The issue of medical students' attitudes toward pursuing a career in family medicine (FM) is critical in addressing current and future health care challenges such as aging populations, complex health care needs, and the shortage of health care professionals.1 Previous research has identified several factors influencing medical students' specialty choices, including rural background, interest in underserved care, lower income expectations, and exposure to FM clerkships.2 Conversely, aspirations for higher income, prestige, and a research-oriented career have been negatively associated with interest in FM.2 In Japan, factors such as interest in clinical reasoning, community-oriented practice, and involvement in preventive care have been linked to a preference for FM.3 However, there is limited research on Japanese medical students' views on FM careers and the barriers to choosing FM as a career. This study aims to fill this gap by identifying Japanese medical students' perspectives on FM and comparing them with those of medical students in China where FM has successfully been promoted by major primary health care reform. We believe that comparing two countries with similar cultures and circumstances yet demonstrating different outcomes regarding the promotion of FM could provide insights that are applicable to the promotion of FM on an international scale.
RESEARCH BRIEF
Medical Students' Views on Family Medicine in Japan: Insights From an International Comparison
Yuki Takeuchi, MD | Qi Chen, PhD | Michael D. Fetters, MD, MPH, MA (deceased)
PRiMER. 2025;9:10.
Published: 3/26/2025 | DOI: 10.22454/PRiMER.2025.358588
Introduction: Promoting family medicine (FM) among medical students is essential for strengthening future primary care systems. This study examines Japanese medical students' perspectives on FM and compares them with findings from an identical study conducted in China to identify effective strategies for promoting FM.
Methods: A cross-sectional, self-administered, online survey was conducted from November 2020 to February 2021, involving 438 medical students across 28 medical schools in Japan. The survey, modeled after an identical study in China, assessed career decision factors, perceptions of FM careers and lifestyles, and attitudes toward FM, using a 5-point Likert scale.
Results: Of the 363 respondents who indicated a preferred specialty, 19.8% selected FM, making it the second most popular choice. Japanese medical students valued social commitment, manageable work hours, and career stability but perceived FM as less prestigious compared to medical students in China. Both groups recognized the importance of FM in rural health care and the role of government support. However, Japanese medical students were less optimistic about FM careers offering good income and work-life balance.
Conclusion: While FM is relatively popular among medical students in Japan, challenges such as perceptions of low prestige and poor work-life balance remain. Addressing these issues might enhance interest in FM. Study limitations include response bias, cultural differences affecting generalizability, and differences in timing of the survey and participant grade levels between studies. Future research should address these limitations and further explore cultural influences on medical students' career decisions.
Family Medicine in Japan and China
In Japan, primary care has traditionally been provided by hospital-trained physicians.4 FM was recently recognized as an independent discipline, with the Japan Primary Care Association introducing the first family medicine board certification in 2009. As of December 31, 2022, there were 1,126 board-certified family physicians (FPs), representing 0.3% of all registered medical doctors (339,623) in Japan.5,6 In contrast, the Chinese government implemented extensive primary health care reforms, rapidly increasing the number of FPs from 32,400 to 309,800 between 2009 and 2018. These reforms included the establishment of 559 hospital-based and 1,660 community-based training programs, the creation of multiple pathways to becoming an FP, and the integration of FM curricula into medical education.7
Study Design
We conducted a cross-sectional, self-administered, online survey from November 2020 to February 2021. The survey aimed to elucidate the characteristics of Japanese medical students by comparing results with an identical study conducted in China in 2016.8 The study received approval from the research ethics committee of Teine Keijinkai Hospital (ID 4-019182-00), and all participants provided online consent before starting the survey.
Participants
The study sample consisted of 438 medical students, ranging from first to sixth year, from 28 medical schools across Japan. The survey was distributed via the mailing lists of each medical school, making it impossible to accurately calculate the response rate. In the online survey, all mandatory questions, except for the optional question regarding preferred specialties, were required to be answered prior to submission. Consequently, all submitted responses were included in the analysis without the application of any exclusion criteria. By contrast, the identical online survey conducted in China by the senior authors (Q.C. and M.D.F.) in 2016 (during the “Introduction to Medicine” lecture for 347 first-year students at Peking University Health Science Center), required all questions including the one regarding preferred specialties, to be answered prior to submission. A total of 335 students completed the Chinese survey.
Data Collection Tools
We used a survey instrument initially administered to medical students in China in 2016,8 developed based on Wright et al's research.9 Our survey included one question about preferred specialty and 45 items with 5-point Likert-scale responses, covering career decision factors, FPs’ lifestyle and career, and attitudes toward FM. To improve response quality by reducing completion time, we excluded 14 questions related to preferred medical settings and patient age groups from the Japanese survey. Additionally, we removed two lifestyle-related questions that could suggest gender role stereotypes. Both the Chinese and the Japanese surveys were administered online, using Google Forms in Japan and the university's original online application in China. Participation was voluntary and anonymous in both studies.
Translation
The original English-language survey was translated into Japanese by bilingual investigators, with translation difficulties resolved through discussions among the translators and two other bilingual family physicians. The same method was used for translation from English to Chinese in the identical study. The instrument was pilot tested with three medical students.
Data Analysis
Using Easy R software (EZR V. 1.55), we conducted a Mann-Whitney U test for scores on the 5-point Likert scale to compare the Japanese and Chinese groups. In the identical survey, we used SPSS 21.0 software (IBM Corp, Armonk, NY) for independent-sample t test between the scores of Chinese and international students. However, given that the Likert scale data in this study were ordinal and their distribution was unknown, we chose the Mann-Whitney U test as the method of analysis.
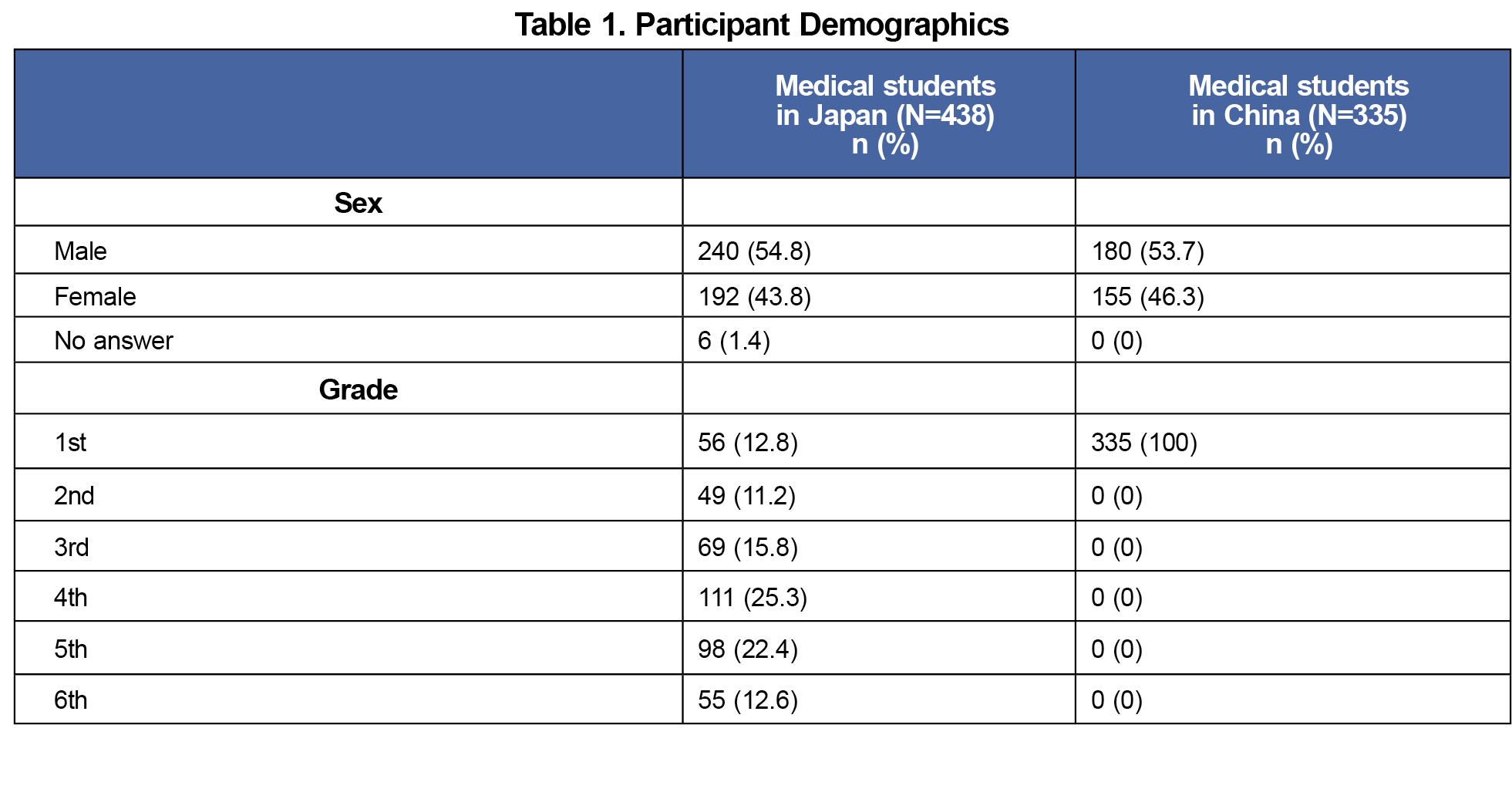
Participants
We received responses from 438 Japanese medical students and compared them with responses from 335 first-year medical students who participated in the identical survey conducted in China in 2016.8 The demographics of participants are shown in Table 1.
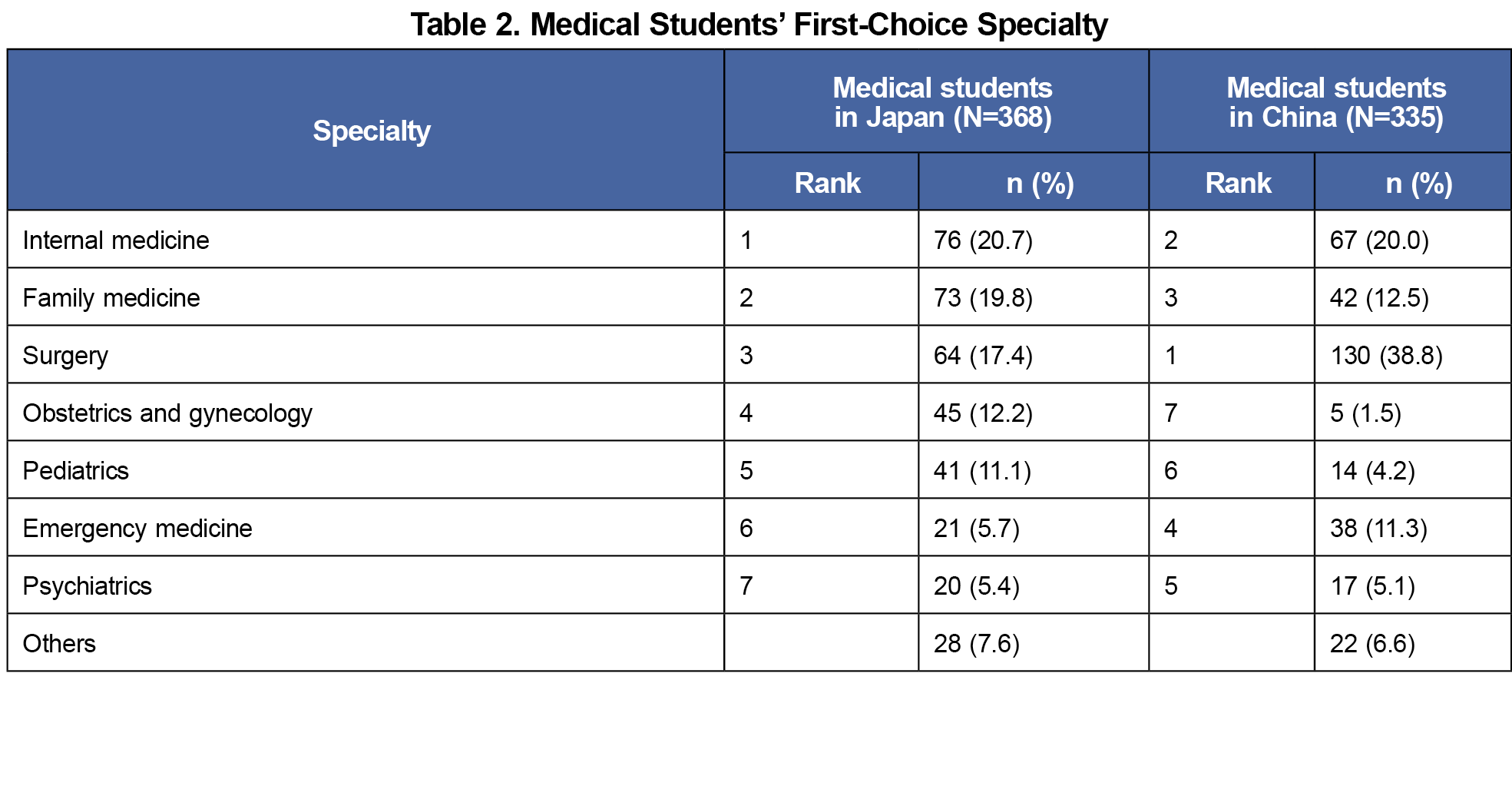
Preferred Specialty
Among the 363 Japanese medical students who indicated their preferred specialty, 73 (19.8%) chose FM as their first choice, making it the second most popular specialty. In contrast, FM ranked third in popularity among medical students in China (Table 2).
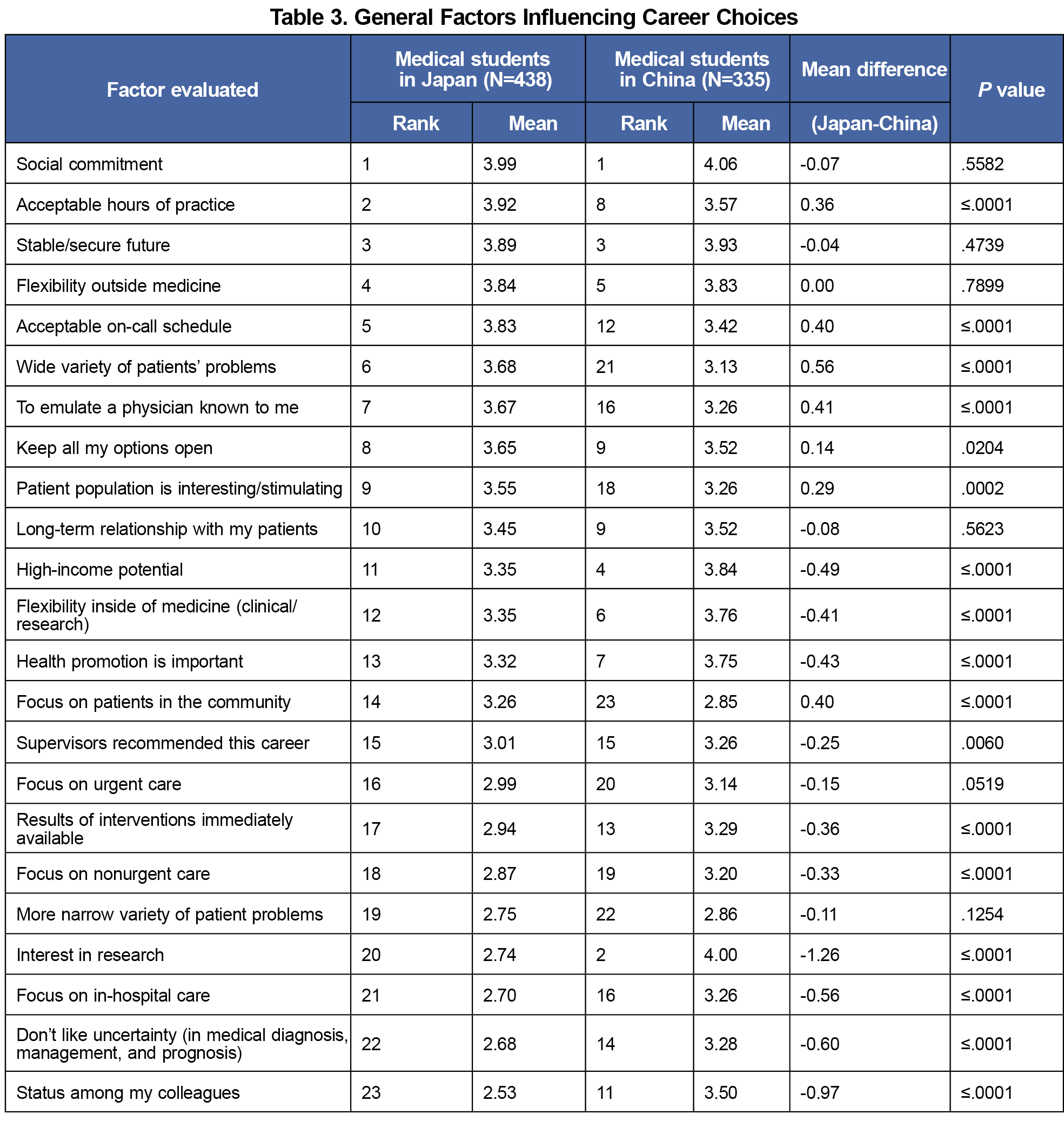
General Factors Influencing Career Decision
Both Japanese and Chinese students valued "social commitment," "acceptable hours of practice," "stable/secure future," "flexibility outside medicine," "keeping all options open," and "long-term relationship with patients." Japanese students also valued "acceptable on-call schedule," "wide variety of patients' problems," and "patient population is interesting/stimulating." Chinese students valued "interest in research," "high-income potential," and "flexibility within medicine" (Table 3).
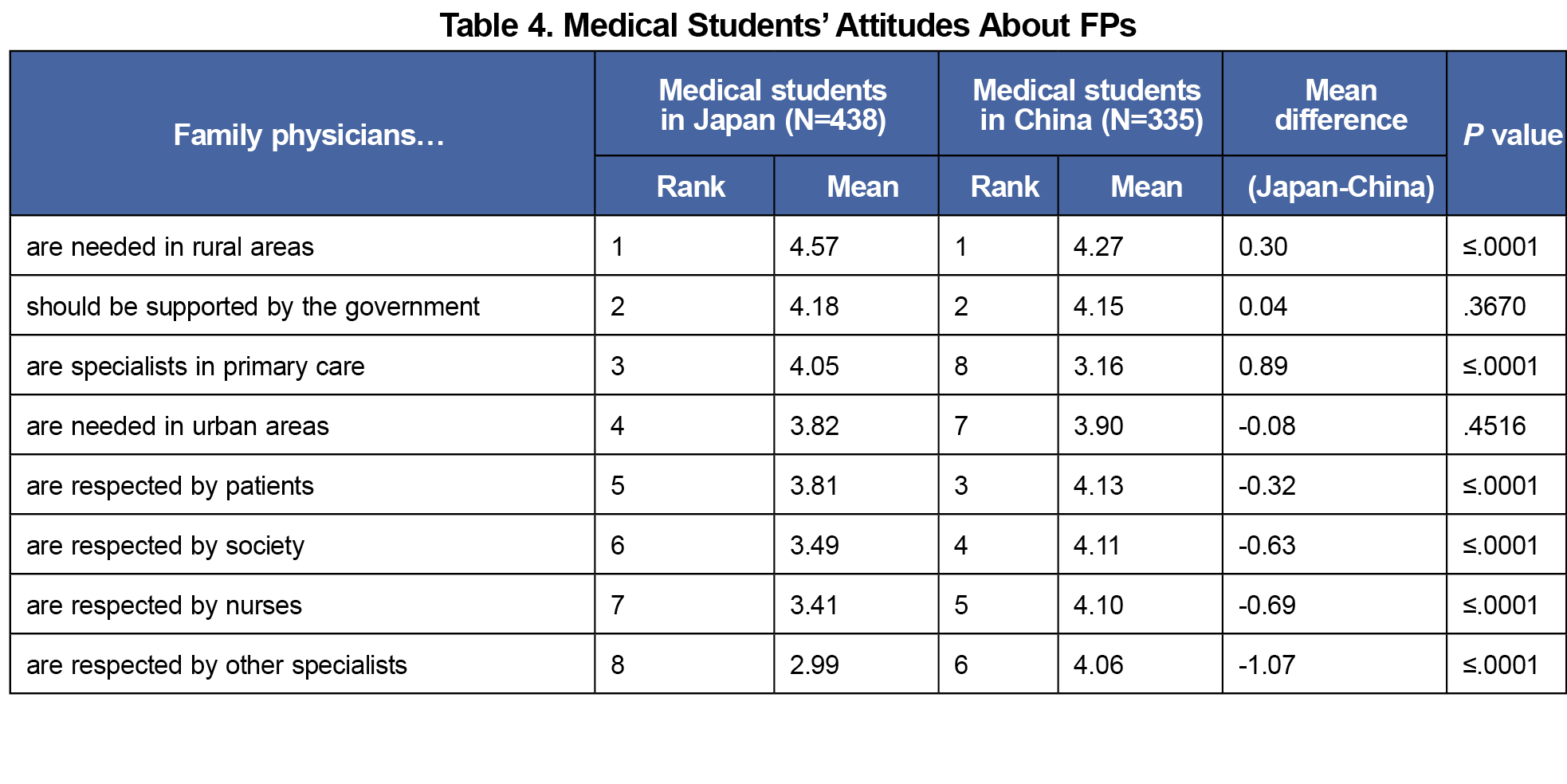
Attitudes Toward FPs
Students in both countries agreed on the need for FPs in rural areas and the necessity of government support for FPs. Chinese students perceived FPs as more respected by society, nurses, and other specialists compared to Japanese students. Japanese students viewed FPs as specialists in primary care, valuing them equally to specialists in other fields, but they assigned lower scores to the level of respect FPs receive from other specialists (Table 4).
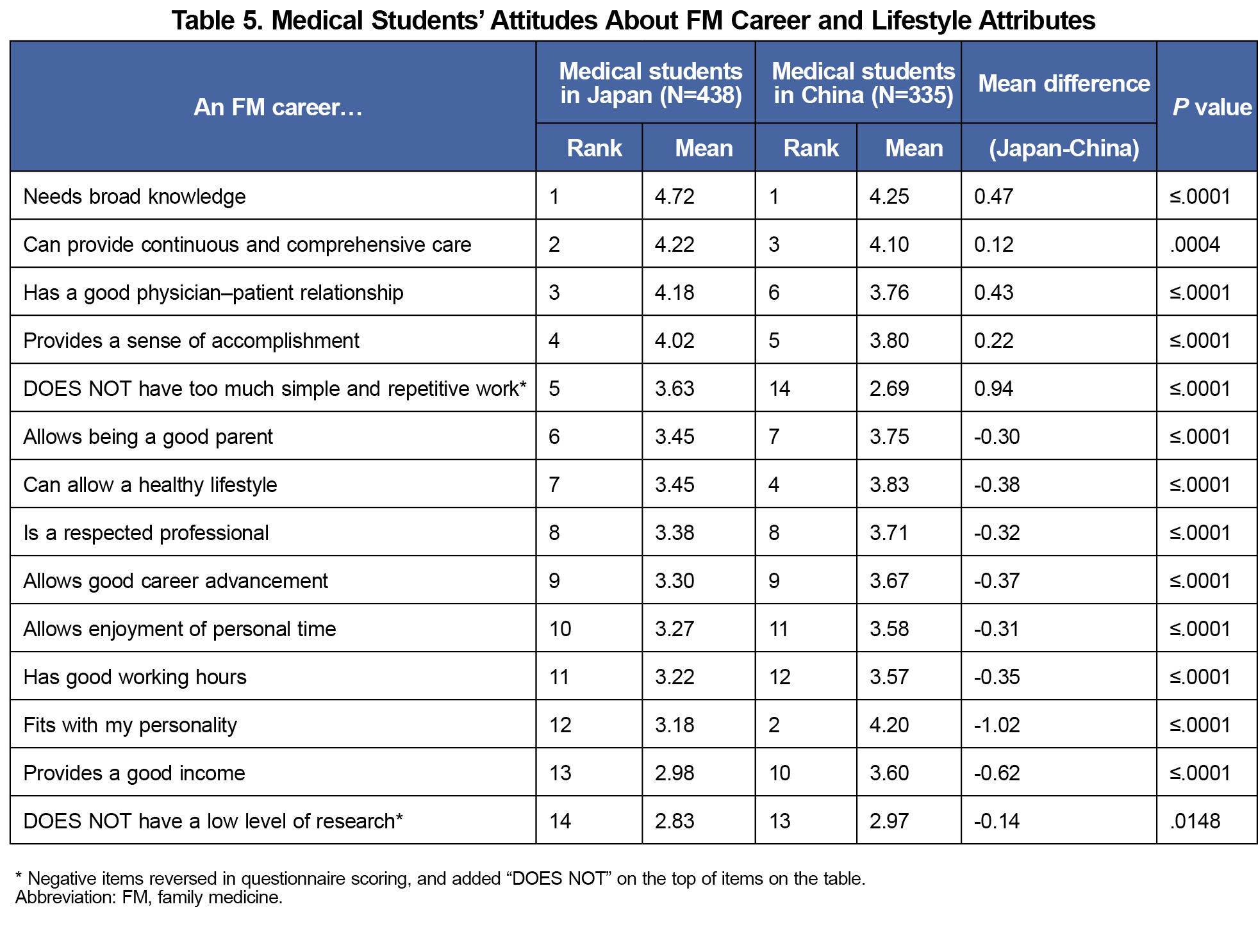
Perspectives on FM Career and Lifestyle
Both groups rated FM career highly in terms of requiring broad knowledge and providing continuous and comprehensive care. However, they were less positive about FPs’ careers offering good income and personal time. Japanese students were more likely to disagree with the statement "FM career has too much simple and repetitive work" (Table 5).
Our study provides valuable insights into the attitudes of Japanese medical students toward FM compared to medical students in China. While FM is a relatively popular specialty among Japanese students, they might be hesitant to choose FM due to negative perceptions, such as low respect for FPs from others and poor work-life balance. This lack of respect for FPs was particularly pronounced in Japan compared to China. Therefore, increasing the prestige of FM and improving work-life balance through flexible working arrangements and enhanced support systems might be effective strategies to attract more medical students to FM. Additionally, we should emphasize the significant contributions of FPs to society, including their broad knowledge and continuous, comprehensive care, as these factors align with the career attributes valued by medical students.
Our study found some students hold the misconception that FM career is too simple and repetitive; however, it is, in fact, highly complex due to the variety of issues addressed during patient visits.10 This complexity may also appeal to students who prioritize factors such as a "wide variety of patients' problems," and an "interesting/stimulating patient population," both of which rank among the top 10 factors influencing career decision-making in Japan.
The promotion of FM is a common challenge faced by many countries. Insights derived from the comparison of two countries with similar cultures and circumstances, but differing outcomes might potentially be applied to enhance the promotion of FM in other countries.
This study has limitations. The voluntary nature of the survey and the inability to accurately calculate the response rate may introduce response bias. Additionally, cultural and systemic differences between Japan and China may influence the generalizability of the findings. It is also noteworthy that the Chinese study only included responses from first-year students, whereas our study collected responses from Japanese medical students across all 6 years of their education. The two studies were conducted 5 years apart, specifically comparing the pre-COVID-19 and post-COVID-19 pandemic periods, which limits the ability to make meaningful comparisons. Future research should address these limitations by employing more robust sampling methods and exploring the cultural nuances that affect medical students' career choices.
Acknowledgments
We extend our deepest gratitude to the medical students who generously assisted in distributing our questionnaires and to the physicians who provided invaluable suggestions for translating our survey. Without their dedicated support and professional insights, this research would not have been possible. Their contributions have significantly enriched the quality of our study, and we are profoundly grateful for their assistance.
We also express our heartfelt appreciation to the late Dr. Michael Fetters, who sadly passed away in 2023. This study and manuscript were conducted under his insightful guidance. Dr Fetters’ contributions to this research were invaluable, and he is deservedly included as an author. His lifelong dedication to family medicine education and his pioneering work in primary care research have left an enduring legacy in the field. His wisdom, mentorship, and passion continue to inspire us, and this work stands as a tribute to his remarkable achievements.
Conflicts of Interest: The authors have no conflicts of interest to disclose in this study.
Presentations: The study results were presented as a poster presentation at STFM 2023 Annual Spring Conference at Tampa, Florida on April 30, 2023.
References
- Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457-502. doi:10.1111/j.1468-0009.2005.00409.x
- Bennett KL, Phillips JP. Finding, recruiting, and sustaining the future primary care physician workforce: a new theoretical model of specialty choice process. Acad Med. 2010;85(10)(suppl):S81-S88. doi:10.1097/ACM.0b013e3181ed4bae
- Ie K, Murata A, Tahara M, et al. What determines medical students’ career preference for general practice residency training?: A multicenter survey in Japan. Asia Pac Fam Med. 2018;17(1):2. doi:10.1186/s12930-018-0039-9
- Otaki J. Considering primary care in Japan. Acad Med. 1998;73(6):662-668. doi:10.1097/00001888-199806000-00013
- Japan Primary Care Association. Number of the Certified Physicians of the JPCA as of December 31, 2022. Accessed April 27, 2023. https://www.primarycare-japan.com/assoc/english/en-membership/
- Ministry of Health, Labour, and Welfare. Statistical overview of medical doctors, Dentists, and pharmacists in 2020 [Japanese]. Vol. 2023. Accessed March 13, 2025. https://www.mhlw.go.jp/toukei/saikin/hw/ishi/20/dl/R02_1gaikyo.pdf
- Zou C, Liao XY, Spicer J, Hayhoe B. Ten years’ GP training in China: progress and challenges. Br J Gen Pract. 2020;70(699):511-512. doi:10.3399/bjgp20X712961
- Chen Q, Lian S, Plegue MA, Fetters MD. First-year medical student attitudes about general practice in China: a comparison between Chinese and international students. Adv Med Educ Pract. 2019;10:571-579. doi:10.2147/AMEP.S198877
- Wright B, Scott I, Woloschuk W, Brenneis F, Bradley J. Career choice of new medical students at three Canadian universities: family medicine versus specialty medicine. CMAJ. 2004;170(13):1920-1924. doi:10.1503/cmaj.1031111
- Katerndahl D, Wood R, Jaén CR. Family medicine outpatient encounters are more complex than those of cardiology and psychiatry. J Am Board Fam Med. 2011;24(1):6-15. doi:10.3122/jabfm.2011.01.100057
Lead Author
Yuki Takeuchi, MD
Affiliations: University of Rochester Medical Center, Department of Family Medicine, Rochester, NY | Teine Keijinkai Hospital, Teine Family Medicine Clinic
Co-Authors
Qi Chen, PhD - School of Health Humanities, Peking University, Beijing, China
Michael D. Fetters, MD, MPH, MA (deceased) - Department of Family Medicine, University of Michigan, Ann Arbor, MI
Corresponding Author
Yuki Takeuchi, MD
Correspondence: University of Rochester Medical Center, Department of Family Medicine, Rochester, NY; Teine Keijinkai Hospital, Teine Family Medicine Clinic
Email: ytakeuchi1016@gmail.com
Fetching other articles... 
Loading the comment form... 
Submitting your comment... 


There are no comments for this article.