Introduction: Oral health is important and affects overall health. Medical students face both common and unique barriers to preserving their own oral health care. This study was designed to survey medical students at the University of Massachusetts Chan Medical School (UMass Chan) to evaluate their oral health hygiene practice and identify barriers to dental care.
Methods: We disseminated a 15-question survey to the student body via email, class Facebook pages, and in-person lecture announcements. We used bivariate analyses (using ꭓ2 tests) to identify any associations among select variables.
Results: Fifty-four percent of students responded to the survey. Of those, 84% brushed their teeth at least twice a day, however only 63% visited a dentist in the last 12 months. Reported barriers to dental visits included being too busy, not knowing how to find local dentists that accepted student dental insurance plans, and lack of finances especially for Hispanic students. We found no significant differences between preclinical and clinical students, however younger age (<26) was associated with more recent dental visits. Students enrolled in Medicaid had larger gaps in care compared to those with private insurance.
Conclusions: UMass Chan students face barriers to professional dental care and do reasonably well on personal dental hygiene. To improve access to dental care, especially for those on Medicaid, efforts should be made to provide referral resources and consider an on-campus dental clinic. Hispanic students may need more money in their loan package. More study on this topic is needed nationally.
The personal health of medical students is often neglected due to significant barriers.1,2 These barriers include lack of time, financial constraints, and proximity to specialty care (eg, vision). Less is known about barriers affecting the oral health of medical students. Yet, oral health is an important aspect of overall health. Oral diseases are common3 and, untreated, are associated with poor social well-being and increased all-cause mortality.4-6
A study at one medical school (in Pennsylvania) reported that individuals seek dental care less after entering medical school.2 Little is known about US medical students’ personal oral hygiene habits or barriers in other parts of the country. A national study of college students confirmed that undergraduates visit the dentist more regularly than medical students.7 Similarly, a single-site study of undergraduate dental care noted that undergraduates brush their teeth regularly.8 In general, medical students have some unique barriers for addressing health issues, including excessive workload, significant stress, and changes in dietary habits.2,9,10 Furthermore, medical students are at an age where they lose parental insurance coverage, which disrupts medical and dental care.11 Older medical students often enroll in Medicaid, which has variable dental coverage and access depending on the state.12
To address the dearth of studies assessing oral health habits and dental visit regularity of US medical students, we surveyed students at the University of Massachusetts Chan Medical School (UMass Chan) regarding personal oral hygiene habits and barriers to accessing dental care.
Study Population
The survey was sent to medical students at UMass Chan (N=685). The study was deemed exempt by the UMass Chan Institutional Review Board. Participants were informed about risks and confidentiality, and consent was obtained.
Data Collection
We developed a 15-question online survey to evaluate barriers to dental care access and self-care. Survey questions were based on external sources (eg, National College Health Assessment).13 Students were asked about demographics (eg, race, gender), dental hygiene, dental visits, and barriers to care. The survey was pilot tested with five students to ensure ease of use.
The survey was sent to students via 4 weekly class Facebook group notices and email bulletins during December 2022. Announcements were made in person twice in first- and second-year classes and virtually in one third-year class. The fourth-year class did not receive in-person announcements. Participants could anonymously enter a drawing for $25 gift cards. We used Qualtrics for the survey’s dissemination and data collection.
Data Analysis
The data was transferred to SPSS version 28 (IBM) for analyses, using a P value of .05 for statistical significance. For select survey questions (eg, last dental visit), responses were recoded from four- or six-point Likert-type scales into two- or three-level categorical variables due to small sample sizes in select responses. Descriptive data analyses were followed, and bivariate analyses (using ꭓ2 tests) were used to identify associations among select variables.14 Comparative analysis of responses by demographics was based on previous literature, excluding race due to the small sample size at UMass Chan.11,13
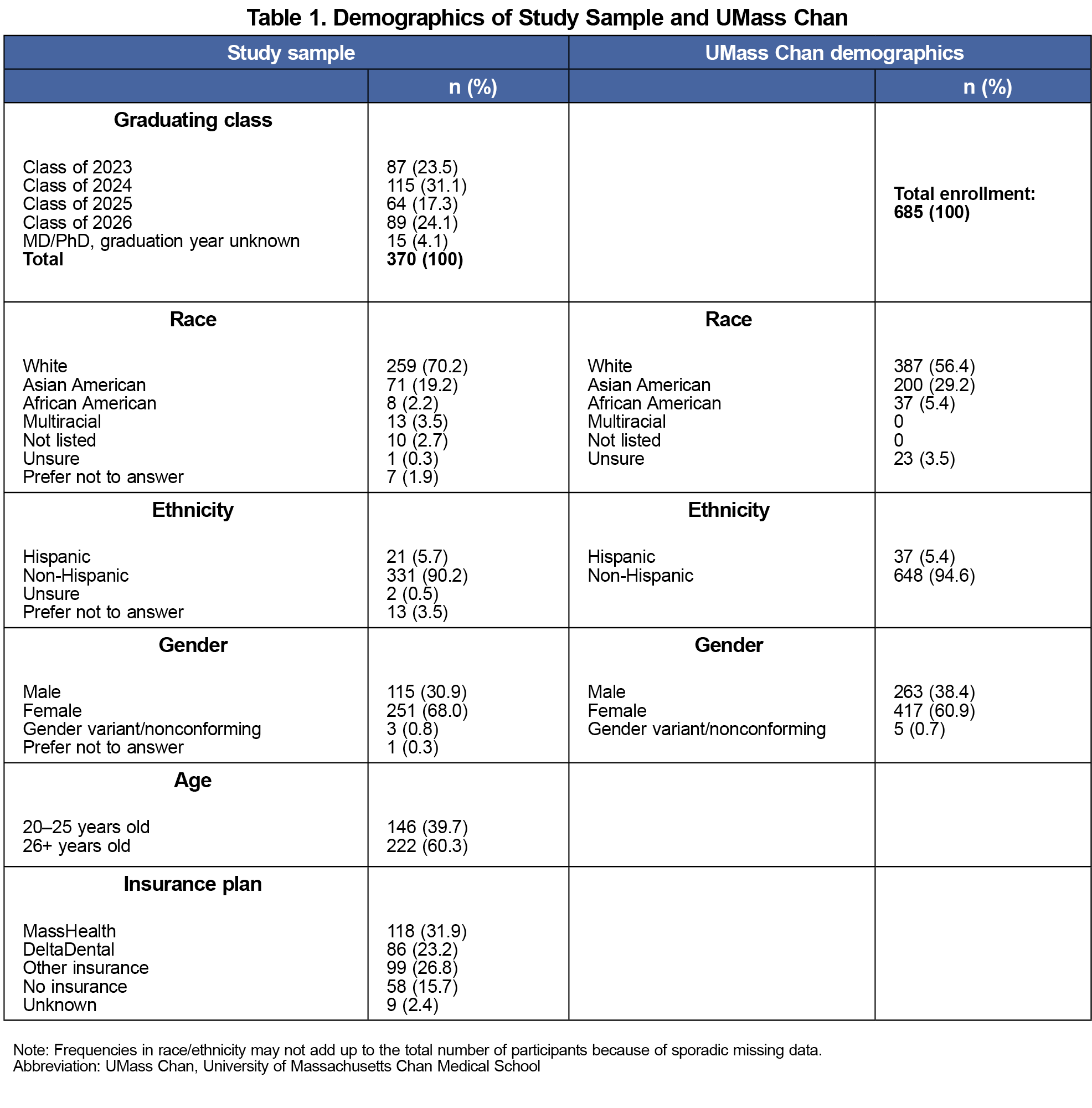
The study had a 54% response rate (370 of 685). All 370 participants completed at least 90% of questions. Demographics were consistent with the medical schools’ demographics (Table 1). The majority (84%) reported having dental insurance; one-third (31%) reported having MassHealth (Massachusetts Medicaid).
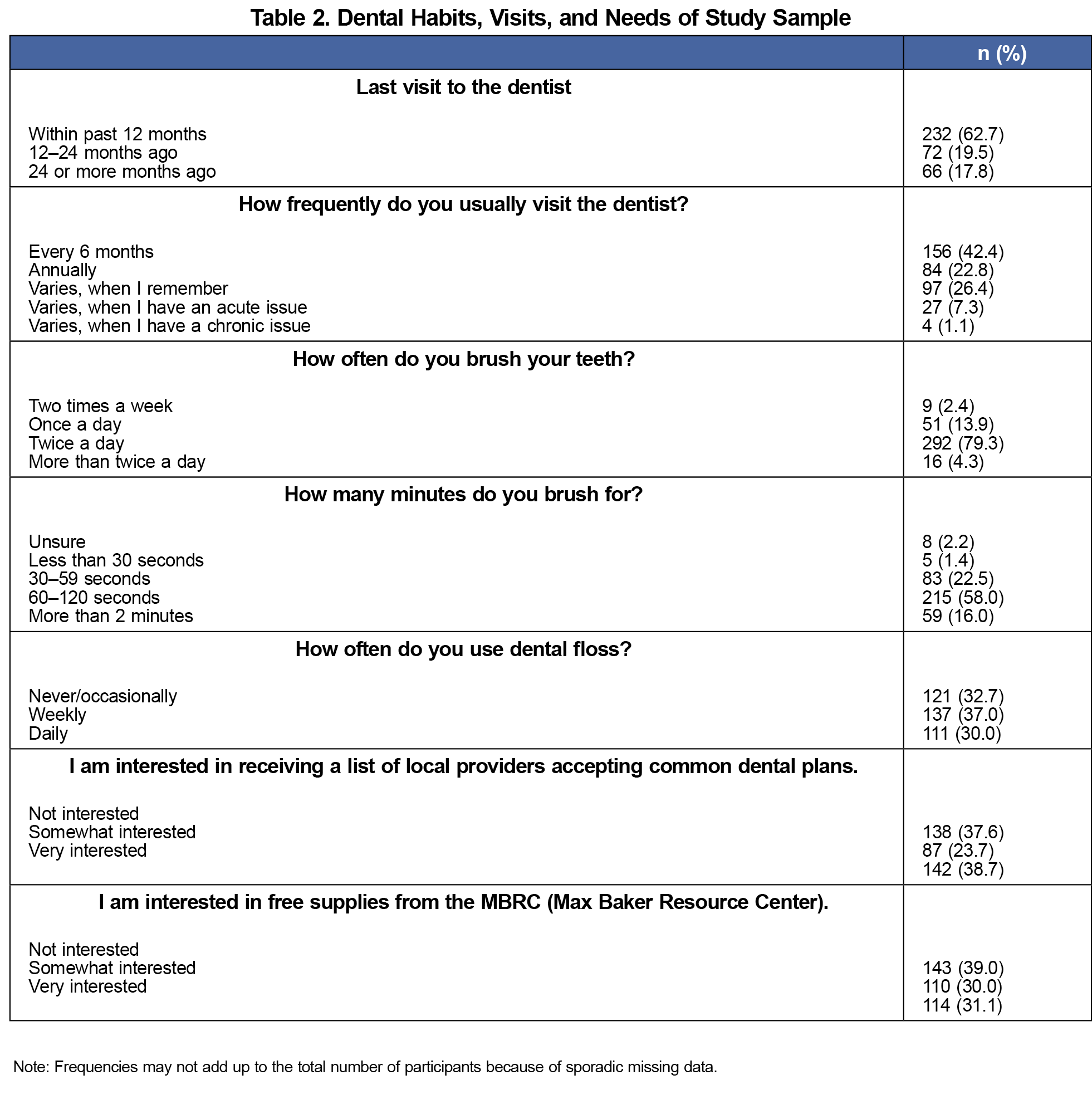
Nearly two-thirds (63%) of participants reported visiting a dentist within the past 12 months. Forty percent stated that they received dental care every 6 months (Table 2).
Regarding barriers to care, nearly one half (47%) reported being “too busy.” One-fifth (23%) stated they did not know how to find a dentist who accepted their insurance. Students enrolled in MassHealth (40%) had significantly more difficulty finding a provider compared to students with DeltaDental insurance (25%) or other private dental insurance (6%; ꭓ2=38.32; P<.001). Nearly one-fifth of participants (18%) reported financial barriers. Other barriers included limited time, fear of the dentist, difficulty finding a trustworthy provider, and visiting less due to self-pay. Only 6.8% reported no barriers.
Most students (84%) brushed their teeth at least twice a day for 60 to 120 seconds (58%). One-third (30%) flossed daily (Table 2).
Most students (62%) were interested in receiving a list of dentists who accepted common dental insurances. Many (61%) were interested in being supplied with free resources (eg, toothbrushes; Table 2).
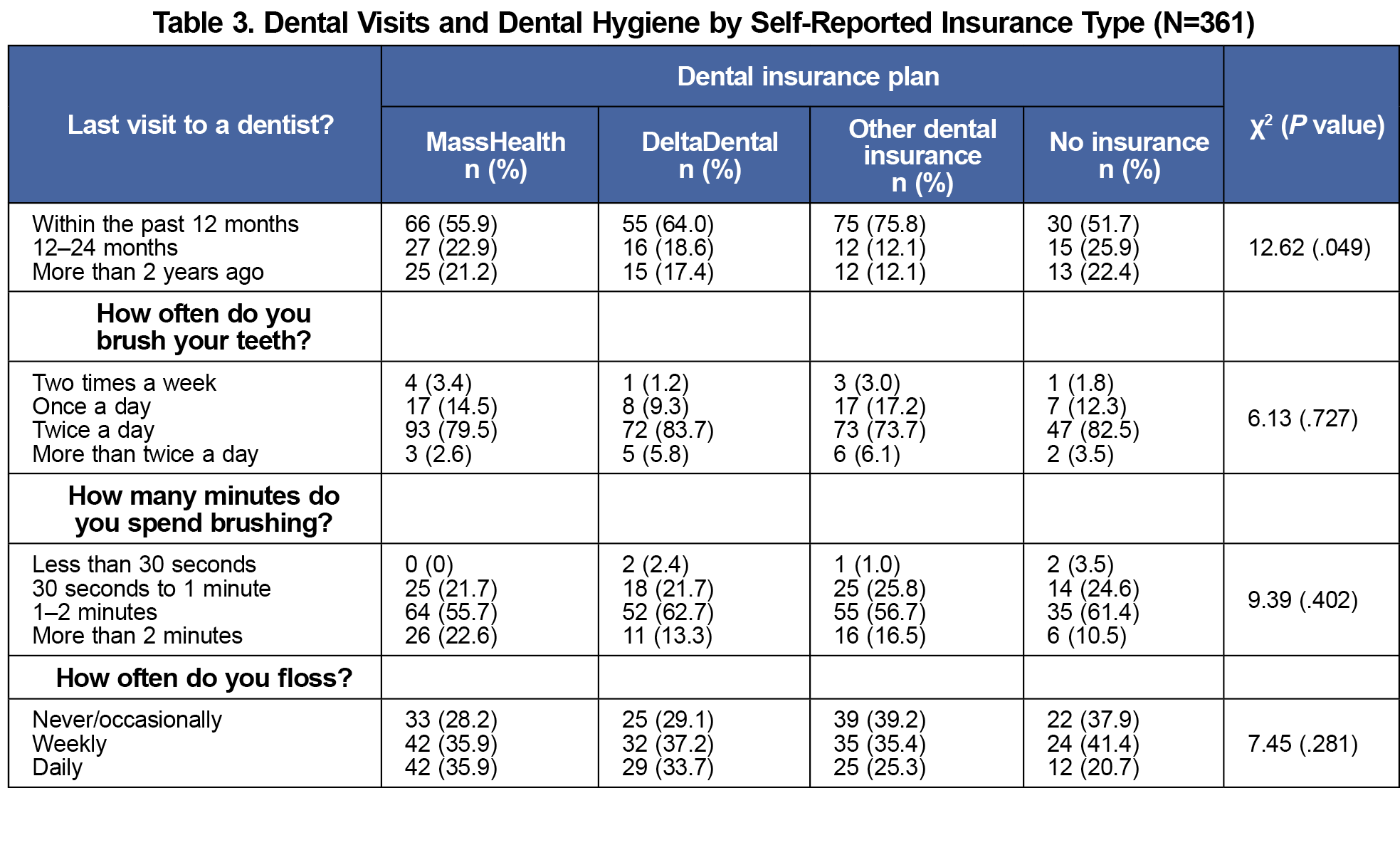
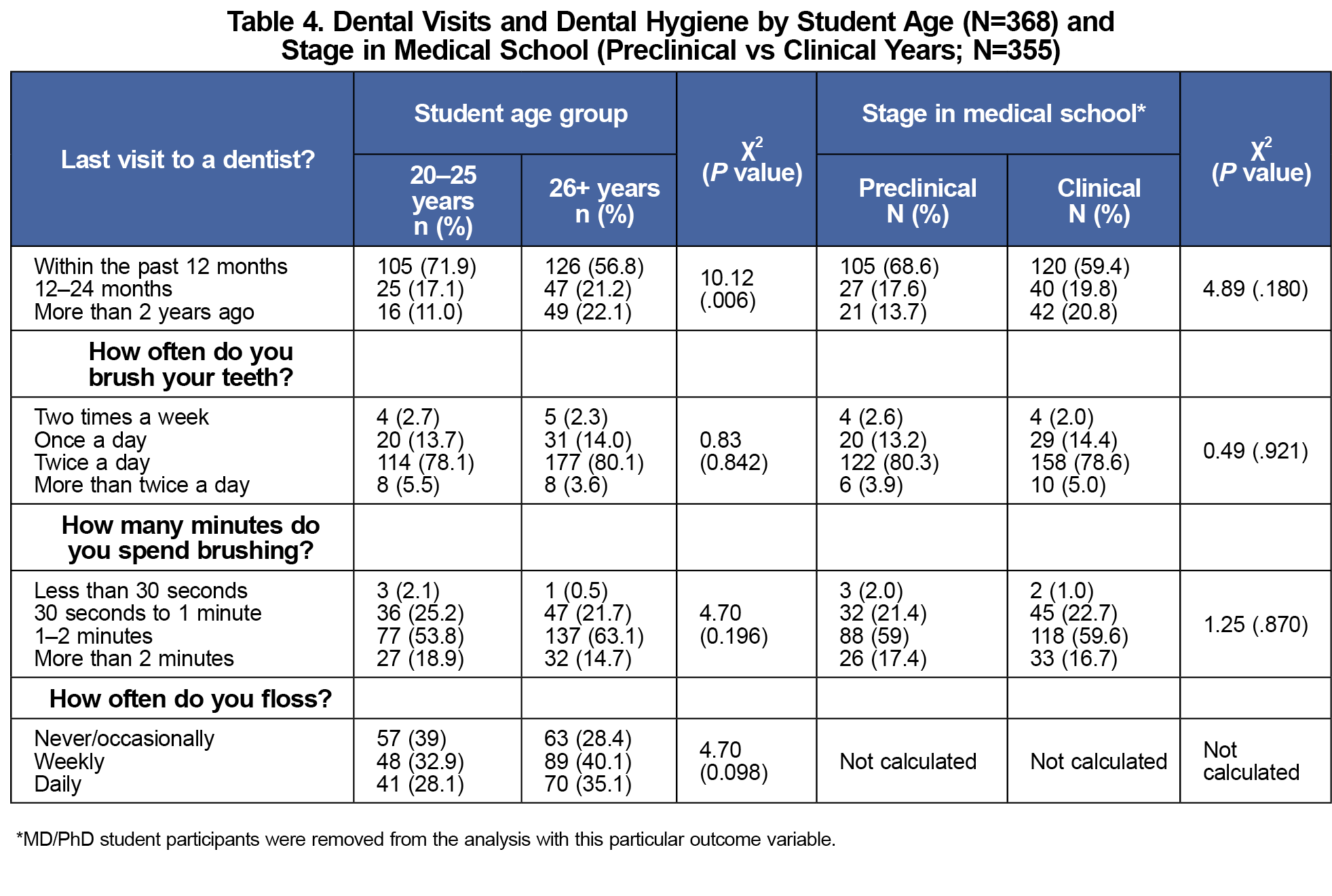
Approximately one-half of students with MassHealth (55%) reported visiting the dentist in the past 12 months, compared with 64% with DeltaDental and 75% with other private insurance (ꭓ2=12.62; P=.049; Table 3). Younger students (72% under age 26) were more likely to visit the dentist in the past year versus 57% of older students. Differences in the last dental visit between students in preclinical versus clinicalyears were not significant (Table 4).
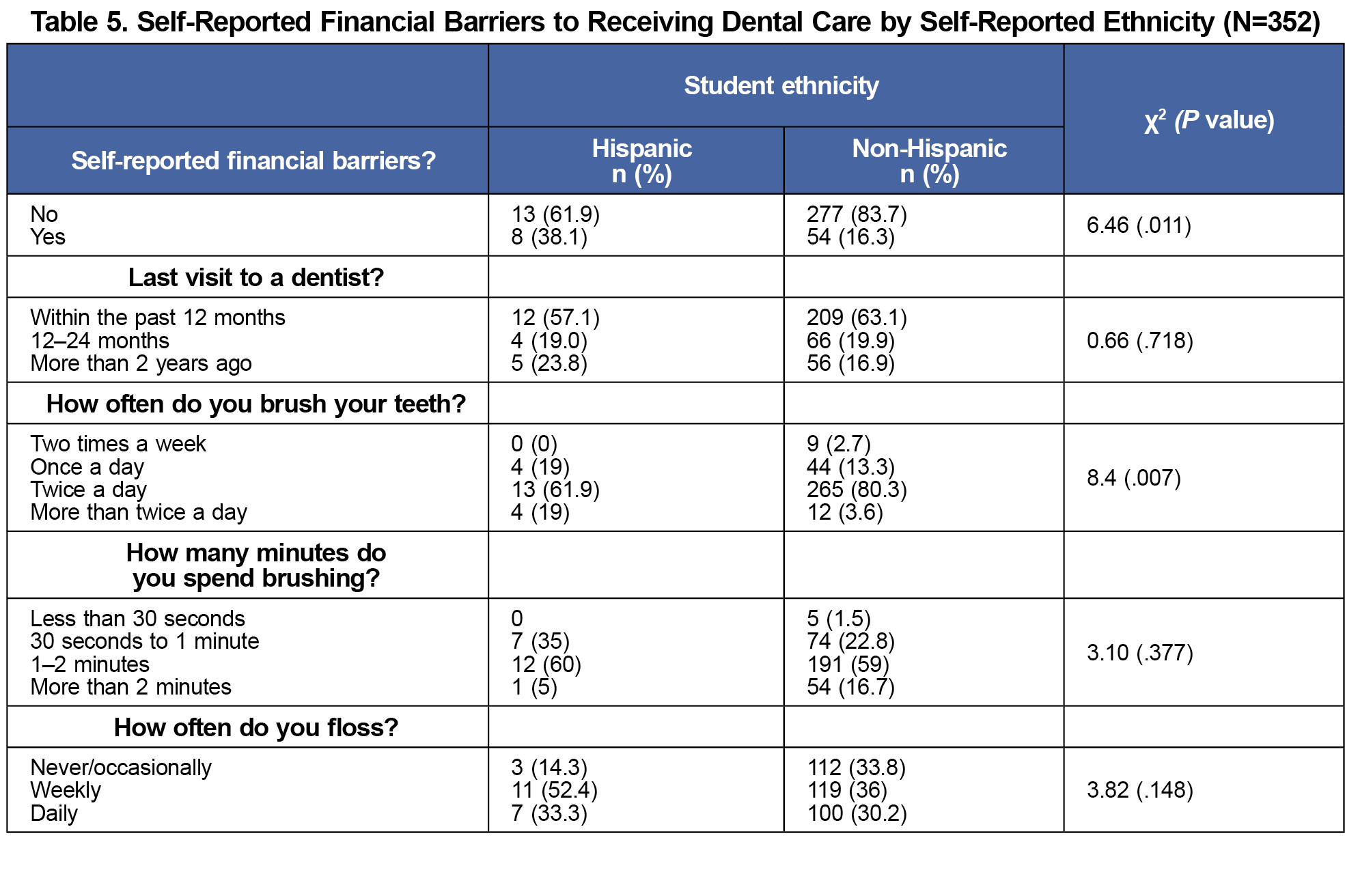
Nearly 60% of clinical students responded being “too busy” compared to 30% of preclinical students. We found no significant differences in personal dental hygiene practices by race or ethnicity. Hispanic students (38%) were more likely to report financial barriers to receiving dental care compared to non-Hispanic students (16%; ꭓ2=6.46; P=.011; Table 5).
DISCUSSION AND CONCLUSIONS
More UMass Chan medical students visited the dentist annually compared to medical students in the aforementioned Pennsylvania study (63% vs 50%) but less than college students in the national study (63% vs 76%).2,7 This finding may suggest that medical students have unique barriers compared to college students. These findings also align with medical schools in different states, potentially having different barriers to accessing dental care. Among older students who enrolled in Medicaid, students experienced state programs with different levels of coverage and different percentages of dentists who accepted Medicaid. With respect to time as a barrier, 78% of medical students in the Pennsylvania study noted lack of time while only 47% of UMass Chan students reported being too busy. At UMass Chan, students have 3 personal days in nonclinical years and 7 during clinical years, which may account for some of this discrepancy.
One possible solution to address time constraints could be adding an on-campus dental clinic within student health services; this was suggested by 15% of the Pennsylvania medical students. Providing students with a list of local dentists and insurances accepted could be helpful considering that two-thirds of UMass Chan students were interested in this resource. Moreover, because Hispanic students faced more financial barriers to accessing dental care, they might be offered additional health funds in their loan package.
Our study has some limitations. Our response rate was 54%, and we surveyed only one medical school. This limitation could impact generalizability of our findings. We also did not define the term “too busy.”
Clearly, students are reporting barriers to comprehensive oral care. UMass Chan could use our results to improve access to dental care. Future studies could evaluate whether these changes improve rates of dental visits. More studies are needed at a national level.
Acknowledgments
Financial Support: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- Roberts LW, Warner TD, Carter D, Frank E, Ganzini L, Lyketsos C; Collaborative Research Group on Medical Student Healthcare. Caring for medical students as patients: access to services and care-seeking practices of 1,027 students at nine medical schools. Acad Med. 2000;75(3):272-277. doi:10.1097/00001888-200003000-00019
- Pazzi C, Farrehi C, Capron M, Stillman M. Medical student health care: a single center pilot study of utilization and barriers. Discov Health Syst. 2024;3:8. doi:10.1007/s44250-024-00071-z
- Lin M, Griffin SI, Gooch, BF. Oral Health Surveillance Report: Trends in Dental Caries and Sealants, Tooth Retention, and Edentulism, United States: 1999–2004 to 2011–2016. Centers for Disease Control and Prevention; 2019. https://stacks.cdc.gov/view/cdc/82756
- Kotronia E, Brown H, Papacosta AO, et al. Oral health and all-cause, cardiovascular disease, and respiratory mortality in older people in the UK and USA. Sci Rep. 2021;11(1):16452. doi:10.1038/s41598-021-95865-z
- Meurman JH, Sanz M, Janket SJ. Oral health, atherosclerosis, and cardiovascular disease. Crit Rev Oral Biol Med. 2004;15(6):403-413. doi:10.1177/154411130401500606
- Friedewald VE, Kornman KS, Beck JD, et al; American Journal of Cardiology; Journal of Periodontology. The American Journal of Cardiology and Journal of Periodontology editors’ consensus: periodontitis and atherosclerotic cardiovascular disease. J Periodontol. 2009;80(7):1,021-1,032. doi:10.1902/jop.2009.097001
- Dewald L. Dental health practices in US college students: the American college health association-national college health assessment findings. J Health Dispar Res Pract. 2016;9(1):3.
- Crabtree R, Kirk A, Moore M, Abraham S. Oral health behaviors and perceptions among college students. Health Care Manag (Frederick). 2016;35(4):350-360. doi:10.1097/HCM.0000000000000124
- Hill MR, Goicochea S, Merlo LJ. In their own words: stressors facing medical students in the millennial generation. Med Educ Online. 2018;23(1):1530558. doi:10.1080/10872981.2018.1530558
- Glore SR, Walker C, Chandler A. Brief communication: dietary habits of first-year medical students as determined by computer software analysis of three-day food records. J Am Coll Nutr. 1993;12(5):517-520. doi:10.1080/07315724.1993.10718345
- Barbaresco S, Courtemanche CJ, Qi Y. Impacts of the Affordable Care Act dependent coverage provision on health-related outcomes of young adults. J Health Econ. 2015;40:54-68. doi:10.1016/j.jhealeco.2014.12.004
- Hinton E, Paradise J. Access to dental care in Medicaid: spotlight on nonelderly adults. Kaiser Family Foundation; March 17, 2016.https://www.kff.org/medicaid/issue-brief/access-to-dental-care-in-medicaid-spotlight-on-nonelderly-adults/
- Hill KB, Chadwick B, Freeman R, O’Sullivan I, Murray JJ. Adult dental health survey 2009: relationships between dental attendance patterns, oral health behaviour and the current barriers to dental care. Br Dent J. 2013;214(1):25-32. doi:10.1038/sj.bdj.2012.1176
- Sandilands D. Bivariate analysis. In: Michalos AC, ed. Encyclopedia of Quality of Life and Well-Being Research.Springer; 2014:416-418. doi:10.1007/978-94-007-0753-5_222



There are no comments for this article.