Background and Objectives: Hospice and palliative medicine (HPM) is one of three Accreditation Council for Graduate Medical Education accredited clinical subspecialties available to family medicine graduates for fellowship training. Despite this, training is not currently a curriculum requirement. We have pioneered a required 4-week palliative medicine rotation into the curriculum.
Methods: Twenty-eight residents who completed the palliative medicine rotation across four classes were surveyed to assess how the rotation improved their level of comfort with providing end-of-life (EOL) care and to demonstrate the need of formal palliative medicine training. Wilcoxon signed ranks test was used to detect statistical differences between the mean level of comfort of residents pre- and postrotation with providing the basic skills needed to practice HPM.
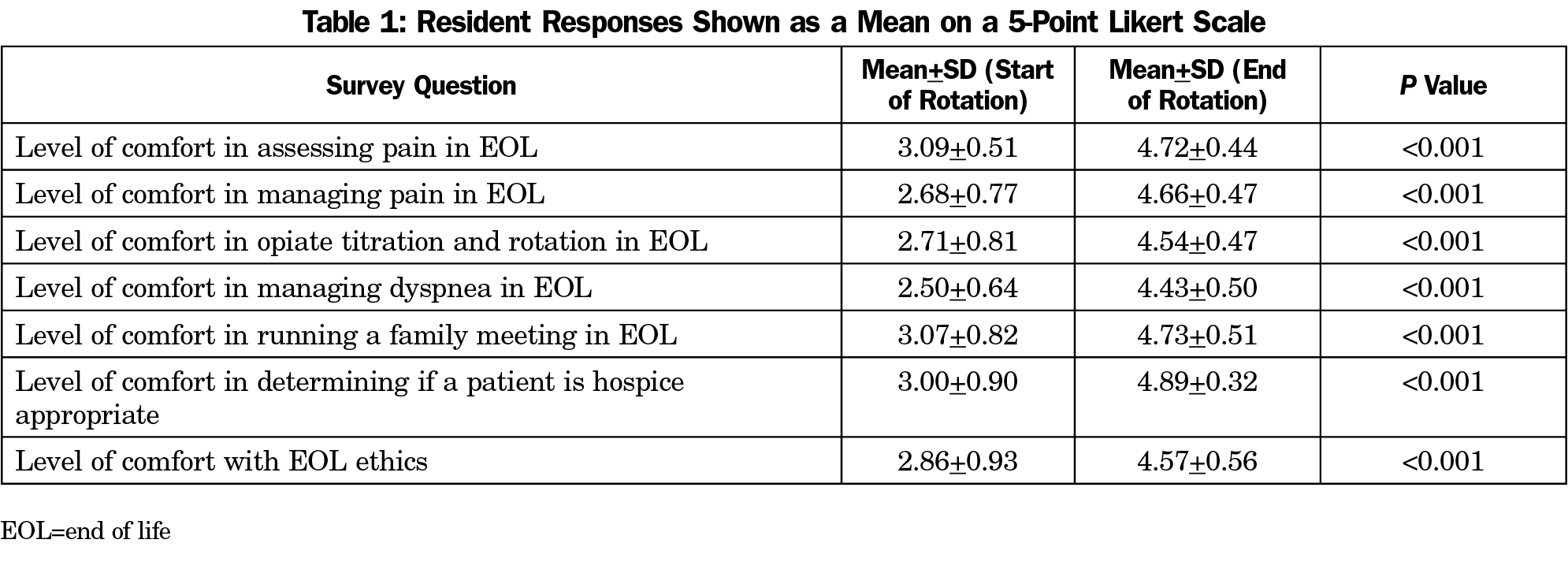
Results: The HPM rotation significantly improved the residents’ level of comfort in all areas of measured EOL care (P<0.001). All residents surveyed strongly agreed that the rotation was valuable to their future and 100% of residents strongly agreed that an HPM rotation should be required.
Conclusions: Formal HPM training should be a required component in residency education and considerations should be given to the 4-week format. This rotation provides a model that can be implemented in other residency programs nationally. Implementation of this rotation may help close the enormous gap of patients not receiving quality EOL care.
In 2006, the American Board of Medical Specialties officially recognized hospice and palliative medicine (HPM) as a subspecialty and the Accreditation Council for Graduate Medical Eduation (ACGME) began accrediting fellowship programs. For the 2016-2017 academic year, there were 117 programs and 362 fellow slots nationally.1 In addition to geriatrics and sports medicine, HPM is the third ACGME-accredited clinical subspecialty for family medicine. The current ACGME program requirements for family medicine include geriatrics and sports medicine, however, there is no equivalent requirement for hospice or palliative patients.2
Hospice and palliative consultation has demonstrated lower health care costs, decreased utilization, and improved quality of care at the end of life (EOL).3-5 In 1998, only 15% of hospitals nationally had a palliative medicine consultation service. That number grew to 67% of hospitals by 2014.6 In 2015, the National Hospice and Palliative Care Organization reported that the number of hospice programs in the United States has nearly doubled since 2000.7 As a result, there is a shortage in the number of physicians available to provide specialty-level HPM care.
Formal training in HPM during residency has shown benefit in multiple studies. A 4-week hospice rotation improved resident confidence regarding palliative skills, and a 2-week required rotation showed improved communication skills.8,9 A significant improvement in knowledge, attitudes, and skills was measured after residents completed a 4-week hospice rotation, and 50% of the residents surveyed perceived that the content was not available elsewhere in their training.10 Another study found a significant improvement in all palliative care domains after residents completed a geriatrics rotation with palliative education built into the curriculum.11 Finally, a Canadian study demonstrated significant improvements of palliative and hospice medical knowledge in second-year family medicine residents after completing a 2-week palliative rotation.12 To our knowledge, the Drexel University College of Medicine Family Medicine Residency is the only family medicine program with a required 4-week hospice and palliative medicine rotation that combines hospital consultation and hospice. The aims of this study were to assess how this rotation improves comfort of family medicine residents in EOL care, and to measure if residents valued this experience enough justify a required rotation.
Rotation Design
Two weeks are required on the hospital-based palliative consultation service and one week at an inpatient hospice unit. The fourth week can be at either site, depending on resident preference. Throughout the rotation residents participate in weekly HPM fellow conference.
Data Collection
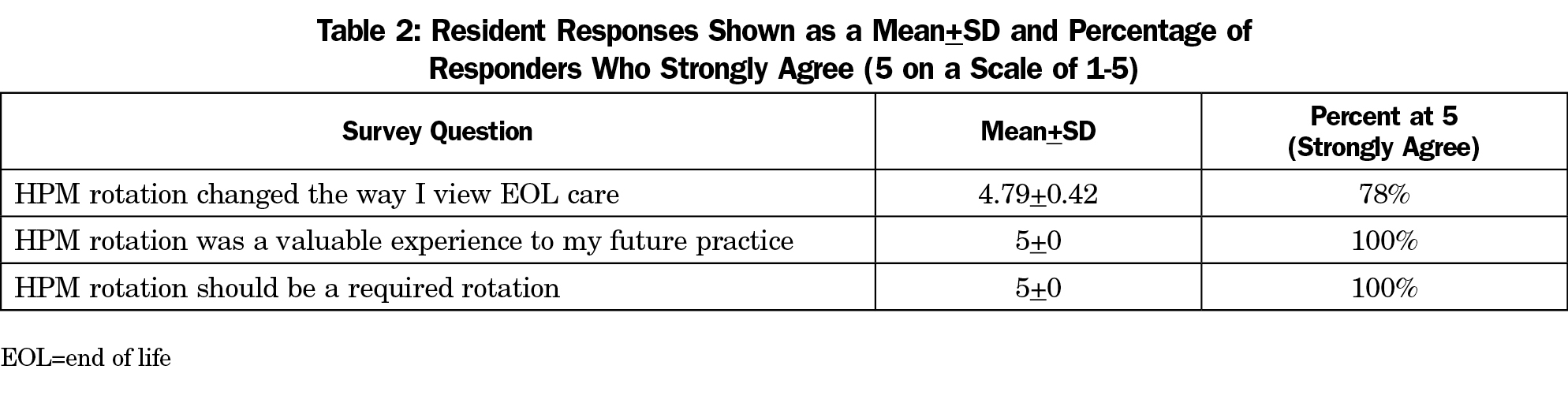
Family medicine residents were surveyed across four classes after the completion of the 4-week rotation. Questions 1 through 7 ask the residents to rate their level of comfort in providing the basic skills needed to properly practice HPM before and after the rotation using a 5-point Likert scale. Using the same scale, questions 8 through 10 ask the residents if the rotation: (a) changed their view of EOL care, (b) was valuable to their future practice, and (c) should be a required rotation in the curriculum.
Data Analysis
A Wilcoxon signed ranks test was used for the first seven questions to detect a statistical difference between the mean level of comfort of the resident pre- and postrotation. For questions 8 through 10, the percentage of residents that strongly agreed with the statement was calculated. This study received exemption status from the Drexel College of Medicine Institutional Review Board.
A total of 28 residents completed the palliative care rotation from July 2012 through July 2015. All questionnaires had 100% completion.
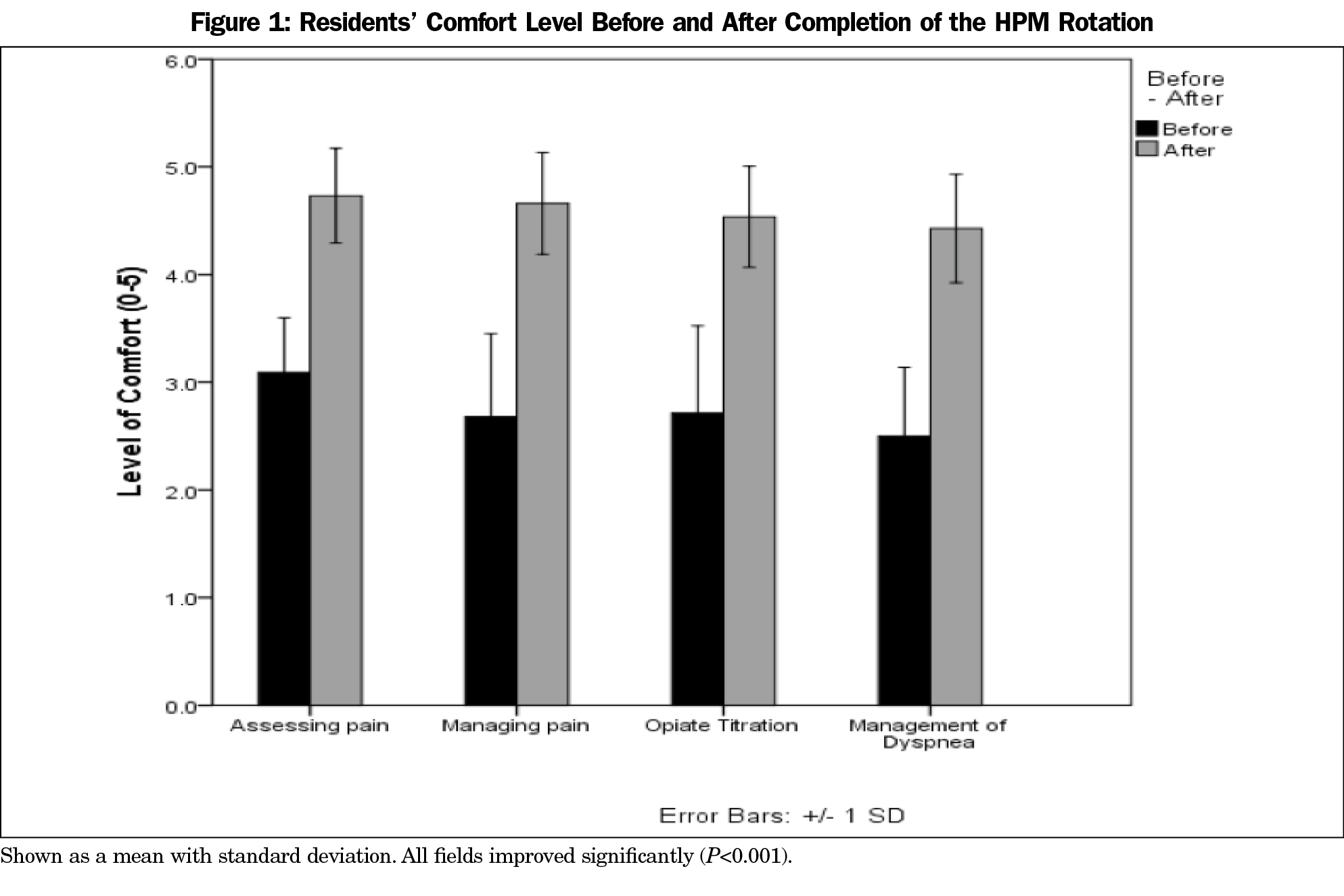
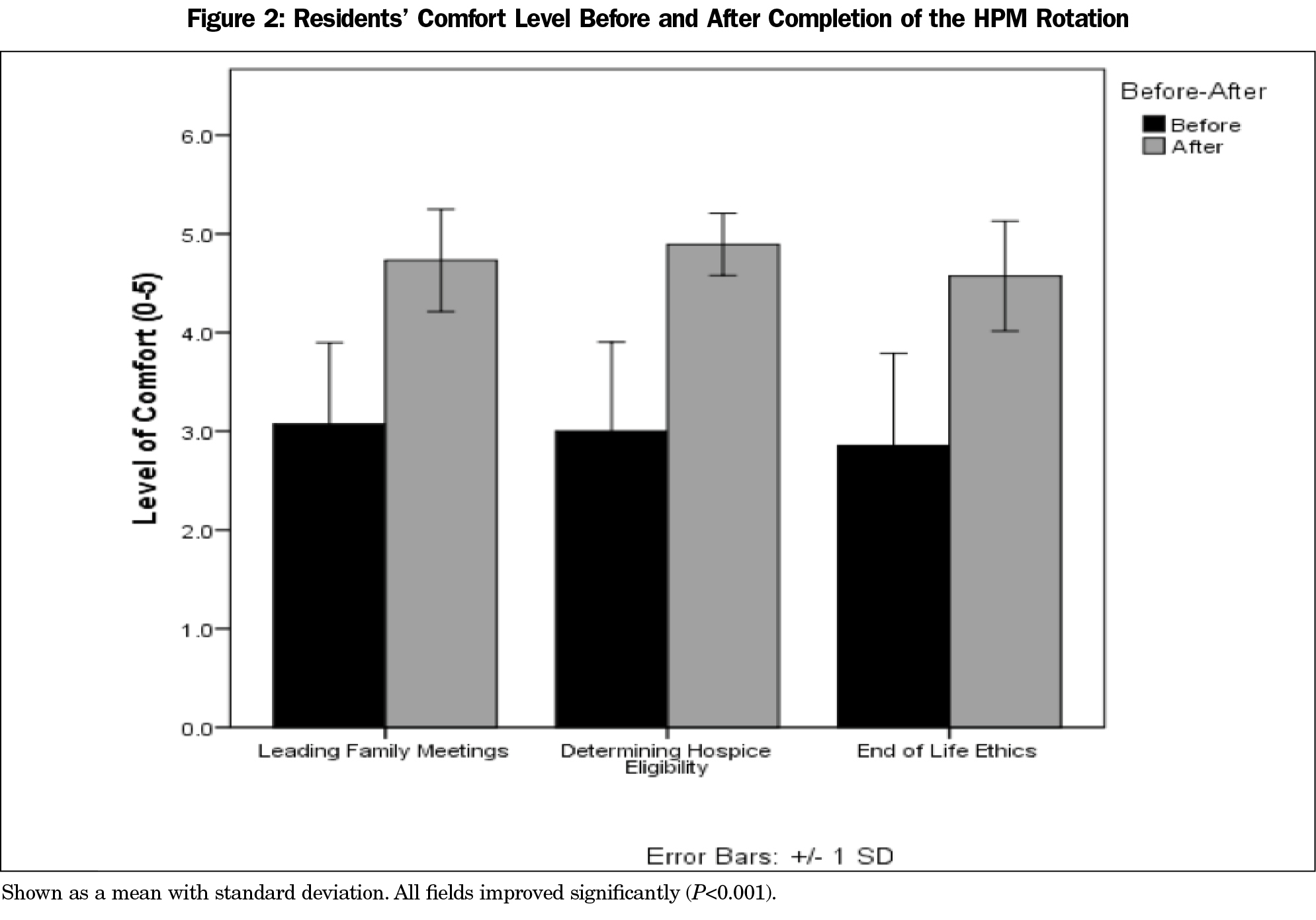
Upon completion of the palliative medicine rotation, there was significant improvement in the residents’ self-assessment in providing all basic HPM skills. Residents felt improvement and more confidence in assessing pain, managing pain, opiate titration and rotation, managing determining if a patient is appropriate for hospice, and EOL ethics (Table 1, Figures 1 and 2)
The percentage of residents that strongly agreed was calculated for questions 8 through 10 (Table 2). Seventy-eight percent of residents strongly agreed that the palliative medicine rotation changed the way they view EOL care. All residents strongly agreed that a palliative medicine rotation was a valuable experience to their future practice and that palliative medicine should be a required rotation.
Based on our study, the palliative medicine rotation significantly improved the residents’ level of comfort in all measured areas. These skills are vitally important to the development of a family physician regardless of future practice setting. The importance of these skills was recognized by the residents and reflected their agreement that the rotation was a valuable experience to their future practice.
Another important result of this study was that all residents surveyed strongly agreed that the 4-week rotation should be required. With greater need for providers skilled at EOL care, adding a palliative medicine requirement in residency serves as an opportunity to help close the gap and increase quality of care provided to terminal patients. Family physicians are well suited to fill this gap due to the emphasis placed on continuity, building relationships, and caring for the family unit. To provide quality care for patients who are gravely ill and dying, family physicians need a basic skill set that includes facilitating discussions on goals of care and managing EOL symptoms. By incorporating a required rotation into the residency curriculum, residents will be exposed to HPM early in their training to broaden their knowledge and provide exposure to residents if fellowship training is desired.
Our study is based on residents’ self-assessment of their level of comfort in providing HPM as opposed to objective performance evaluation. This design may have recall bias as it is asking residents to self-evaluate after the rotation was complete. However, this methodological design also allows for residents to serve as their own control and eliminates confounding biases, which could be seen as a strength. Lastly, despite data gathering over four classes, our study is still limited to a small sample size at a single institution.
This rotation can provide a model example that can be implemented in other residency programs. Implementation of this rotation may help close the gap of patients not receiving quality EOL care.
Acknowledgments
Pilot data was presented as a poster at the American Association of Hospice and Palliative Medicine Annual Assembly, February 24-28, 2015, Philadelphia, PA.
References
- American Academy of Hospice and Palliative Medicine. Hospice and Palliative Medicine Fellowship Programs (Data Table). http://aahpm.org/uploads/Program_Data_Table_102516.pdf. Accessed May 30, 2017.
- Accreditation Council for Graduate Medical Education. ACGME Family Medicine Program Requirements. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/120_family_medicine_2016.pdf. Accessed May 30, 2017.
- Teno JM, Clarridge BR, Casey V, et al. Family perspectives on end-of-life care at the last place of care. JAMA. 2004;291(1):88-93.
https://doi.org/10.1001/jama.291.1.88.
- Emanuel EJ, Ash A, Yu W, et al. Managed care, hospice use, site of death, and medical expenditures in the last year of life. Arch Intern Med. 2002;162(15):1722-1728.
https://doi.org/10.1001/archinte.162.15.1722.
- Bakitas M, Lyons KD, Hegel MT, et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA. 2009;302(7):741-749.
https://doi.org/10.1001/jama.2009.1198.
- Dumanovsky T, Augustin R, Rogers M, Lettang K, Meier DE, Morrison RS. The Growth of Palliative Care in U.S. Hospitals: A Status Report. J Palliat Med. 2016;19(1):8-15.
https://doi.org/10.1089/jpm.2015.0351.
- National Hospice and Palliative Care Organization. NHPCO Facts and Figures: Hospice Care in America, 2015. https://www.nhpco.org/sites/default/files/public/Statistics_Research/2015_Facts_Figures.pdf. Accessed August 10, 2017.
- von Gunten CF, Mullan PB, Nelesen R, et al. Primary Care Residents Improve Knowledge, Skills, Attitudes, and Practice After a Clinical Curriculum With a Hospice. Am J Hosp Palliat Care. 2017;34(8):713-720.
- Vergo MT, Sachs S, MacMartin MA, Kirkland KB, Cullinan AM, Stephens LA. Acceptability and impact of a required palliative care rotation with pre-rotation and post-rotation observed simulated clinical experience during internal medicine residency training on primary palliative communication skills. J Palliat Med. 2017;20(5):542-547.
https://doi.org/10.1089/jpm.2016.0348.
- Von Gunten CF, Mullan PB, Harrity S, et al; Faculty, Center for Pallative Study. Residents from five training programs report improvements in knowledge, attitudes and skills after a rotation with a hospice program. J Cancer Educ. 2003;18(2):68-72.
https://doi.org/10.1207/S15430154JCE1802_06.
- Montagnini M, Varkey B, Duthie E Jr. Palliative care education integrated into a geriatrics rotation for resident physicians. J Palliat Med. 2004;7(5):652-659. https://doi.org/10.1089/jpm.2004.7.652.
- Oneschuk D, Fainsinger R, Hanson J, Bruera E. Assessment and knowledge in palliative care in second year family medicine residents. J Pain Symptom Manage. 1997;14(5):265-273.
https://doi.org/10.1016/S0885-3924(97)00179-6.



There are no comments for this article.