Mood alone can affect an individual’s weight and eating habits.1 Additionally, the Centers for Disease Control and Prevention has estimated obesity prevalence to be higher than 20% in the United States, meaning more than one in five adults are affected by obesity.2 Similarly, a 2020 study showed that 18.4% of adults in the United States are diagnosed with depression.3 One effective treatment for obesity or depression is cognitive behavioral therapy (CBT) for that specific disorder.4-6 This study aimed to explore whether CBT, when used exclusively to treat depression and without concurrent weight management interventions, leads to changes in body mass index (BMI). Given the multifaceted nature of weight change, influenced by factors such as exercise and medication, this retrospective analysis sought to isolate the effects of CBT on BMI in patients undergoing treatment solely for depression.
LEARNER RESEARCH
The Impact of Cognitive Behavioral Therapy on Body Mass Index in Patients Treated Exclusively for Depression
Shawn Y. Sunu, DO, MS | Jason R. Woloski, MD
PRiMER. 2025;9:31.
Published: 6/24/2025 | DOI: 10.22454/PRiMER.2025.921088
Introduction: Mood can affect an individual’s weight and eating habits, making cognitive behavioral therapy (CBT) a potential approach to improving body mass index (BMI). Nevertheless, analyzing weight change is complex due to other factors, such as exercise and medications. This retrospective study examines BMI changes in depressed patients undergoing CBT exclusively for depression, not weight management.
Methods: A retrospective study compared BMI changes between a CBT group and a no CBT group of depressed patients at an academic medical center in central Pennsylvania. To minimize variability, participants were matched one-to-one for gender, age at diagnosis, and BMI at diagnosis. Both groups were followed from the initial psychology visit to the completion of CBT in the experimental group.
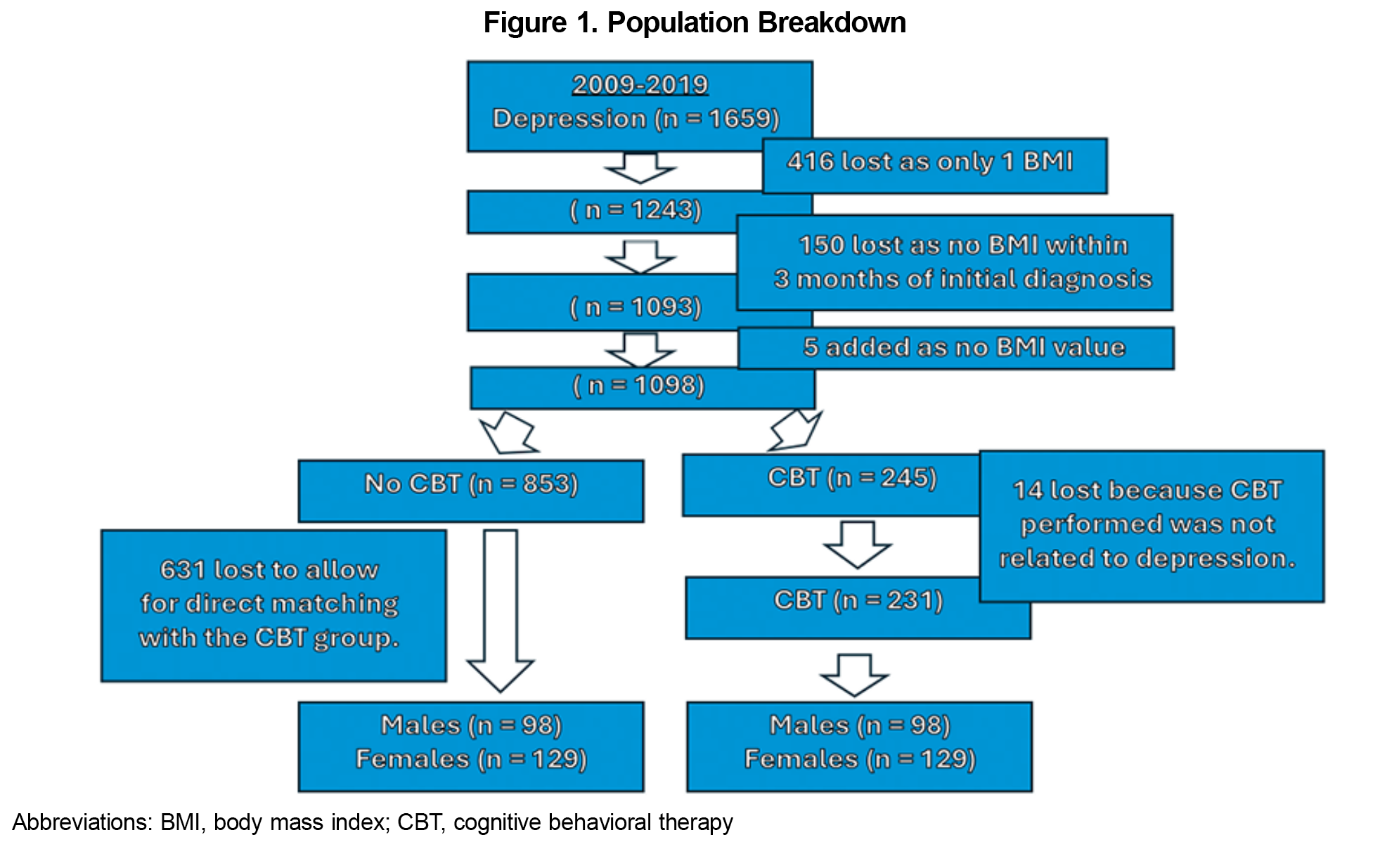
Results: From 2009 to 2019, 1,659 people were diagnosed with depression, but only 231 underwent CBT for depression. The CBT group had a slightly higher BMI at baseline (BMI=35.7 vs BMI=34.6). Among controls (no CBT), 9.2% were on Medicaid compared to only 1.3% in the experimental group. Overall, neither group showed a median difference in BMI during the study period.
Conclusions: CBT alone did not significantly impact BMI when used exclusively for depression without additional weight-loss interventions. A secondary finding was the apparent underutilization of CBT among those with depression. Future research should explore barriers to CBT access in the depressed population.
Inclusion criteria were adult patients (18 years and older) within a large academic health system in central Pennsylvania who had a new diagnosis of depression, a concurrent diagnosis of obesity, and completion of CBT for depression within the same institution from 2009 to 2019. Exclusion criteria included those with CBT visits initiated before the designated time frame, those with initiation of CBT more than a year prior, those with antidepressant medication use less than 1 year, and those taking medications with weight loss potential concurrently during the study.
Propensity scores (predicted probability being in the CBT group) were estimated for patients with depression and used to match CBT patients to no CBT patients. Using logistic regression, the model included age at depression, diagnosis, sex, and BMI at depression diagnosis. Matching was determined within a caliper of 0.25 time the standard deviation of the propensity score. We achieved a total of 227 matched pairs. We calculated descriptive statistics, including mean, standard deviations, medians, and interquartile ranges for continuous variables, and frequency and percentages for categorical variables. For continuous variables, we performed a Wilcoxon signed rank test due to abnormal distribution of the data. For categorial variables, we used McNemar tests.
We applied a multivariable approach using a generalized linear model with a lognormal distribution to estimate the least square means for both the cases and controls, helping to account for better control of potential confounding variables. For the difference in BMI, a constant value had to be applied to make all values positive and then back transformed for the least square means estimates. Models were adjusted for the use of antidepressants and the number of CBT visits. For the control group, the number of CBT visits was zero for all patients. Additionally, Type 3 tests of fixed effects are presented to show significance of CBT status, use of antidepressants, and number of CBT visits on the outcomes.
All statistical analyses were conducted in SAS Enterprise Guide version 8.2 (SAS Institute Inc). The Geisinger Health System Institutional Review Board (IRB# 2021-0878) approved this study.
A total of 1,659 individuals were diagnosed with depression, but only 245 (16.3%) of those underwent CBT. Of the 245 patients in the experimental group, 14 were removed because they underwent CBT that was not related to depression (Figure 1).
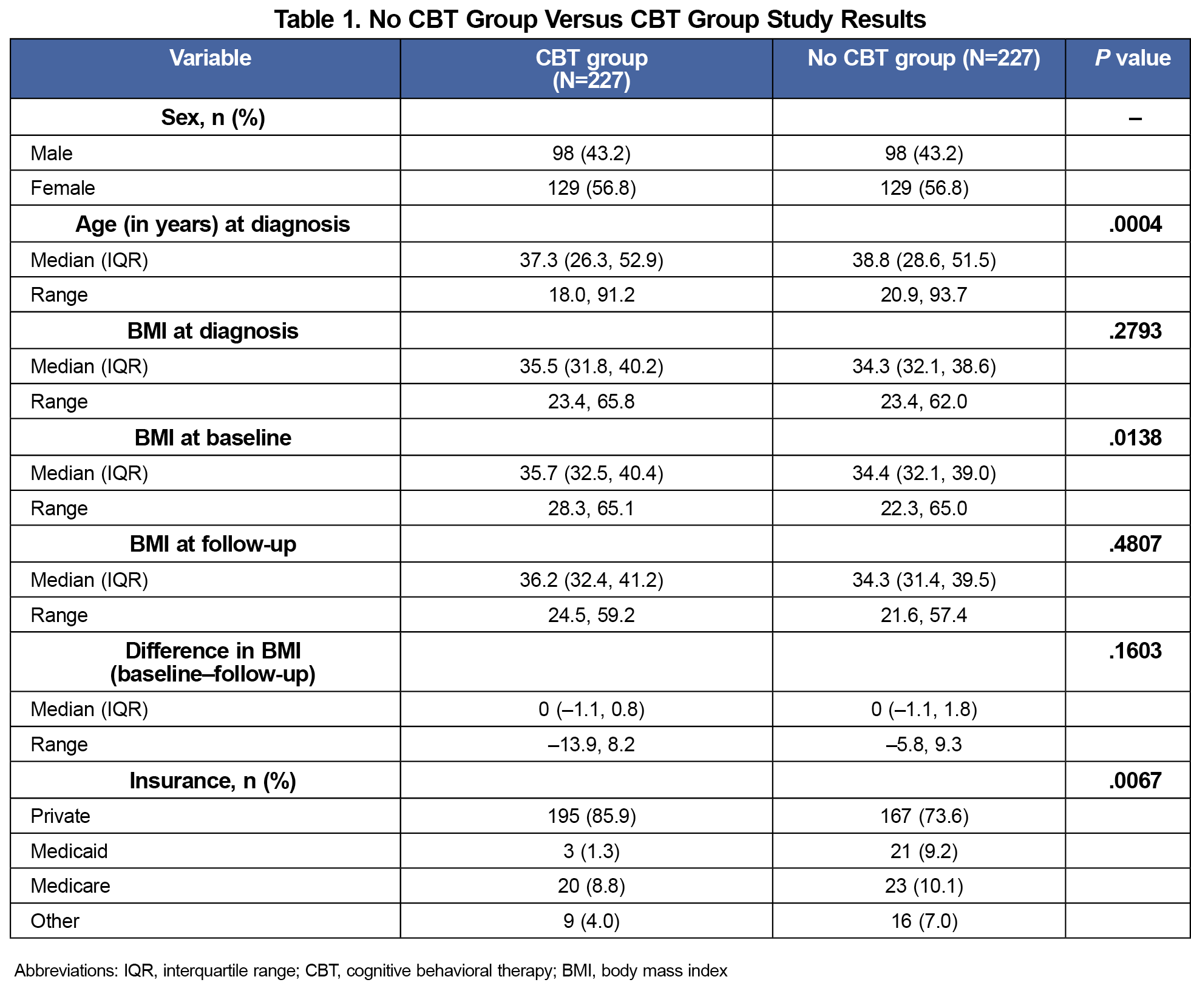
When comparing the 227 in the no CBT group versus the CBT group, the median BMI for the CBT group was slightly higher than the no CBT group at the start of therapy (CBT group BMI of 35.7 vs no CBT group BMI of 34.3; P value .0138). The median difference between the no CBT group versus the CBT group showed no statistical difference in BMI (no CBT group BMI difference 0 vs CBT group BMI difference 0; P value .1603). However, the range of changes in BMI of the CBT group varied more than the no CBT group (no CBT group –5.8±9.3 vs CBT group –13.9±8.2). Lastly, of the 227 in the CBT group, 195 (85.9%) were privately insured, but only 3 (1.3%) were on Medicaid compared to the 21 (9.2%) in the no CBT group. A breakdown of the results can be seen in Table 1.
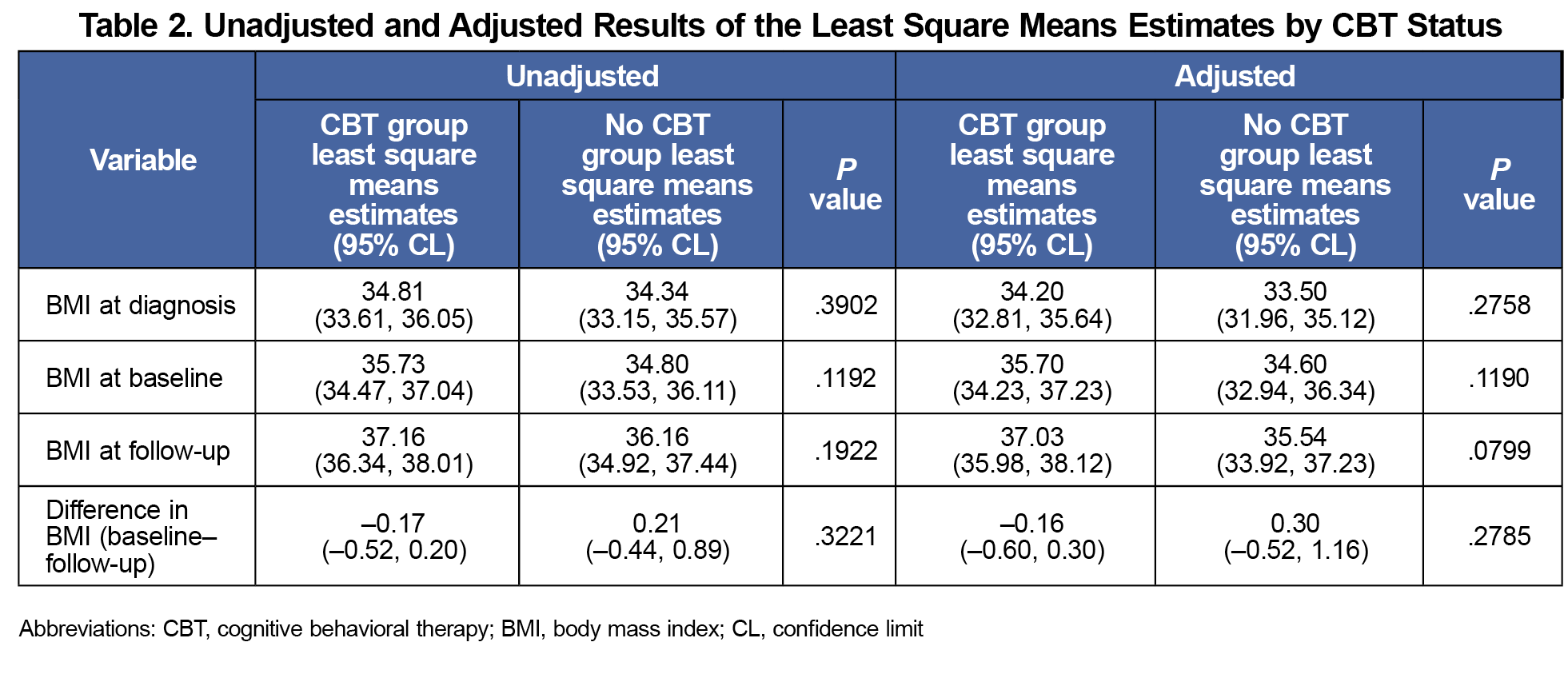
Via the adjusted least square mean estimates, we still found no statistical difference between the CBT group and no CBT group at diagnosis (CBT group BMI 34.81 vs no CBT group BMI 34.34; P value .3902) or the difference in BMI at the end of the study (CBT group BMI difference –0.16 vs no CBT group BMI difference 0.30; P value .2784; Table 2). The BMI at baseline was still noted to be slightly higher with the CBT group than the no CBT group, but not of significance given the P value (CBT group BMI 35.7 vs no CBT group 34.6; P value .1190).
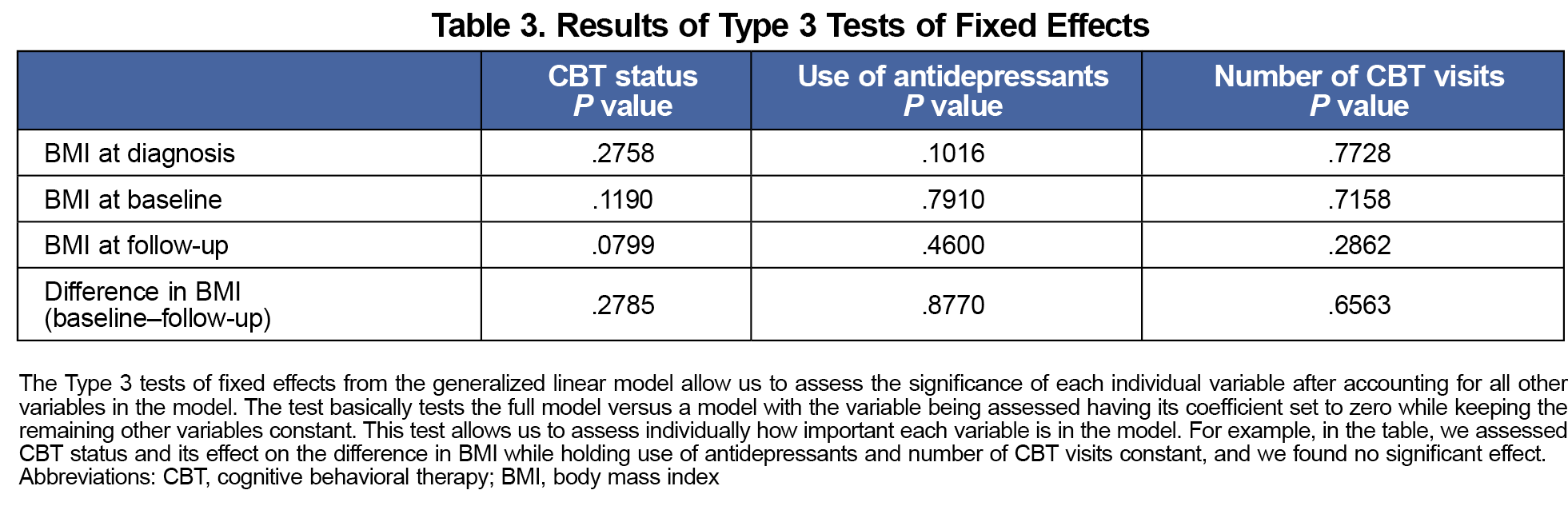
The use of antidepressants (P value .8770) or the number of CBT visits (P value .6563) did not have a significant impact on BMI change over the course of the study (Table 3).
The limited number of CBT visits highlights the underutilization of CBT, despite well-established benefits.5 Additionally, a significantly smaller proportion of those who received CBT were covered by Medicaid, suggesting that insurance type may impact CBT access.
Results indicated that individuals with a higher BMI were more likely to undergo CBT. However, our study was not designed to assess this correlation, and numerous confounding variables were not accounted for. Investigation of this potential relationship may provide valuable insights in future studies.
Another limitation of our study was the inability to access patient records for individuals who received CBT outside the studied hospital system. This constraint highlights the need for further studies to explore barriers to data sharing in the electronic record.
For those who underwent CBT exclusively for depression, we found no significant difference in BMI compared to those who did not receive CBT for depression. These findings suggest that CBT, when not directly addressing obesity, does not significantly impact BMI. Clinically, this finding underscores the importance of ensuring that therapy referrals explicitly specify all relevant diagnoses to optimize therapeutic outcomes. However, our study did not specifically examine the potential differences between individuals who received CBT for depression alone versus those who received CBT for both depression and obesity.
Acknowledgments
The authors thank the Gesinger research core and biostatistics team.
Financial Support: Financial support for this study was provided by Geisinger’s Internal Research Core Services
Presentations: This study was presented at the Pennsylvania Academy of Family Physicians Research Day, April 22, 2023, in Tannersville, Pennsylvania.
References
- Frayn M, Knäuper B. Emotional eating and weight in adults: a review. Curr Psychol. 2018;37(4):924-933. doi:10.1007/s12144-017-9577-9
- Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Nutrition, Physical Activity, and Obesity. Adult obesity prevalence maps. CDC; September 21, 2023.
- Lee B, Wang Y, Carlson SA, et al. National, state-level, and county-level prevalence estimates of adults aged ≥18 years self-reporting a lifetime diagnosis of depression—United States, 2020. MMWR Morb Mortal Wkly Rep. 2023;72(24):644-650. doi:10.15585/mmwr.mm7224a1
- Comșa L, David O, David D. Outcomes and mechanisms of change in cognitive-behavioral interventions for weight loss: a meta-analysis of randomized clinical trials. Behav Ther Res. 2020;132:103654. doi:10.1016/j.brat.2020.103654.
- Jacob A, Moullec G, Lavoie KL, et al. Impact of cognitive-behavioral interventions on weight loss and psychological outcomes: a meta-analysis. Health Psychol. 2018;37(5):417-432. doi:10.1037/hea0000576
- Fennell M. Cognitive behaviour therapy for depressive disorders. In: Gelder M, Andreasen N, Lopez-Ibor J, Geddes J, eds. New Oxford Textbook of Psychiatry.Oxford University Press; 2012:1,305-1,313. doi:10.1093/med/9780199696758.003.0167
Lead Author
Shawn Y. Sunu, DO, MS
Affiliations: Geisinger Kistler Family Medicine Residency, Wilkes-Barre, PA
Co-Authors
Jason R. Woloski, MD - 1Geisinger Kistler Family Medicine Residency, Wilkes-Barre, PA
Corresponding Author
Shawn Y. Sunu, DO, MS
Correspondence: Geisinger Kistler Family Medicine Residency, Wilkes-Barre, PA
Email: sysunu7@gmail.com
Fetching other articles... 
Loading the comment form... 
Submitting your comment... 


There are no comments for this article.