Introduction: Continuous glucose monitoring (CGM) has become an essential tool in managing diabetes, offering real-time insights that improve patient engagement, decision-making, and clinical outcomes. Despite its benefits, CGM is underutilized in primary care due to perceived complexity and time constraints. This study aimed to enhance health care professionals' understanding of and confidence in prescribing CGM technology through two multidisciplinary, hands-on workshops.
Methods: A total of 51 participants, including family medicine residents, faculty, clinical staff, and pharmacists, attended hands-on workshops and wore a CGM for 10-14 days. We analyzed prescribing patterns using EHR data to compare CGM orders placed before and after the workshops. Additionally, we evaluated pre- and postworkshop surveys’ changes in participants’ comfort, knowledge, and likelihood of recommending CGMs to patients.
Results: Results showed a 31% improvement in participants' prescribing patterns of CGMs after holding the workshops. Qualitative feedback highlighted insights into device usability, blood sugar patterns, and patient counseling.
Conclusion: This study demonstrates the value of experiential learning in improving health care providers' competence with diabetes technologies. Future research should explore the long-term impact of such training on clinical practice and patient outcomes.
Continuous glucose monitoring (CGM) has emerged as a valuable tool in diabetes self-management and is increasingly recognized as a standard of care for individuals using insulin and noninsulin therapies.5 By providing real-time insights into ambulatory blood glucose (ABG) levels, CGM facilitates data-driven, therapeutic decision-making and enhances patient understanding and engagement in adjusting their behaviors and lifestyle. This, in turn, leads to more meaningful discussion and collaborative patient–clinician interactions beyond the limitations of relying on HbA1c alone.2 Previous studies have shown that CGM is a cost-effective adjunct to diabetes management that has the potential to improve glycemic outcomes and quality of life in patients with diabetes.3
Despite these benefits, optimal utilization of CGM data remains a challenge in clinical practice. One study found that only 38.6% of primary care physicians report ever prescribing CGMs.4 Time constraints, frequent technological updates, and perceived complexity of device use and management often lead to underutilization by clinicians. Family medicine providers at our clinic tend to defer CGM device initiation and education to specialists for these reasons, reflecting broader trends in primary care.
Currently, medical students and residents may encounter CGM technology during lectures, electives, or special pilot programs—but there is no standardized requirement across all programs that ensures robust, hands-on education in CGM.5 The 2025 American Diabetes Association Standards of Care emphasize the need for health care professionals to develop competencies in diabetes technology, but translating that into uniform curricular mandates is still a work in progress.1 Many clinics operate without access to diabetes specialists such as educators, clinical pharmacists, or endocrinologists, leaving the responsibility for diabetes technology management primarily in the hands of physicians. Education, training, and ongoing support are critical to maximizing the utility of these devices.
This project aimed to address these gaps through innovative, hands-on, multidisciplinary workshops designed to improve health care professionals’ understanding and confidence with CGM technology. The workshops also introduced participants to new over-the-counter CGM devices that eliminate the need for a prescription, further enhancing accessibility. By incorporating a 10-14-day trial of wearing a CGM device, this study sought to evaluate whether such experiential learning improves clinicians’ likelihood of prescribing CGMs to patients, comfort in counseling, and overall attitudes toward their use in diabetes management.
The expedited review committee of the BayCare Health System Institutional Review Board (IRB) approved the protocol. Dexcom G7 and Freestyle Libre 3 CGM systems were donated to our graduate medical education (GME) program for two hands-on workshops involving all direct patient care team members, including family medicine residents, supervising physicians, clinical staff, psychologists, and clinical pharmacists. Participants had the option to wear CGM devices to gain experience on device placement, monitoring using smart phone apps, and interpretation of readings. We excluded front office, triage, and nonclinical team members from these workshops.
Two 1-hour workshops were organized by our interprofessional faculty to provide participants with education and an opportunity to ask questions about CGM use. Topics included outcome data from trials investigating CGM benefits, interpretation of ambulatory glucose profiles, management of hypoglycemia events, remote monitoring, insurance coverage, and office billing considerations (Appendix 1).
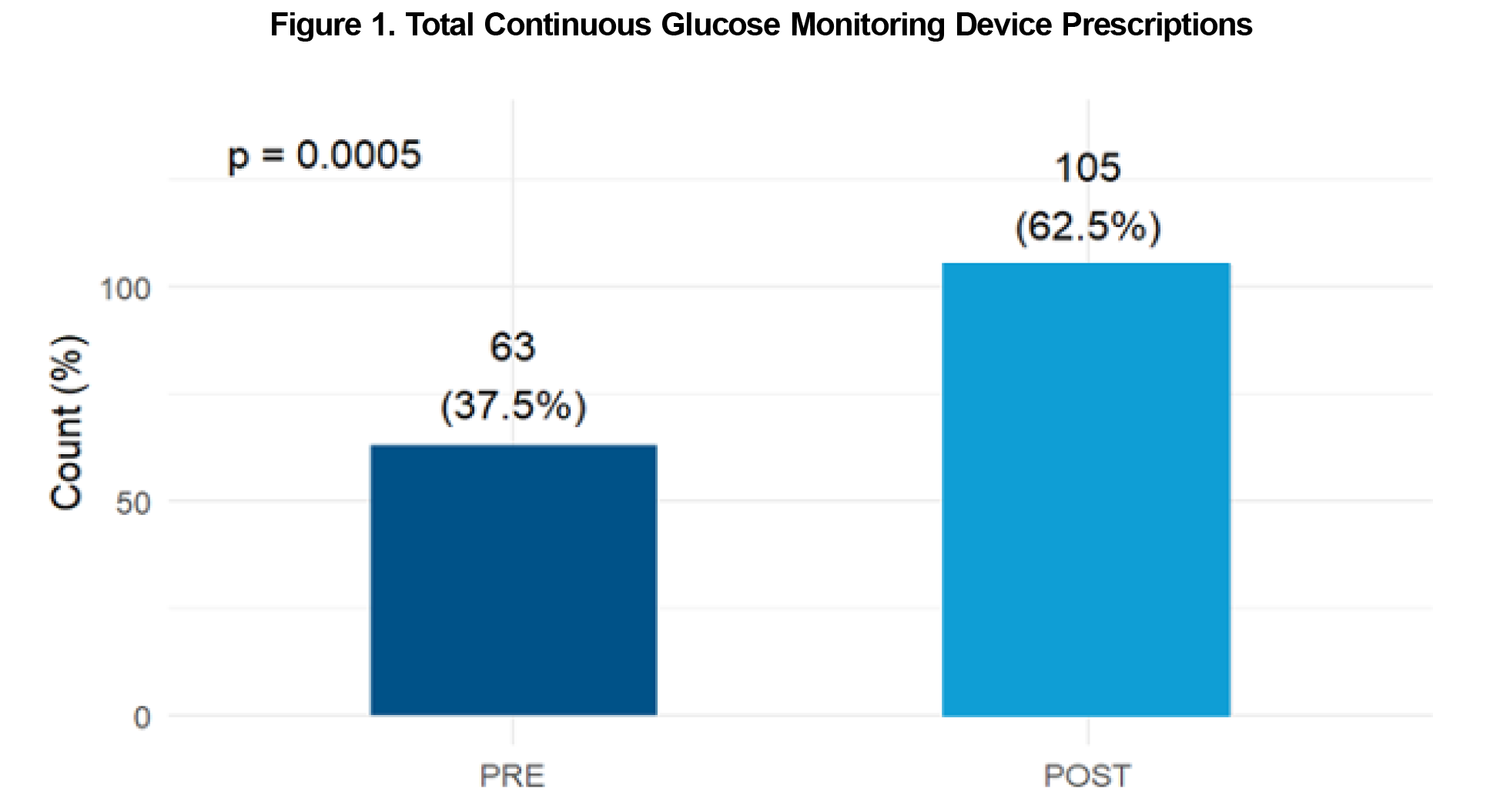
Prescribing patterns were analyzed using electronic health record (EHR) data to compare CGM device orders by faculty physicians and residents before and after the workshops. The preintervention period spanned from July 1, 2024 to December 31, 2024, while the postintervention period covered January 1, 2025 to June 30, 2025. Differences in prescribing proportions between the two periods were assessed using the χ2 test.
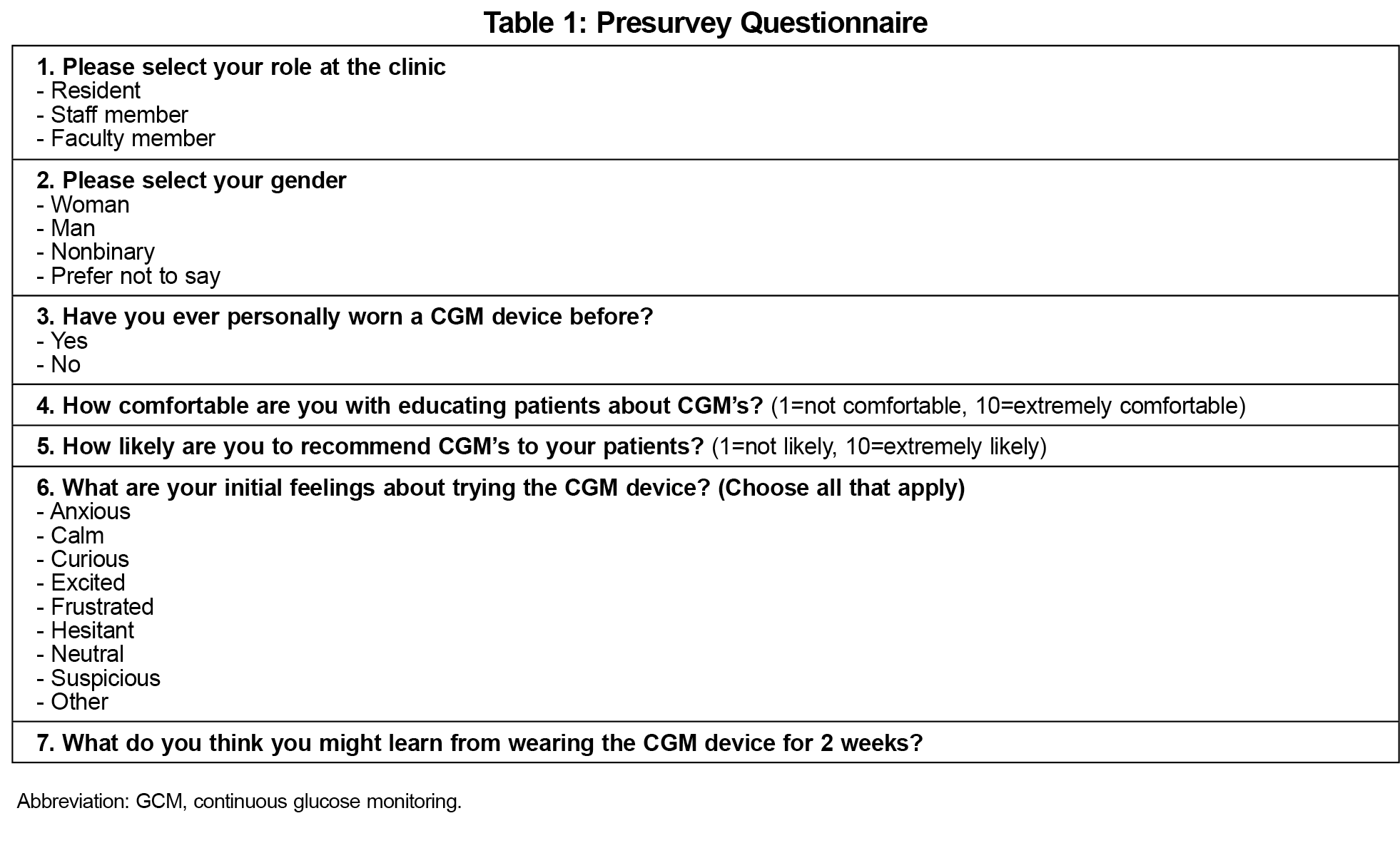
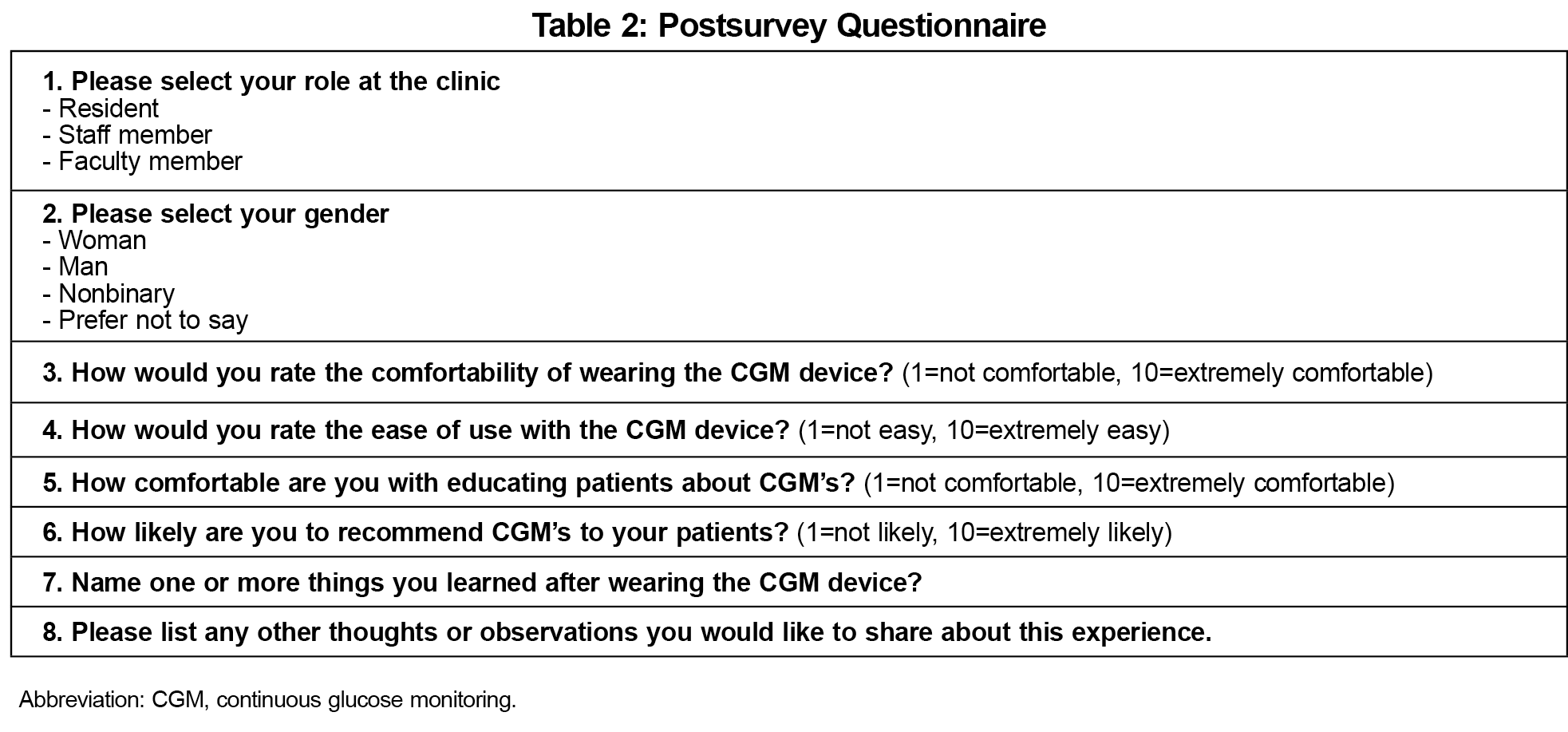
We developed a pre and postsurvey and distributed this to the participants (Tables 1 and 2). These brief 5-minute questionnaires asked about overall feelings towards the devices, perceived comfortability and understanding of CGMs, and likelihood to recommend to a patient before and after the workshops and trial periods. The pre and postsurveys were voluntary, anonymous, and completed online via Microsoft Forms. We used descriptive statistics to analyze survey results.
Prescribing Patterns
A total of 168 CGM prescription orders were placed during the study period. Of those, 40 orders (24%) were entered by a faculty physician or faculty pharmacist and 128 orders (76%) were placed by a resident physician or resident pharmacist. Following the hands-on CGM workshops, there was a significant increase in CGM orders across all prescriber groups, with 105 orders placed post-intervention compared to 63 orders preintervention (P<.05). Notably, residents in both family medicine and pharmacy demonstrated a significant increase in CGM prescribing after the intervention (P=.0005; Figure 1). No significant difference was observed in the choice of CGM device prescribed within the cohort (P=.415).
Survey Results
We collected pre- and postsurveys from 50 and 30 participants, respectively. The presurvey sample consisted of family medicine residents (50%), faculty (32%), and clinical office staff (18%). Seventy-two percent of respondents in the presurvey identified as female and 28% as male. Sixty-six percent of participants had never personally used a CGM device before. Prsurvey results found the top-three emotions associated with trying the device to be “curious,” “excited,” and “calm.”
The postsurvey sample consisted of family medicine residents (60%), faculty (30%), and clinical office staff (10%). Postsurvey results found the top-three emotions associated with having tried the CGM device to be “excited,” “curious,” and “calm.”
As a result of personally wearing the CGM devices, participants' rating of their comfort in educating patients about CGM devices increased from 6.1 (pre) to 9.0 (post) on a scale of 1-10. Similarly, participants' rating of their likelihood to recommend a CGM device to patients increased from 8.16 (pre) to 9.43 (post) out of 10. Postsurvey results also reported that the subjective comfort of wearing the device was 8.67 out of 10 and the ease of using the device was 8.67 out of 10. This was not assessed in the presurvey.
Qualitative comments from the presurvey included themes of wanting to learn more about device use and comfort, dietary and lifestyle factors, influence on blood sugar readings, counseling and patient application and accessibility and trouble shooting. Postsurvey qualitative comments included themes of comfort and ease of use, insights into blood sugar patterns and educational, technical, and usability takeaways.
Despite strong guideline recommendations, CGM use for managing diabetes remains underutilized in the primary care setting. This distinction is particularly relevant given the current environment of longer wait times for specialist’s care leaving many patients to rely on their primary care team for timely diabetes management. The 2025 American Diabetes Association Standards of Care emphasize that all health care professionals involved in diabetes care should be proficient in the use of technologies such as CGM, underscoring the expectation that this knowledge extends beyond endocrinology. Initiatives like ours help bridge this gap by equipping nonspecialist health care professionals with hands-on knowledge of emerging technologies, such as CGMs, to improve their comfort and confidence in recommending these tools to patients. By equipping clinicians with the knowledge and skills necessary to integrate these tools into practice, clinical pharmacists, diabetes educators, and others can help reduce therapeutic inertia and promote meaningful improvements in glycemic outcomes. Through these multidisciplinary workshops, we provided health care personnel—including family medicine residents, supervising physicians, clinical staff, psychologists, and clinical pharmacists—with firsthand experience of wearing CGM devices. This allowed participants to navigate the practical and technological aspects of device utilization while appreciating both strengths and challenges.
The execution of such hands-on workshops increased prescribing patterns of CGMs in both our faculty and resident prescribers. There was no evidence of bias towards a particular CGM device brand after the workshops. With the advent of over-the-counter CGM options, such workshops can play a pivotal role in empowering providers to embrace these technologies and better support patients who stand to benefit. Our in-person CGM workshops significantly improved participants' comfort, understanding, and likelihood to prescribe CGMs, highlighting the value of experiential learning in GME.
Some limitations apply to this study. Analyses were based on a small sample as the postsurvey had a low response rate. The study design did not allow for a control group as the training aimed to reach the largest possible target audience. Additionally, this study focused solely on prescriber orders and did not assess the rate at which patients successfully obtained CGM devices from the pharmacy or initiated their use. Lastly, the setting of this study was an academic clinic and may not be reproducible in a traditional family medicine clinic.
Future efforts should focus on evaluating the long-term impact of such training on patient outcomes and integration of CGM use into routine primary care. Our clinic plans to host these workshops annually to further understand the long-term impacts and provide continuing education on the frequent advancements of diabetes technology. These findings underscore the importance of fostering interprofessional collaboration and continued education to advance diabetes care in primary care settings. Additionally, this CGM workshop highlights the essential role of technology-focused education in family medicine and supports broader GME goals by equipping residents with the skills and mindset needed to adopt and integrate emerging tools such as AI and remote patient monitoring into their future clinical practice.
Acknowledgments
Financial support: Dexcom & Freestyle donated continuous glucose monitoring devices, but provided no financial support.
Conflict of Interest Statement: The authors have no conflicts of interest to disclose.
References
- ElSayed NA, McCoy RG, Aleppo G, et al; American Diabetes Association Professional Practice Committee. Diabetes technology: standards of care in diabetes-2025. Diabetes Care. 2025;48(1)(suppl 1):S146-S166. doi:10.2337/dc25-S007
- Beck RW, Riddlesworth TD, Ruedy K, et al; DIAMOND Study Group. Continuous glucose monitoring versus usual care in patients with type 2 diabetes receiving multiple daily insulin injections: a randomized trial. Ann Intern Med. 2017;167(6):365-374. doi:10.7326/M16-2855
- Mullen DM, Bergenstal R, Criego A, Arnold KC, Goland R, Richter S. Time savings using a standardized glucose reporting system and ambulatory glucose profile. J Diabetes Sci Technol. 2018;12(3):614-621. doi:10.1177/1932296817740592
- Oser TK, Hall TL, Dickinson LM, et al. Continuous glucose monitoring in primary care: understanding and supporting clinicians’ use to enhance diabetes care. Ann Fam Med. 2022;20(6):541-547. doi:10.1370/afm.2876
- Knezevich E, Fuji KT, Larson K, Muniz G. A cross-sectional survey study examining the provision of continuous glucose monitoring education in U.S. doctor of pharmacy programs. Pharmacy (Basel). 2022;10(6):174. doi:10.3390/pharmacy10060174



There are no comments for this article.