Introduction: With a critical primary care clinician shortage, team-based care (TBC) is under development to enhance access, especially in rural regions. However, there has been limited discussion about TBC from the patient’s perspective. We explored rural patient preferences for composition of their current and ideal primary health care team.
Methods: An anonymous online survey of rural residents was conducted within the Kootenay-Boundary region of British Columbia. The survey included demographic information and current and ideal health care team composition. Descriptive statistics were used.
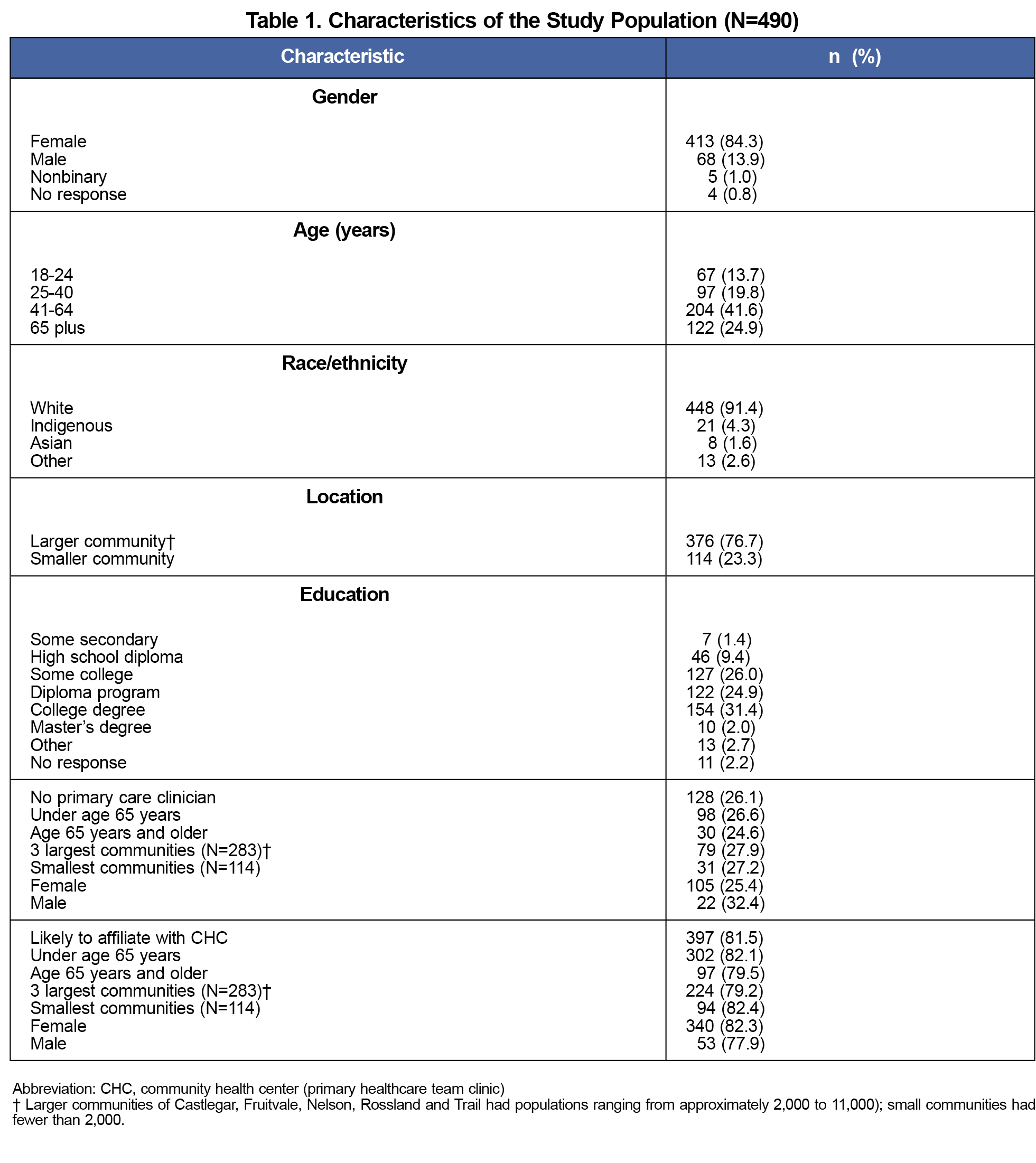
Results: Four hundred ninety individuals responded to the survey. Most respondents self-identified as female, were over age 40 years, White, and had a postsecondary school diploma. Those with a health care provider (n=362, 74%) included a primary care doctor (86.5%), alternative medicine practitioner (52.2%), allied health professional (35.4%), friends/family/support people (35.1%), specialist physician (30.1%) and nurse practitioner (18.5%) on their team. Ideal health care teams included a primary care physician (92.2%) followed by an alternative medicine practitioner (64.1%), allied health professionals (61.2%), specialist physician (59.8%), and nurse practitioner (54.8%). Almost half of all respondents (46.6%) chose five or more categories of team members and 43.7% chose 3-4 categories of members. Respondents (81.1%) were highly likely (49.6%) or likely (31.6%) to affiliate with a primary health care team clinic.
Conclusion: Both current and ideal health care team membership included many types of caregivers, with most respondents including three or more team-member categories. As many people in rural BC are without primary care providers, incorporating alternative medical practitioners and allied health professions into clinical teams within multidisciplinary settings could improve health care access.
With a critical primary care clinician shortage in British Columbia (BC),1 interdisciplinary and team-based care (TBC) can enhance health care through role flexibility, task delegation, and skills to overcome cultural barriers.2 TBC involves various providers from different fields of study or expertise that occupy distinct roles within a health care system and work together as a functional team, contributing to a shared goal of providing the best patient care.3 TBC can be provided within clinics or the larger community. In the Kootenay-Boundary (KB) region of BC, establishment of TBC within primary care practices began in 2018 to improve care quality and patient access to primary care. Benefits of TBC for patients include improved access, knowledge, ability to self-care, continuation and coordination of care, and overall health.4-6 For providers, TBC can create a more manageable workload.7
Concerns voiced about TBC and care models like Community Health Centers (CHCs) in Canada include system navigation and provider concerns about maintaining care quality and physician compensation, especially in fee-for-service models.8,9 In addition, introducing TBC often requires a systemic hierarchical shift between health care providers.10
Successful integration of TBC depends on creating the right mix of health care professionals and allied support persons within teams. However, little is known about the optimal composition of primary care teams from the patient’s perspective, and patients’ willingness to affiliate with team-based clinics like CHCs remains uncertain.11 The primary purpose of the study is to explore rural KB residents’ perceptions of their current and ideal primary health care team.
Three third-year rural premedicine students at Selkirk College conducted the survey as their rural health research project in collaboration with the KB Patient Advisory Committee and Community. The study was reviewed and approved by the Selkirk College Research Ethics Board (REB 2023-014).
Participants
The anonymous online survey was available to any KB resident 18 years or older for 6 weeks beginning in February 2024. Posters containing a QR code were placed in local businesses and anonymous paper surveys were available in the larger community libraries. Completed paper copies were placed in envelopes and given to the librarian for later collection.
Survey
The 15-question survey was hosted on a Google Forms platform. Survey questions included demographics, current access to a primary care provider (eg, with or without a family physician or nurse practitioner), participants’ current and ideal health care team composition, and willingness to affiliate with a CHC. Health care team members, both current and ideal, were selected from a list including the following categories: primary care physician, nurse practitioner, allied health professionals (eg, social worker, physical therapist), alternative medicine practitioners (eg, chiropractor, naturopath), family/friends/support people, specialist physician(s), situational (whoever is needed to help me get the health care that I need), religious advisor, Indigenous Elder, and other.
Data Analysis
We summarized data by categories and percentages. Having a family practitioner, current and ideal health care team, and willingness to affiliate with a CHC were examined by age, gender, and size of community (larger communities had 2,000 to 11,000 people and smaller communities <2,000).
Demographic Characteristics
The survey received 490 responses. Respondent demographics are shown in Table 1. Eighty-four percent self-identified as female, 66.5% were over age 40 years, 91.4% were White, and 61% had a postsecondary school diploma. About one-quarter (26.1%) did not have a family practitioner, with similar percentages by age category and size of community, but higher percentages reported for males (Table 1).
Health Care Team Membership
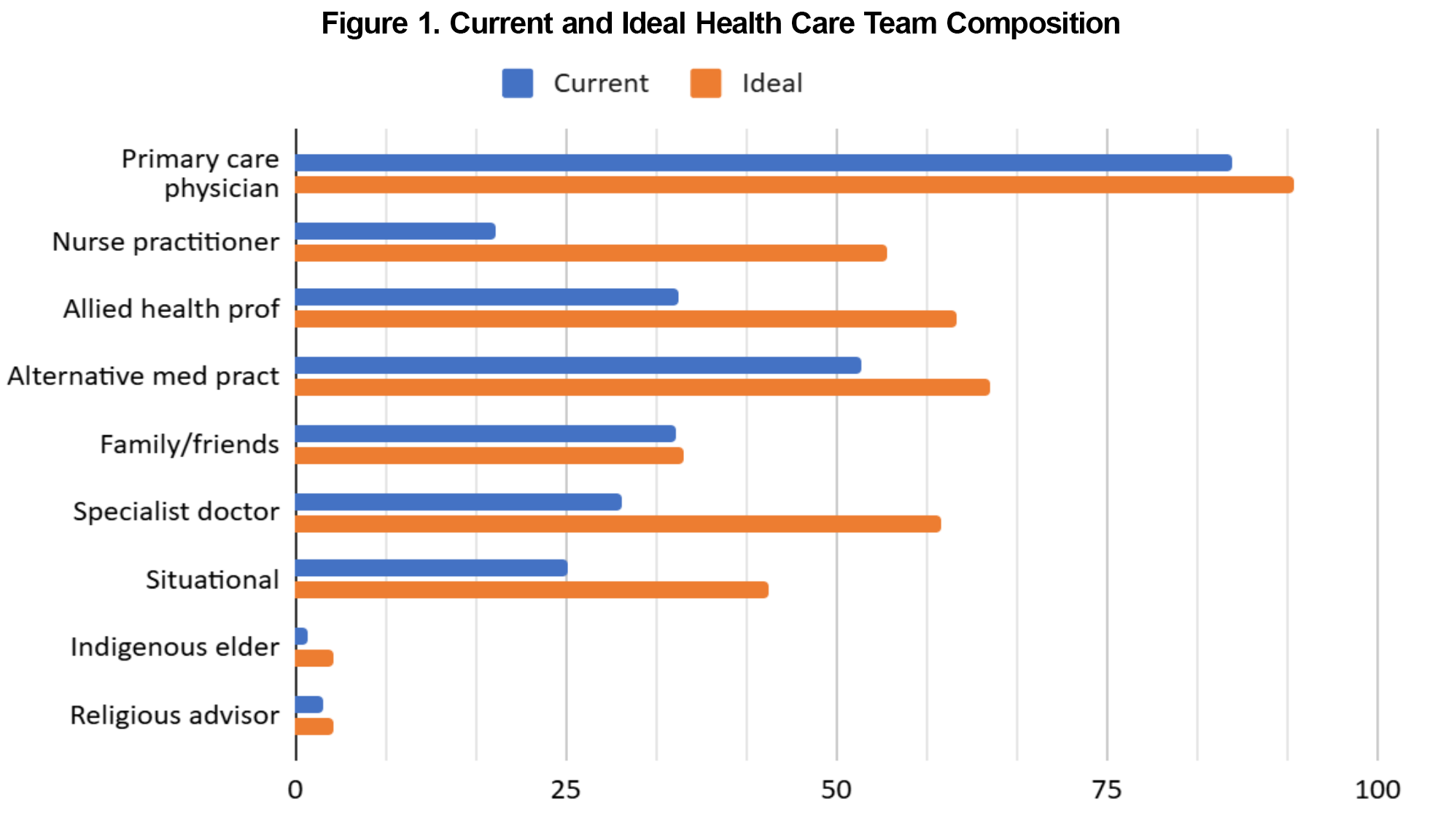
Categories of team members who currently make up one’s primary health care team and ideal health care team are shown in Figure 1. Of 362 respondents reporting on their current health care team (blue bars), 86.5% included a primary care physician followed by an alternative medicine practitioner (52.2%), allied health professionals (35.4%), friends/family/support people (35.1%), specialist physicians (30.1%) and nurse practitioner (18.5%). Other team members reported by one or twp respondents included dentists, pharmacists, and personal trainers. About one-quarter of respondents endorsed that their healthcare team was situational.
For the 487 respondents reporting their ideal health care team, nearly all (92.2%) included a primary care physician followed by an alternative medicine practitioner (64.1%), allied health professionals (61.2%), specialist physician (59.8%), and nurse practitioner (54.8%). For number of categories of ideal team members, 46.5% of respondents chose five or more followed by 43.7% choosing three or four categories of team members. Few (5.7%) wanted eight or more categories of team members and 3.9% choose only one or two for their ideal team.
Comparisions
Respondents ages 18-64 years were more likely than older respondents to choose only one or two team-member categories on their ideal team (15.8% vs 11.5%, respectively) and less likely to choose five or more categories of team members (37.2% vs 41.8%, respectively). Men (n=67) also chose fewer team-member categories for their ideal health care team (32.8% choosing one or two providers vs 11.2% for women). Those in the three largest communities (n=274) created smaller ideal teams (16.8% choose one or two categories vs 12.7% for those living in smaller communities and 36.5% choose five or more team member categories vs 46.9% from smaller communities).
Affiliation With Primary Health Care Team Clinic
Most of the 487 respondents reported being highly likely (49.6%) or likely (31.6%) to affiliate with a primary health care team clinic with over three quarters willing to affiliate by age, community size and gender (Table 1).
We found that both current and ideal healthcare team membership included many types of care givers, with most respondents including three or more team-member categories. Ideal teams included more nurse practitioners and allied health professionals. Inclusion of these practitioners within TBC could expand service delivery especially within colocated and/or care coordinated spaces such as CHCs,12 which was highly endorsed by our respondents. About one-half of current and ideal teams also included alternative medicine practitioners demonstrating patients’ preferences for other approaches to health and wellness. With about one in five Americans and Canadians experiencing chronic pain,13 incorporation of alternative medicine providers could support positive outcomes,14 and influence patient satisfaction and success of CHCs in rural areas. Given the reality of the Canadian context with too few family physicians and primary care nurse practitioners to empanel patients, primary care networks allow a shift toward a broader range of health care provider teams within and outside the walls of clinics that considers patient preference and availability. Expanding educational, leadership, and communication opportunities and providing change facilitators to learners and clinicians for optimizing team-based care could accelerate such collaborative practice and enhance access to care.15,16
Study Limitations
More women than men responded to the survey and users of alternative practitioners are more often women of higher education and/or income.17 This could bias results towards inclusion of these practitioners in TBC. However, as women make approximately 80% of health care decisions for their families,18 their opinions about health care teams might reflect who other family members would seek for care. More respondents also had higher education levels than the area population (college degree or higher: 38% vs 20.2% of households by regional 2021 Census data) which may have led to a greater interest in TBC among our respondents. In one Canadian study, education was positively associated with unmet healthcare need due to availability, particularly for those who received non-team-based vs TBC.19 Although most respondents were White, 95.9% of the KB population are mostly White.
In conclusion, respondent’s current health care team membership included primarily primary care physicians with just over half including alternative health providers and about one-third including allied health professionals and family/friends; three or more team-member categories made up their current team. Most respondent’s ideal teams also included nurse practitioners and specialists in addition to primary care physicians, alternative practitioners and allied health professionals. Taking rural patient preferences into consideration could expand access to care by actively incorporating alternative medical practitioners and allied health professions into clinical teams within multidisciplinary settings such as CHCs.
Acknowledgments
Financial support: The project was completed as a third-year community engagement project by the above students during their Rural Pre-Medicine program at Selkirk College, Castlegar, British Columbia and supported by the college.
Presentations: Results were presented to the Kootenay-Boundary (KB) Patient Advisory Committee and Community, the partnering organization, via Zoom web meeting in April 2023.
Conflict Disclosure: The authors have no conflicts of interest to declare.
References
- Li K, Frumkin A, Bi WG, Magrill J, Newton C. Biopsy of Canada’s family physician shortage. Fam Med Community Health. 2023;11(2):e002236. doi:10.1136/fmch-2023-002236
- Rygh EM, Hjortdahl P. Continuous and integrated health care services in rural areas. A literature study. Rural Remote Health. 2007;7(3):766. doi:10.22605/RRH766
- Cashman S, Reidy P, Cody K, Lemay C. Developing and measuring progress toward collaborative, integrated, interdisciplinary health care teams. J Interprof Care. 2004;18(2):183-196. doi:10.1080/13561820410001686936
- Newton C. It is time to invest in team-based care. Can Fam Physician. 2023;69(2):143. doi:10.46747/cfp.6902143
- Jesmin S, Thind A, Sarma S. Does team-based primary health care improve patients’ perception of outcomes? Evidence from the 2007-08 Canadian Survey of Experiences with Primary Health. Health Policy. 2012;105(1):71-83. doi:10.1016/j.healthpol.2012.01.008
- Szafran O, Kennett SL, Bell NR, Green L. Patients’ perceptions of team-based care in family practice: access, benefits and team roles. J Prim Health Care. 2018;10(3):248-257. doi:10.1071/HC18018
- Hui D, Hannon BL, Zimmermann C, Bruera E. Improving patient and caregiver outcomes in oncology: Team-based, timely, and targeted palliative care. CA Cancer J Clin. 2018;68(5):356-376. doi:10.3322/caac.21490
- Longhurst A, Cohen M. The importance of community health centres in BC’s primary care reforms: what the research tells us. Canadian Centre for Policy Alternatives. March 2019. Accessed January 8, 2025. https://www.researchgate.net/publication/336867950.
- Primary care networks in Ontario health teams: guidance document. January 2024. Accessed January 8, 2025. https://www.ontario.ca/files/2024-01/moh-primary-care-networks-guidance-en-2024-01-23.pdf.
- Howard J, Miller WL, Willard-Grace R, et al. Creating and sustaining care teams in primary care: perspectives from innovative patient-centered medical homes. Qual Manag Health Care. 2018;27(3):123-129. doi:10.1097/QMH.0000000000000176
- Takach M, Buxbaum J. Care management for Medicaid enrollees through community health teams. The Commonwealth Fund. May 21, 2013. . Accessed January 8, 2025.https://www.commonwealthfund.org/publications/fund-reports/2013/may/care-management-medicaid-enrollees-through-community-health
- Hanson C. Evidence Brief, Government of Canada, August 2022. Here today, gone tomorrow: public transportation and vulnerabilities in rural and remote Canada. Accessed January 8, 2025. https://www.criaw-icref.ca/wp-content/uploads/2022/02/Here-Today-Gone-Tomorrow-Final-Report.pdf
- Rikard SM, Strahan AE, Schmit KM, Guy GP Jr. Chronic pain among adults - United States, 2019–2021. MMWR Morb Mortal Wkly Rep. 2023;72(15):379-385. doi:10.15585/mmwr.mm7215a1
- Urits I, Schwartz RH, Orhurhu V, et al. A comprehensive review of alternative therapies for the management of chronic pain patients: acupuncture, tai chi, osteopathic manipulative medicine, and chiropractic care. Adv Ther. 2021;38(1):76-89. doi:10.1007/s12325-020-01554-0
- Shrivastava S, Martinez J, Coletti DJ, Fornari A. Interprofessional leadership development: role of emotional intelligence and communication skills training. MedEdPORTAL. 2022;18:11247. doi:10.15766/mep_2374-8265.11247
- LaMothe J, Hendricks S, Halstead J, Taylor J, Lee E, Pike C, Ofner S. Developing interprofessional collaborative practice competencies in rural primary health care teams. Nurs Outlook. 2021 May-Jun;69(3):447-457. 2020 Dec 29. doi:10.1016/j.outlook.2020.12.001
- Canizares M, Hogg-Johnson S, Gignac MAM, Glazier RH, Badley EM. Changes in the use practitioner-based complementary and alternative medicine over time in Canada: cohort and period effects. PLoS One. 2017;12(5):e0177307. doi:10.1371/journal.pone.0177307
- Matoff-Stepp S, Applebaum B, Pooler J, Kavanagh E. Women as health care decision-makers: implications for health care coverage in the United States. J Health Care Poor Underserved. 2014;25(4):1507-1513. doi:10.1353/hpu.2014.0154
- Zygmunt A, Asada Y, Burge F. Is team-based primary care associated with less access problems and self-reported unmet need in Canada? Int J Health Serv. 2017;47(4):725-751. doi:10.1177/0020731415595547



There are no comments for this article.