aware of their HCV diagnosis and were interested in initiating treatment through their PCP. By creating appointments dedicated to HCV treatment directly after the survey, additional scheduling barriers were reduced.
The fact that one-third did not understand HCV infection and that five said no provider had ever explained it to them emphasizes the need for greater patient education at our clinic, which has since been addressed.
Patients reported diverse barriers to treatment suggesting that greater patient assistance by staff and monitoring of follow up is needed to ensure HCV patients are fully treated. Additionally, in this small sample of patients, the majority preferred to receive treatment at their primary care clinic. This emphasizes the need for further study on how to increase HCV services at this and other primary care clinics.
We experienced challenges with our project. Many patients had moved or changed phone numbers so we were unable to contact them. At the time of this publication we have treated eight patients who completed the survey. We sent registered letters to those who have not followed up and flagged their charts for treatment.
This QI project has demonstrated that previously untreated patients with HCV from ethnically diverse and disadvantaged backgrounds can be—and desire to be—treated by their own providers in primary care.
References
- Geddawy A, Ibrahim YF, Elbahie NM, Ibrahim MA. Direct acting anti-hepatitis C virus drugs: clinical pharmacology and future direction. J Transl Int Med. 2017;5(1):8-17. doi:10.1515/jtim-2017-0007
- Too few people treated for hepatitis C. Centers for Disease Control and Prevention. Accessed July 18, 2024. https://www.cdc.gov/vitalsigns/hepc-treatment/index.html.
- McGowan CE, Fried MW. Barriers to hepatitis C treatment. Liver Int. 2012;32(0 1)(suppl 1):151-156. doi:10.1111/j.1478-3231.2011.02706.x
- Kattakuzhy S, Gross C, Emmanuel B, et al; ASCEND Providers. Expansion of treatment for hepatitis C virus infection by task shifting to community-based nonspecialist providers. Ann Intern Med. 2017;167(5):311-318. doi:10.7326/M17-0118



There are no comments for this article.