Introduction: Data on the implementation of successful pediatric ambulatory curricula in residency are limited. Although most pediatric residents pursue careers in primary care, the educational focus in residency training sways toward inpatient medicine. Barriers exist to standardized, consistent teaching in the outpatient clinic. We aimed to create a novel longitudinal ambulatory curriculum focusing on high-yield topics geared toward modern learners that would be well-received and result in retained knowledge.
Methods: Thirty-two pediatric residents were exposed to an 18-month curriculum consisting of 62 high-yield ambulatory topics. Standardized topic guides were taught in brief sessions weekly. Pre- and posttests, midcurriculum cumulative exams, and a 1-year follow-up exam assessed baseline knowledge and long-term retention. We used a Likert scale (1=not at all, 5=very much) to assess satisfaction and use of the curriculum in clinical practice.
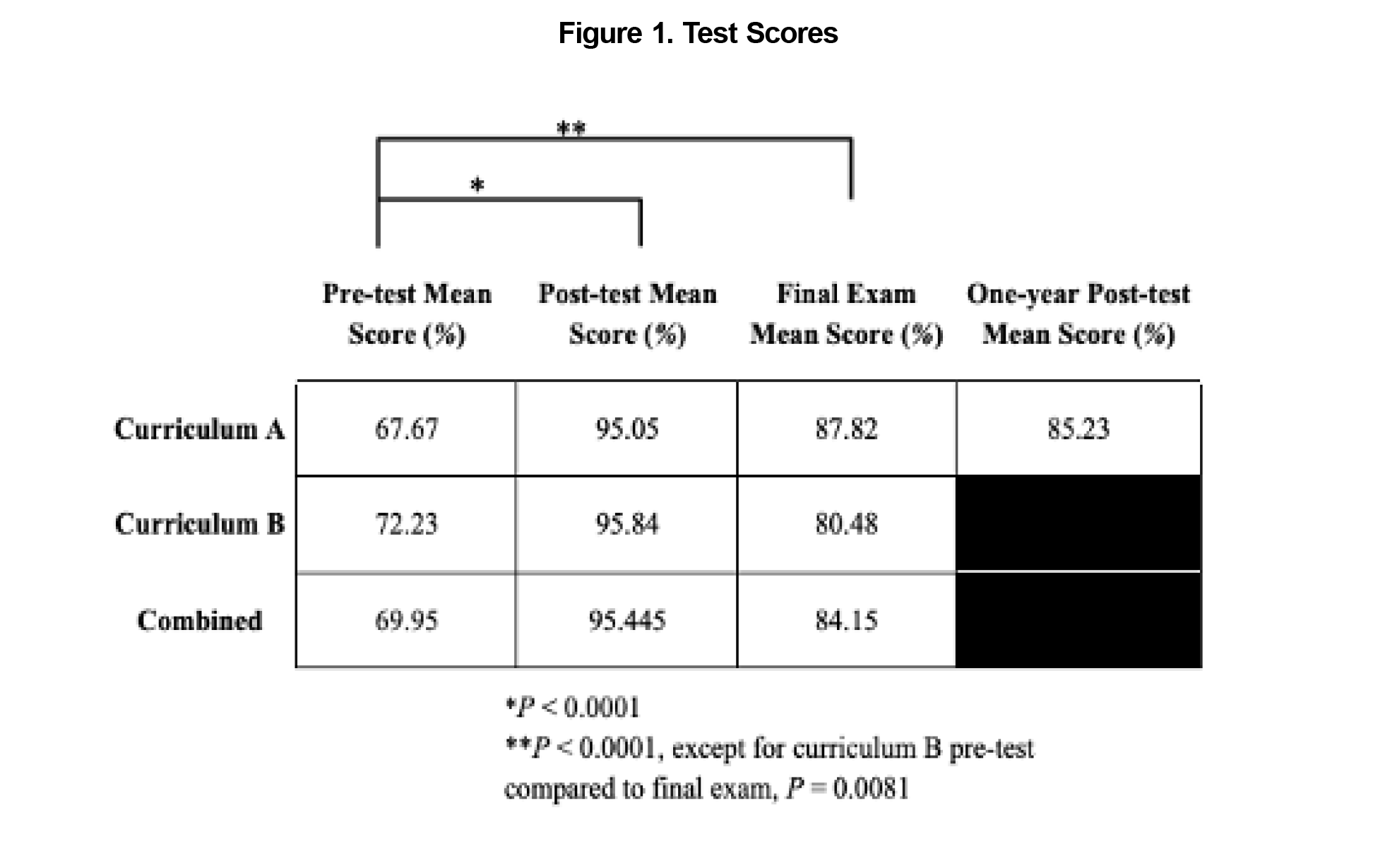
Results: Mean weekly scores increased from pretest to posttest and from pretest to final exam for each half curriculum. The mean test score 1 year later was sustained at over 85%. Mean satisfaction and effectiveness scores were 4.6 and 4.5, respectively. When asked how much the curriculum was used in clinical practice, the average score was 4.45.
Conclusions: Ambulatory education in residency is often inconsistent, with gaps in published data. We created an approach geared toward modern learners that provided consistent pediatric outpatient education of high-yield topics, was well received, and led to a sustained increase in knowledge. This type of curriculum can be used in other ambulatory settings to improve resident knowledge with minimal interruption to clinical sessions.
The Accreditation Council for Graduate Medical Education (ACGME) acknowledges the requirement for formal outpatient resident education with recent shifts toward increasing ambulatory hours; however, clear and uniform guidelines for implementing these curricula are not emphasized.1 Although the majority of graduates choose primary care, residency education has limited emphasis on formal ambulatory education.2 Gaps in medical knowledge of common ambulatory topics in pediatrics and internal medicine exist, leaving residents feeling better-equipped to practice inpatient medicine.3,4 Furthermore, limited outpatient education can deter residents from choosing outpatient careers.5
Ambulatory education reform is vital for improving knowledge gaps in residency training. Ambulatory curricula are often found to be impractical for residents and challenging for preceptors, so many residents do not fully engage in all components of published curricula.6,7 In addition, current learners, coined “Generation Z,” have unique learning styles; they are independent, technologically driven learners who prefer brief, visually stimulating topics as opposed to traditional lectures. Adult learning theory emphasizes the need to consider generational diversity when tailoring medical curricula.8-12 To address some of these current gaps and limitations, we created a novel, structured, longitudinal pediatric ambulatory curriculum geared toward closing the curricula gap, while providing standardization of ambulatory education and increasing resident knowledge, satisfaction, and practical application. This strategy can be adopted by other primary care programs to improve outpatient residency education.
The Staten Island University Hospital pediatric residency program consists of 24 residents (eight residents per postgraduate year [PGY] class), who attend weekly continuity clinics. The curriculum initially was created to be completed over 12 months and to be repeated annually. Topics were chosen from high-yield pediatric board exam content, common clinical scenarios, and subject areas of previous in-training exams on which residents underperformed. A new topic was scheduled weekly. The clinic preceptors facilitated the small group teaching sessions on the assigned topic with the ambulatory trainees who were scheduled during each clinic session. No prework was assigned. The duration of each teaching session was 10 to 15 minutes, including one- to two-page topic guides prepared by faculty and three to five questions given as pre- and posttests. The planned 12-month curriculum was paused after 9 months due to the pandemic; feedback from residents and faculty was then incorporated, resulting in a revised curriculum following an 18-month structure. With an 18-month curriculum, each topic would be presented twice during each resident’s 3-year training.
The initial curriculum was split into two parts (A and B, with Part B resuming after the pause). A cumulative exam was administered at the end of Parts A and B to objectively assess knowledge retention. Residents who completed Part A also completed a 1-year follow-up exam after completion of the curriculum to assess long-term knowledge retention. We used a Likert scale from 1 to 5 (1=not at all, 5=very much) to assess resident satisfaction scores, increase in knowledge, and use of the curriculum in clinical practice.
We described continuous variables by mean and standard deviations, and summarized categorical data as frequency counts and percentages. We used a paired t test to compare continuous variables between pre- and postintervention. We used the analysis of variance method to compare mean differences between PGYs. All statistical tests were two-sided. P values less than .05 were considered significant. All statistical analyses were performed using SAS version 9.4 (Statistical Analysis Systems Inc). The project was submitted for human subject research determination review and was determined to be exempt from review by the institutional review board.
Thirty-two residents were exposed to the curriculum; 16 participated in both parts of the curriculum (A and B). We noted increases in knowledge with the implementation of the new curriculum. Figure 1 demonstrates cumulative mean test scores for the weekly pre- and posttests, final exam, and 1-year follow-up exam. Mean posttest scores significantly increased compared to pretest scores for Parts A and B and the overall combined curriculum. Mean final exam scores significantly increased compared to pretest scores, indicating sustained knowledge. The 1-year follow-up mean exam scores for Part A were sustained from the mean final exam scores, demonstrating longitudinal knowledge retention. Although mean follow-up exam scores decreased compared to mean weekly posttest scores, we found statistically significant increases compared to the pretest, demonstrating overall knowledge increase.
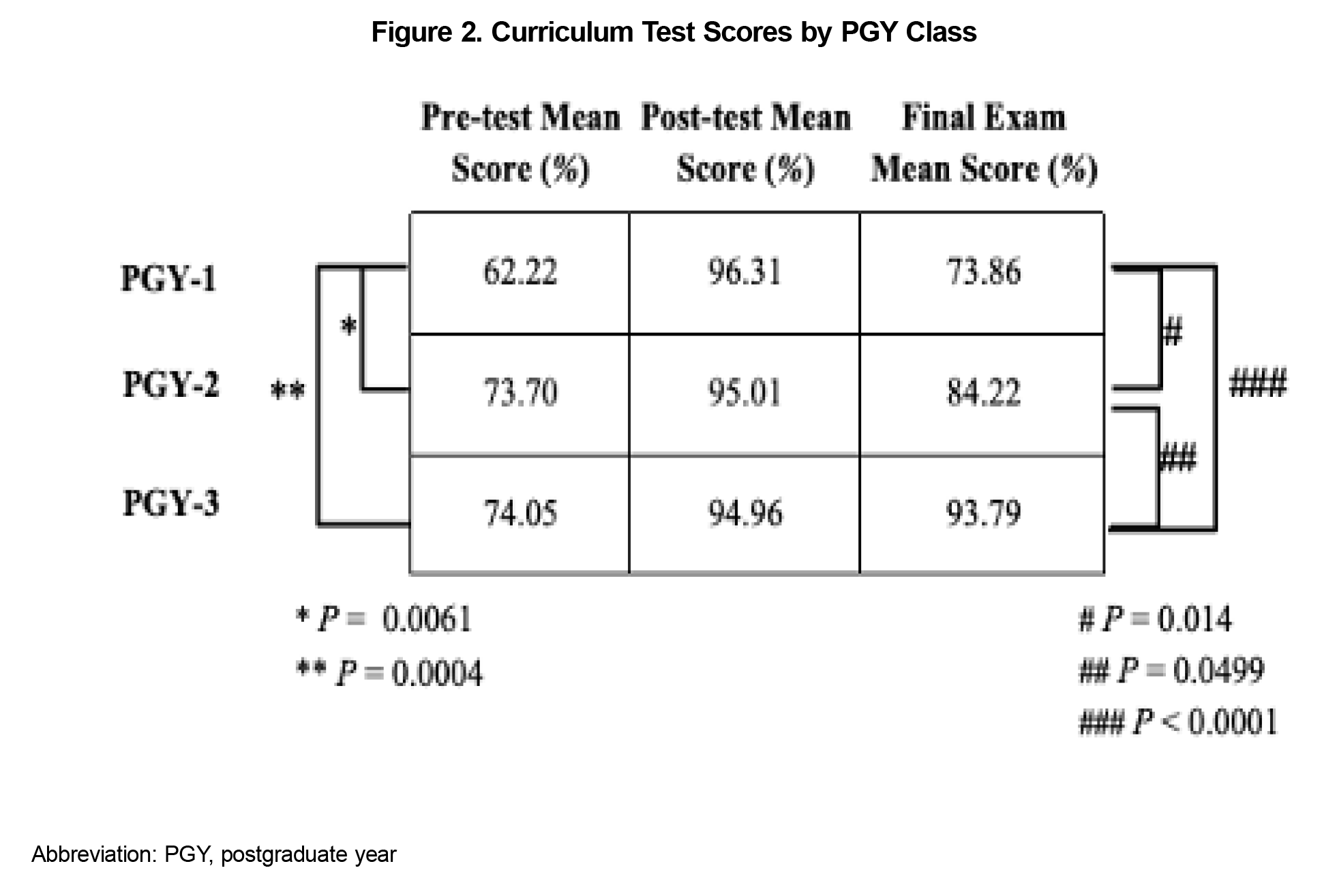
Figure 2 displays mean pretest, posttest, and final exam scores for the combined curriculum by postgraduate year. We noted improvements in pretest to final exam mean scores from PGY-1 to PGY-2 and stronger statistically significant increases from PGY-1 to PGY-3. All three groups showed an increase in knowledge scores from pretest to posttest and follow-up exam, with more experienced residents having higher baseline knowledge scores.
Regarding resident feedback on the curriculum, mean scores (+/– standard deviation) for curriculum efficacy, self-reported increase in knowledge, and overall satisfaction ratings were 4.5 (+/– 0.8), 4.6 (+/– 0.5), and 4.6 (+/– 0.5) out of 5, respectively. When asked whether the knowledge gained from the curriculum was being used in clinical practice, the mean score was 4.45 (+/– 0.6) out of 5. When asked whether the residents planned to use (or continue using) the knowledge gained from the curriculum in clinical practice, the mean response was 4.73 (+/– 0.6) out of 5.
Ambulatory education reform in residency is an understudied yet fundamental area for improving knowledge gaps in residency training. While some residency programs use extramural curricula, they are often found to be impractical for residents and challenging for preceptors, so many residents do not fully engage in all components of published curricula.6,7 The majority of residents do not complete prework due to time restraints and lack of extrinsic motivators, with one study noting 51% of residents did not even open their emails or access the curriculum materials, and only 37% completed the prework.7
We integrated a teaching model that adapted well within busy ambulatory clinics. Generation Z learners have unique learning styles, and adult learning theory emphasizes the need to consider generational diversity when tailoring medical curricula.8-10 Those in Generation Z are independent, technologically driven learners who prefer brief, visually stimulating topics as opposed to traditional didactics and lectures.10-12 We kept teaching points brief and succinct, incorporating short bursts of teaching on practical pediatric topics in small group environments compared to lengthier, in-depth topics that may limit retention. This format targets modern learners and minimizes interruptions to clinic flow and patient care. Adult learning is effective when learners provide input during the process.8 We used resident feedback to tailor the curriculum to the learners’ educational needs.
Our data demonstrated that implementation of a formal ambulatory curriculum geared toward modern pediatric learners improved resident knowledge and increased satisfaction with ambulatory education. Our curriculum provided a standardized outpatient education with consistent topics in a high-yield learning format with easily accessible resources for self-study without relying on prework completion prior to sessions. This specific curriculum and resources can be used by pediatric and family medicine training programs to enhance teaching of pediatric ambulatory topics. The curriculum model can be implemented on a broader scale; it is not only applicable to pediatric and family medicine programs, but also to other disciplines across different institutions to improve resident knowledge and enhance patient care with minimal interruption to the clinical session.
In conclusion, this curriculum was feasible, well-liked by learners, and led to increased knowledge for participants. Generalizability may be limited by the study’s single institution nature and implementation into a small pediatric residency program. Additionally, while attempts were made to standardize teaching with consistent material, sessions were taught by different faculty members, which may have influenced their efficacy and satisfaction scores. Furthermore, not all participants completed the full curriculum. While residents reported using the curriculum in clinical practice, the impact on patient care was not assessed. Finally, a control group of learners who were not exposed to the curriculum was not included in this study; therefore we are not able to determine how much of the improvement in longitudinal testing scores was due to the education provided in the curriculum versus expected increases in knowledge over time for trainees. Future directions include assessing resident behavior changes and effect on direct patient care with chart reviews, direct observations, and patient feedback.
Acknowledgments
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Pediatrics. Accessed December 1, 2024. https://www.acgme.org/globalassets/pfassets/programrequirements/2025-prs/320_pediatrics_2025.pdf
- Coyle A, Helenius I, Cruz CM, et al. A decade of teaching and learning in internal medicine ambulatory education: a scoping review. J Grad Med Educ. 2019;11(2):132-142. doi:10.4300/JGME-D-18-00596.1
- Sisson SD, Dalal D. Internal medicine residency training on topics in ambulatory care: a status report. Am J Med. 2011;124(1):86-90. doi:10.1016/j.amjmed.2010.09.007
- Freed GL, Dunham KM, Switalski KE, Jones MD Jr, McGuinness GA; Research Advisory Committee of the American Board of Pediatrics. Recently trained general pediatricians: perspectives on residency training and scope of practice. Pediatrics. 2009;123(suppl 1):S38-S43. doi:10.1542/peds.2008-1578J
- Brooks JV, Singer SJ, Rosenthal M, Chien AT, Peters AS. Feeling inadequate: residents’ stress and learning at primary care clinics in the United States. Med Teach. 2018;40(9):920-927. doi:10.1080/0142159X.2017.1413236
- Talwalkar JS, Satcher D, Turner TL, Sisson SD, Fenick AM. Use of extramural ambulatory care curricula in postgraduate medical training. Perspect Med Educ. 2015;4(2):93-97. doi:10.1007/S40037-015-0166-Z
- Nicklas D, Lane JL, Hanson JL. If you build it, will they come? a hard lesson for enthusiastic medical educators developing a new curriculum. J Grad Med Educ. 2019;11(6):685-690. doi:10.4300/JGME-D-19-00246.1
- Knowles MS. Andragogy: adult learning theory in perspective. Community Coll Rev. 1978;5(3):9-20. doi:10.1177/009155217800500302
- Sudak DM, ed. Handbook of Psychiatric Education. 2nd ed. American Psychiatric Association Publishing; 2021. https://www.appi.org/Products/Academic-Psychiatry/Handbook-of-Psychiatric-Education-Second-Edition?page=3&SearchText=HandbookofPsychiatricEducation.&SelectedSearchMode=anyword&CurrentTab=products&sku=37344
- Eckleberry-Hunt J, Lick D, Hunt R. Is medical education ready for generation Z? J Grad Med Educ. 2018;10(4):378-381. doi:10.4300/JGME-D-18-00466.1
- Schwartz AC, McDonald WM, Vahabzadeh AB, Cotes RO. Keeping up with changing times in education: fostering lifelong learning of millennial learners. Focus Am Psychiatr Publ. 2018;16(1):74-79. doi:10.1176/appi.focus.20170004
- Hampton D, Welsh D, Wiggins AT. Learning preferences and engagement level of generation Z nursing students. Nurse Educ. 2020;45(3):160-164. doi:10.1097/NNE.0000000000000710



There are no comments for this article.