Introduction: Little is known about patients’ perceptions of their risk for type-2 diabetes (T2D), or if knowledge of risk could facilitate weight and diabetes prevention discussions with health care professionals.
Methods: In our academic family medicine practice, 25 patients completed a previsit T2D risk assessment on their phone and answered interview and survey questions to assess their understanding of their risk for developing T2D.
Results: Interest in their T2D risk was high, but self-estimation of risk before obtaining their score was low (21/25 reported ≤30% chance of developing diabetes). All patients perceived T2D to be very serious, most remembered their risk score (18/23 correct) when interviewed 3-5 days later, and many reported that the score increased their motivation to prevent T2D development. Despite this, the calculated risk result was not considered accurate by 8/23 patients and only 4/23 patients shared their score during their appointment visit.
Conclusion: T2D risk evaluation can facilitate patient awareness of their risk and lifestyle improvement, but clinician engagement and communication are needed for interpretation, treatment, and linkage to prediabetes care.
An estimated 97.6 million (38%) US adults have prediabetes, a condition of abnormally elevated blood glucose (hemoglobin A1C values between 5.7% and 6.4%) that puts them at higher risk of developing type-2 diabetes (T2D).1 Unfortunately, only about 19% report awareness of their prediabetes diagnosis,2 pointing to gaps in screening and identification of those at risk.
Lifestyle modification interventions are recognized by US Preventive Task Force recommendations for effective prevention of disease progression,3 but fewer than 5% of patients report having been referred to prevention programs.4 Primary care physicians (PCPs), the specialty most likely to provide such screening, have reported that providing the diagnosis of prediabetes is effective for advising patients of the need for lifestyle modification.5 However, while PCPs commonly use recommended blood tests when progression to diabetes is suspected, fewer than 30% of PCPs utilize a comprehensive risk questionnaire with their patients. Such questionnaires have been shown to increase the likelihood to order such tests.6 Among the barriers to screening is PCPs’ belief that the prediabetes diagnosis lacks clarity for portraying risk status or the progression toward T2D diagnosis.5, 7
In prior studies, patients described having little knowledge about their likelihood of developing diabetes,4 but tend to underestimate their risk,8, 9 and are uncertain about the seriousness of prediabetes.10 Nevertheless, when a group of patients were notified of their prediabetes diagnosis and followed for 18 months without intervention, their glycemic control and adipose improved in comparison to a control group.11 This suggests that early communication could prompt lifestyle changes that reduce risk even without a physician’s intervention. One way for patients to understand their risk is to use questionnaire-based risk calculators. These have shown good performance in sensitivity and specificity analyses,12 but as described above, their use is limited.6,13 In a prior qualitative study in our own5 and other primary care practices,14 at-risk patients expressed that T2D risk communication was desired, but lacking in their clinician interactions. To assess the effectiveness of implementing called-for15 use of diabetes risk scores in daily clinical practice, we examined patients’ perceptions of risk, T2D seriousness, and validity of a self-assessed T2D risk score. Sharing of risk results in the clinical encounter was the primary outcome.
Data collection for this mixed methods pilot/feasibility study occurred between November 2021 and March 2022 at our academic family medicine practice. One of two female medical student researchers (P.C., H.K.) approached patients in their clinic room while waiting to be seen by their PCP. We sought an approximately equal gender representation and excluded patients with a charted diagnosis of T2D and if they were unable to read and speak English. We used purposive sampling to identify and approach patients with a prior A1C value less than 6.5% in their chart to gain a sample of patients with likely knowledge about their diabetes risk, though a previous A1C blood test was not required for participation. After consent, each patient provided an in-person interview and paper survey of perceived T2D seriousness, perceived personal risk, and validity of T2D risk score assessment. Next, on a smartphone (their own or one provided), they completed the American Diabetes Association (ADA)’s T2D risk assessment.16 Upon completion, patients were asked if they would want their physician to know their risk score and were compensated with a $10 gift card. A subsequent follow-up phone interview was requested of all patients within 5 business days from the in-person session, and a second $15 gift card was mailed to those who completed the interview. Because this was a small pilot study, we did not calculate sample size determinations, and we evaluated data using descriptive statistics. The University of Kentucky Institutional Review Board reviewed and approved the study.
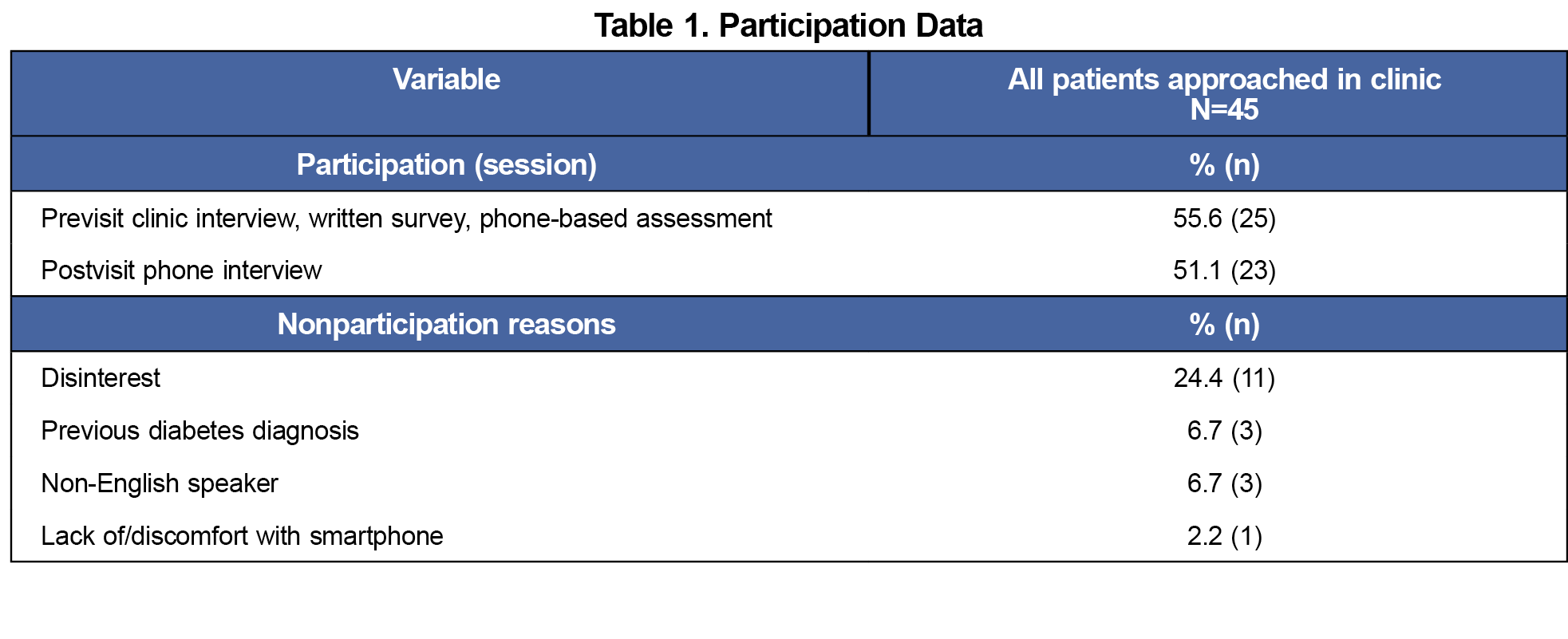
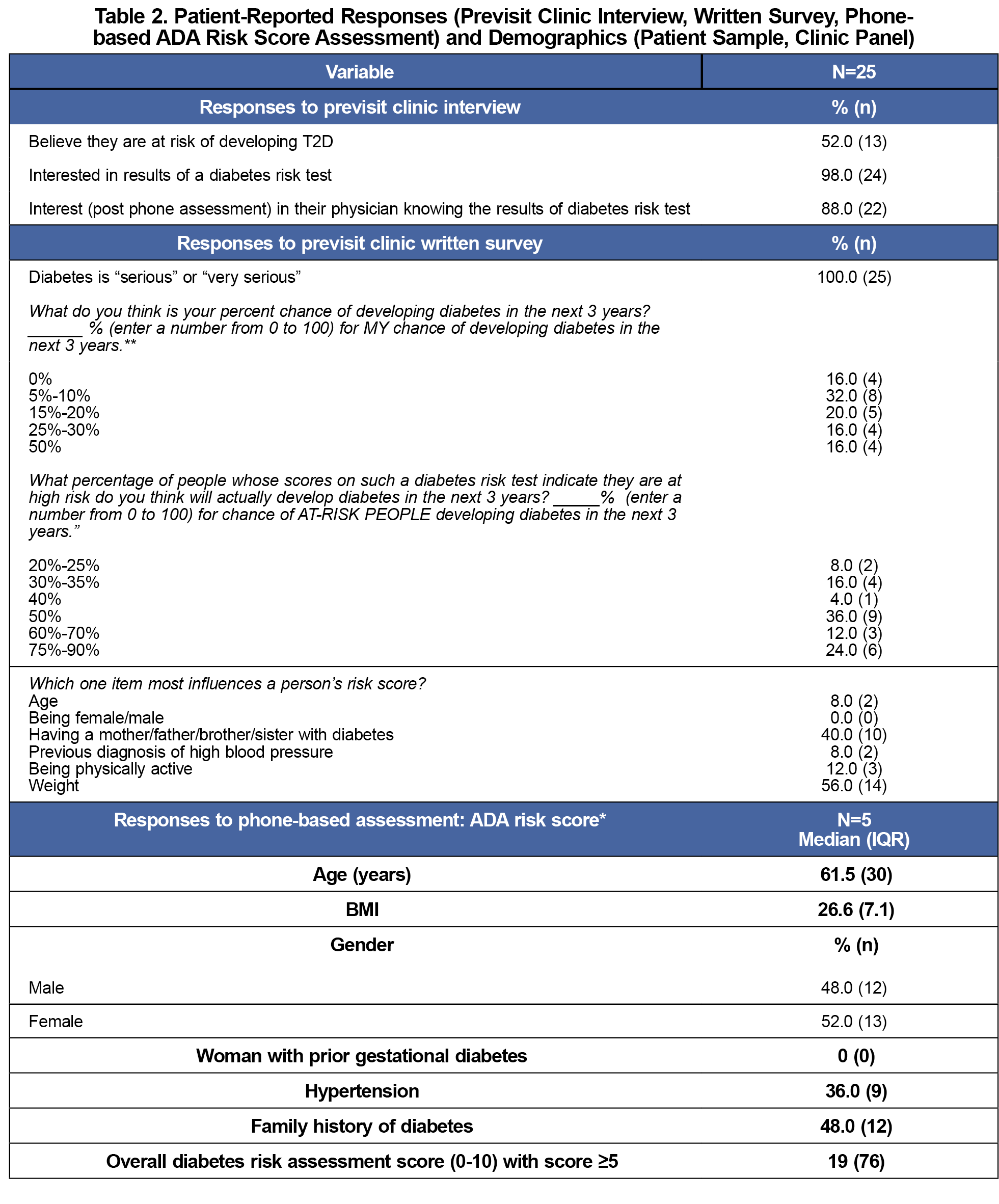
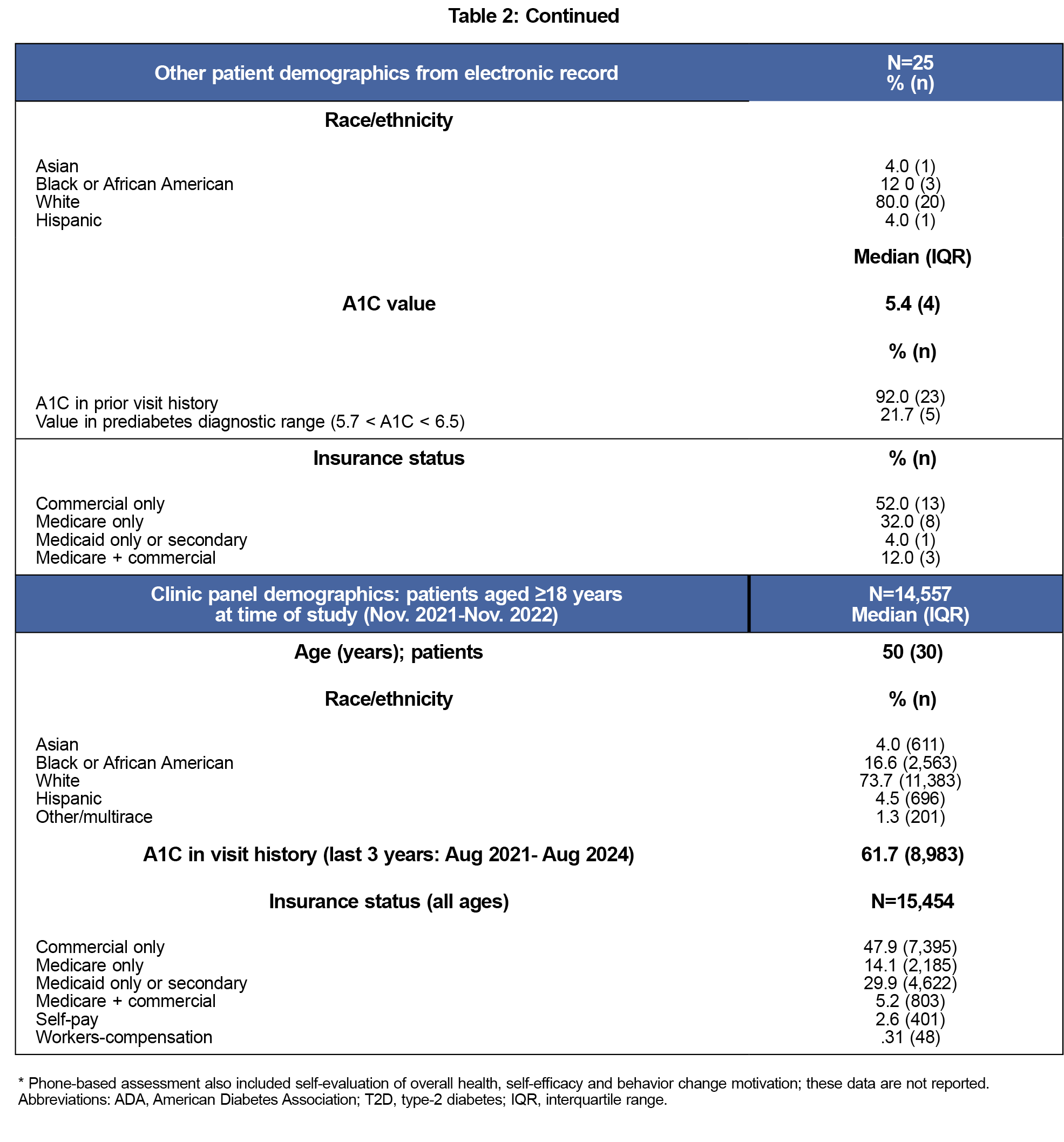
Of 45 patients approached, 25 agreed to participate (Table 1). Nearly all (24/25) participants interviewed endorsed interest in knowing the result of a diabetes risk questionnaire. More than half (13/25) of participants thought they were at risk for developing T2D. Despite this, 21/25 wrote that their chance of developing T2D in the next 3 years was under 30% on the paper form. All participants rated T2D to be serious/very serious and 18/25 thought that a higher risk score indicated a 3-year chance of development to be 50% or greater (actual is 30%17). Weight and family history were the primary components of the T2D risk assessment that they considered most influential.
Prior A1C values were available in the chart for 23/25 patients and 5/23 patients had a value in the prediabetic diagnostic range. A total of 19/25 of the sample obtained a calculation indicating high risk (score ≥5 on the 10-point scale). After receiving their score, 22/25 participants responded that they would want their physician to know the score. Table 2 shows participants’ responses to the in-person interview, paper form, ADA risk assessment, additional demographics from the medical record, and selected demographics of our clinical population.
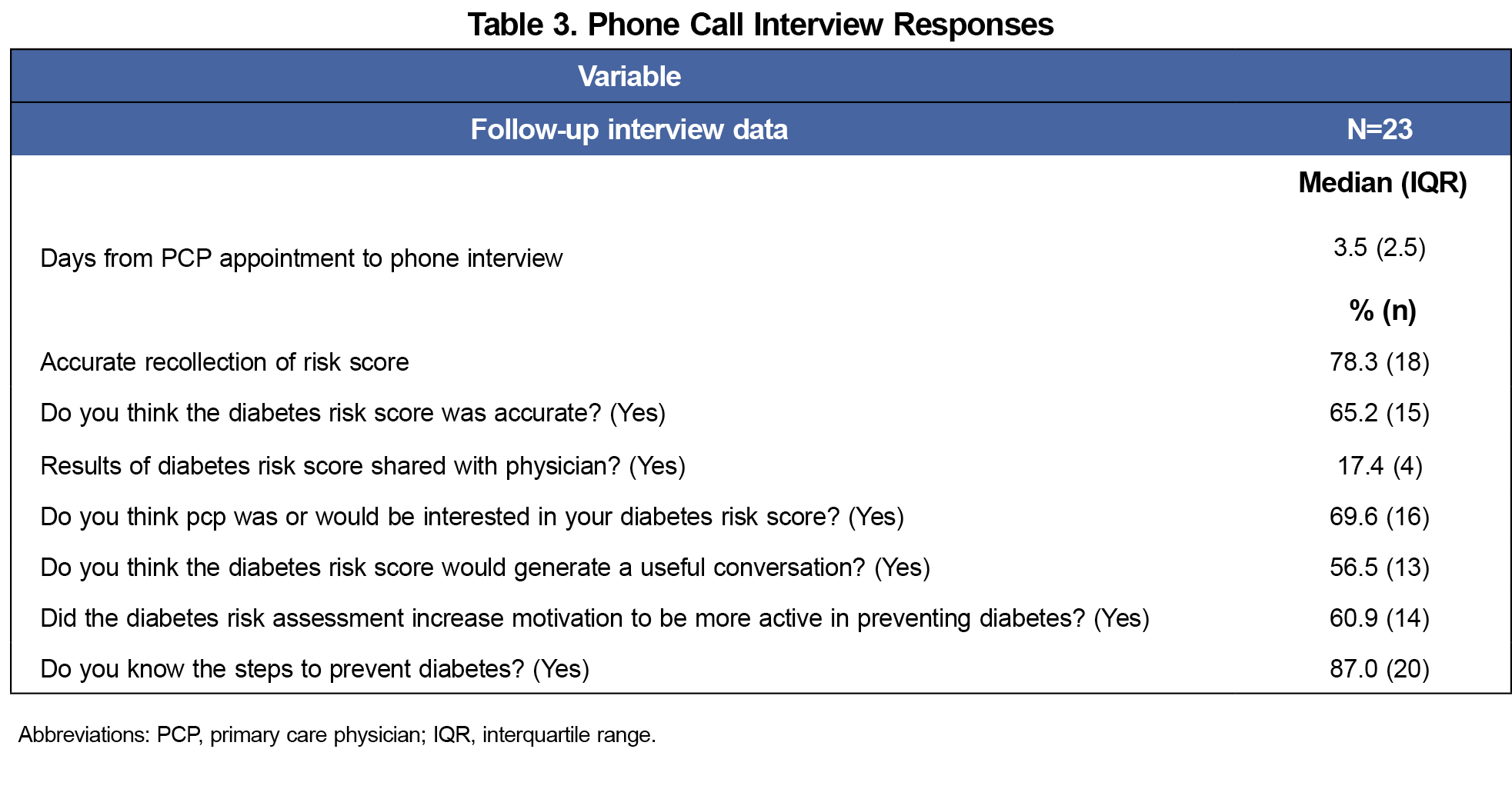
A total of 23/25 of the patients who completed the in-person survey and risk assessment also completed the subsequent interview call. One patient refused and one patient could not be reached. Only 4/23 interviewed patients reported sharing their risk score with their physician during the visit (Table 3), despite the aforementioned interest that they be notified. The most frequent reasons for not sharing the result were other needs to address during the visit and being a new patient. Others assumed the physician had access to the score and would bring it up if necessary. More than one-third (8/23) did not perceive their risk result to be accurate. Nevertheless, most remembered their risk score (18/23 correct recall) and 16/23 felt their PCP would have been interested in the results of the assessment. More than half (14/23) reported increased motivation toward risk reduction to prevent development of diabetes and 20/23 patients felt they understood ways to decrease their risk.
The goal of our study was to evaluate if a T2D risk assessment completed just before patients’ appointments might prime patients to initiate a discussion and possibly further care planning to prevent diabetes progression. A patient-initiated approach may overcome uncertain attitudes toward the uptake of diabetes risk assessment tools by health care practitioners, who report impracticality of using such tools in addition to lack of reimbursement and regulatory support and barriers (eg, lack of resources/time/capability) to initiating prediabetes counseling.13,18,19 Although we did not assess physician attitudes, one multistate study of nurse practitioners (NPs) who have utilized the same risk assessment tool in their clinics provided high ratings of its clinical feasibility, including its value in facilitating conversations about patient diabetes risk.20 Conversations initiated following patient self-assessment may also help allay concerns for prediabetes diagnosis based on A1C screening values, which potentially create unnecessary concern for disease,21 while still maintaining the PCP’s role in fostering a proactive, preventive approach.22 Unfortunately, few patients found an opportunity within their visit to discuss their assessment, indicating a need for greater PCP involvement.
Several studies have shown that patients with risk factors for developing T2D have a low perceived risk of developing the disease, which is consistent with what was observed in this study.8,9, 23 Prior research has found that family history of T2D is a leading correlate of more accurate risk perception.23 Interestingly, of the self-assessed risk factors in this study, patients considered family history to be a leading influence.
Mobile-based applications now provide a wide array of functions intended to bridge the gap between risk assessment and patient-physician discussions, including communication tools and reminders, symptoms monitoring, and goal-setting.24 Given the improvements these tools have had for a number of covered health indications (T2D and hypertension being prominent),24 technology assessing T2DM risk and providing strategies to patients for risk reduction could similarly assist the PCP in facilitating lifestyle improvements in patients who are deemed high risk using the risk assessment and standard A1C screening.
Study Strengths and Limitations
While our study gained a balanced representation of males and females, the overall sample was small, of older age (13/25 over 60 years), and comprised of patients from a single academic medical center’s primary care clinic. The sample, like the clinic’s panel demographics shown in Table 2, reveal this to be a largely White population with a relatively high percentage (30%) with lower income health coverage through Medicaid primary or secondary insurance.
This pilot study suggests that a diabetes risk self-assessment prior to a primary care clinic visit using phone-based technology could be useful in creating awareness of T2D risk. Given that PCPs13 and NPs20 have positive attitudes toward T2D risk assessment tools yet do not routinely utilize them in their clinical practice, additional study of their usefulness and of implementation opportunities and barriers is needed.
References
- Centers for Disease Control and Prevention. National Diabetes Statistics Report 2021. Reviewed November 29, 2023. Accessed December 20, 2024. https://www.cdc.gov/diabetes/data/statistics-report/index.html
- Xia P-F, Tian Y-X, Geng T-T, et al. Trends in prevalence and awareness of prediabetes among adults in the U.S., 2005-2020. Diabetes Care. 2022;45(2):e21-e23. doi:10.2337/dc21-2100
- U.S. Preventive Services Task Force. Final Recommendation Statement: Prediabetes and Type 2 Diabetes: Screening. USPSTF. August 24, 2021. Accessed December 20, 2024. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/screening-for-prediabetes-and-type-2-diabetes#fullrecommendationstart
- Venkataramani M, Pollack CE, Yeh HC, Maruthur NM. Prevalence and correlates of diabetes prevention program referral and participation. Am J Prev Med. 2019;56(3):452-457. doi:10.1016/j.amepre.2018.10.005
- Roper KL, Thomas AR, Hieronymus L, Brock A, Keck J. Patient and clinician perceptions of prediabetes: a mixed-methods primary care study. Diabetes Educ. 2019;45(3):302-314. doi:10.1177/0145721719845347
- Nhim K, Khan T, Gruss SM, et al. Primary care providers’ prediabetes screening, testing, and referral behaviors. Am J Prev Med. 2018;55(2):e39-e47. doi:10.1016/j.amepre.2018.04.017
- Thomas JJ, Moring JC, Baker S, et al. Do words matter? Health care providers’ use of the term prediabetes.Health Risk Soc. 2017;19(5-6):301-315. doi:10.1080/13698575.2017.1386284
- Kowall B, Rathmann W, Stang A, et al. Perceived risk of diabetes seriously underestimates actual diabetes risk: the KORA FF4 study. PLoS One. 2017;12(1):e0171152. doi:10.1371/journal.pone.0171152
- Heidemann C, Paprott R, Stühmann LM, et al. Perceived diabetes risk and related determinants in individuals with high actual diabetes risk: results from a nationwide population-based survey. BMJ Open Diabetes Res Care. 2019;7(1):e000680. doi:10.1136/bmjdrc-2019-000680
- Troughton J, Jarvis J, Skinner C, Robertson N, Khunti K, Davies M. Waiting for diabetes: perceptions of people with pre-diabetes: a qualitative study. Patient Educ Couns. 2008;72(1):88-93. doi:10.1016/j.pec.2008.01.026
- Owei I, Umekwe N, Ceesay F, Dagogo-Jack S. Awareness of prediabetes status and subsequent health behavior, body weight, and blood glucose levels. J Am Board Fam Med. 2019;32(1):20-27. doi:10.3122/jabfm.2019.01.180242
- Poltavskiy E, Kim DJ, Bang H. Comparison of screening scores for diabetes and prediabetes. Diabetes Res Clin Pract. 2016;118:146-153. doi:10.1016/j.diabres.2016.06.022
- Dhippayom T, Chaiyakunapruk N, Krass I. How diabetes risk assessment tools are implemented in practice: a systematic review. Diabetes Res Clin Pract. 2014;104(3):329-342. doi:10.1016/j.diabres.2014.01.008
- O’Brien MJ, Moran MR, Tang JW, et al. Patient perceptions about prediabetes and preferences for diabetes prevention. The Diabetes Educator. 2016;42(6):667. doi:10.1177/0145721716666678
- Duan D, Kengne AP, Echouffo-Tcheugui JB. Screening for Diabetes and Prediabetes. Endocrinol Metab Clin North Am. 2021;50(3):369-385. doi:10.1016/j.ecl.2021.05.002
- Bang H, Edwards AM, Bomback AS, et al. Development and validation of a patient self-assessment score for diabetes risk. Ann Intern Med. 2009;151(11):775-783. doi:10.7326/0003-4819-151-11-200912010-00005
- Knowler WC, Barrett-Connor E, Fowler SE, et al; Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393-403. doi:10.1056/NEJMoa012512
- Messina J, Campbell S, Morris R, Eyles E, Sanders C. A narrative systematic review of factors affecting diabetes prevention in primary care settings. PLoS One. 2017;12(5):e0177699. doi:10.1371/journal.pone.0177699
- Tseng E, Greer RC, O’Rourke P, et al. National Survey of Primary Care Physicians’ Knowledge, Practices, and Perceptions of Prediabetes. J Gen Intern Med. 2019;34(11):2475-2481. doi:10.1007/s11606-019-05245-7
- Marjama KL, Oliver JS, Hayes J. Nurse Practitioner Perceptions of a Diabetes Risk Assessment Tool in the Retail Clinic Setting. Clin Diabetes. 2016;34(4):187-192. doi:10.2337/cd15-0054
- Rani M. Is Prediabetes Overdiagnosed? Yes: A Patient-Epidemiologist’s Experience. Ann Fam Med. 2024;3093(3):247-250. doi:10.1370/afm.3093
- Jonathan GG. Is Prediabetes Overdiagnosed? No: A Clinician’s Perspective. Ann Fam Med. 2024;3101(3):251-253. doi:10.1370/afm.3101
- Joiner KL, Adams MP, Lee KA, Piatt G, Davis MA. Perceived risk for diabetes among U.S. adults with undiagnosed prediabetes. Prev Med. 2022;160:107089. doi:10.1016/j.ypmed.2022.107089
- Chong SOK, Pedron S, Abdelmalak N, Laxy M, Stephan AJ. An umbrella review of effectiveness and efficacy trials for app-based health interventions. NPJ Digit Med. 2023;6(1):233. doi:10.1038/s41746-023-00981-x



There are no comments for this article.