Background and Objectives: The national opioid crisis requires medical education to develop a proactive response centering on prevention and treatment. Primary care providers (PCPs)—many of whom are family medicine physicians—commonly treat patients on opiates, and write nearly 50% of opioid prescriptions. Despite linkages between PCP opioid prescribing patterns and the associated potential for overdose, little is known about how family medicine clerkship students are trained to prevent opioid overdose, including training on the use of naloxone. This study describes the presence of opioid overdose education at the national level and barriers to inclusion. It also discusses implementation strategies along with instructional methodology and learner evaluation.
Methods: Data were collected as part of a cross-sectional survey administered electronically by the Council of Academic Family Medicine Educational Research Alliance to 139 family medicine clerkship directors.
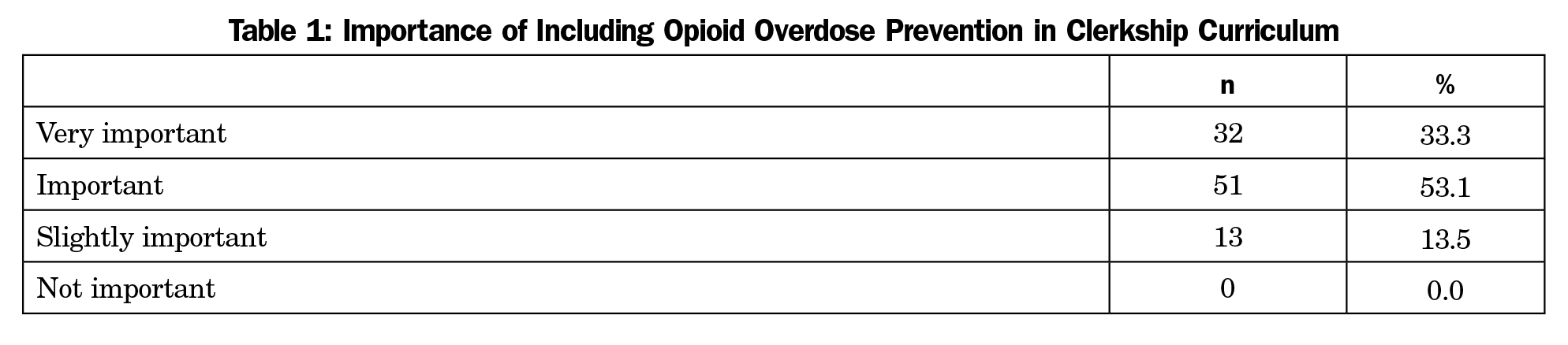
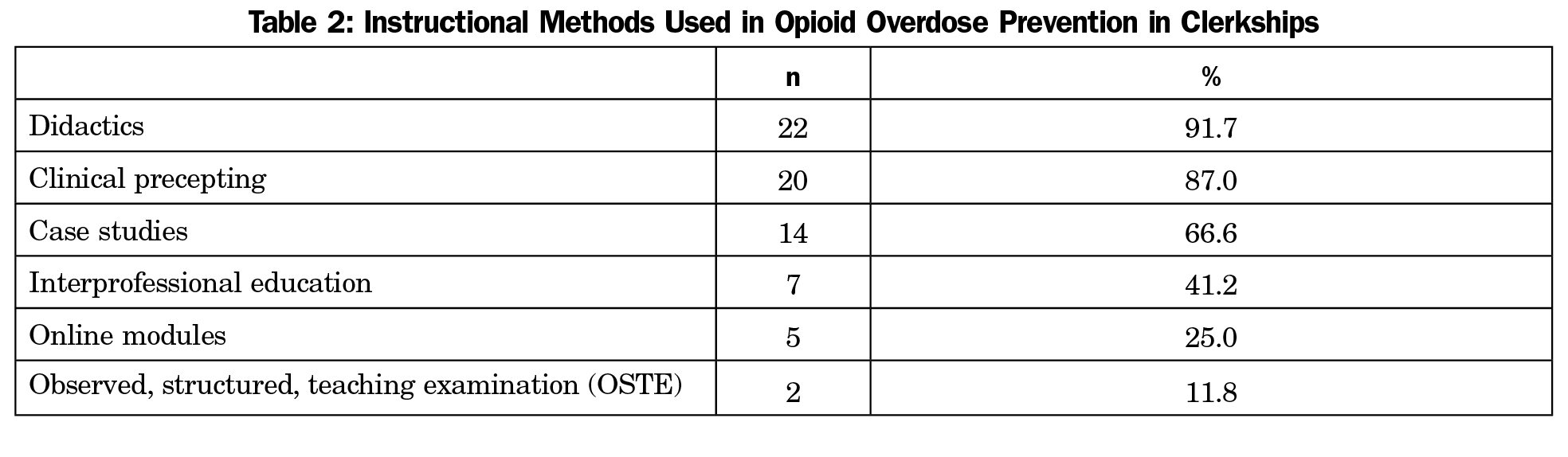
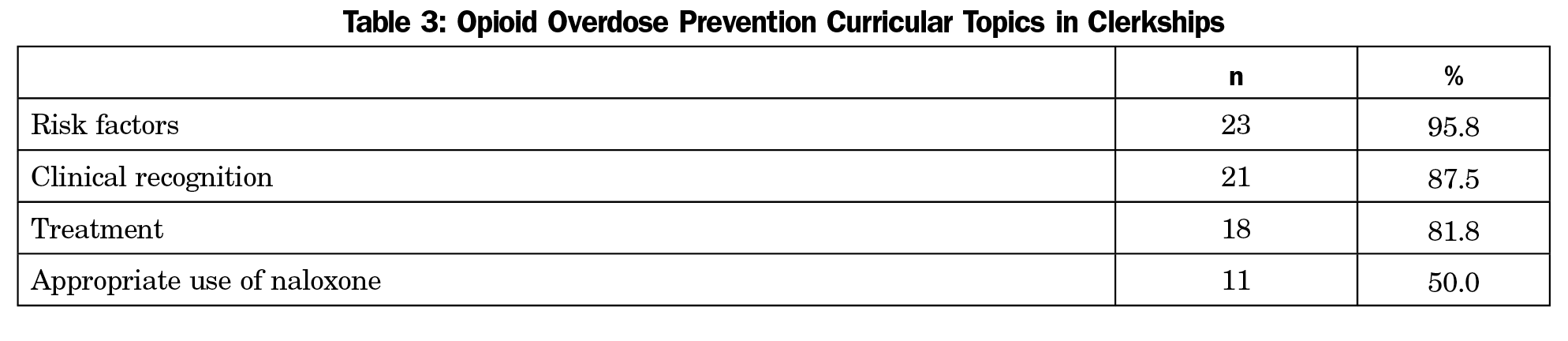
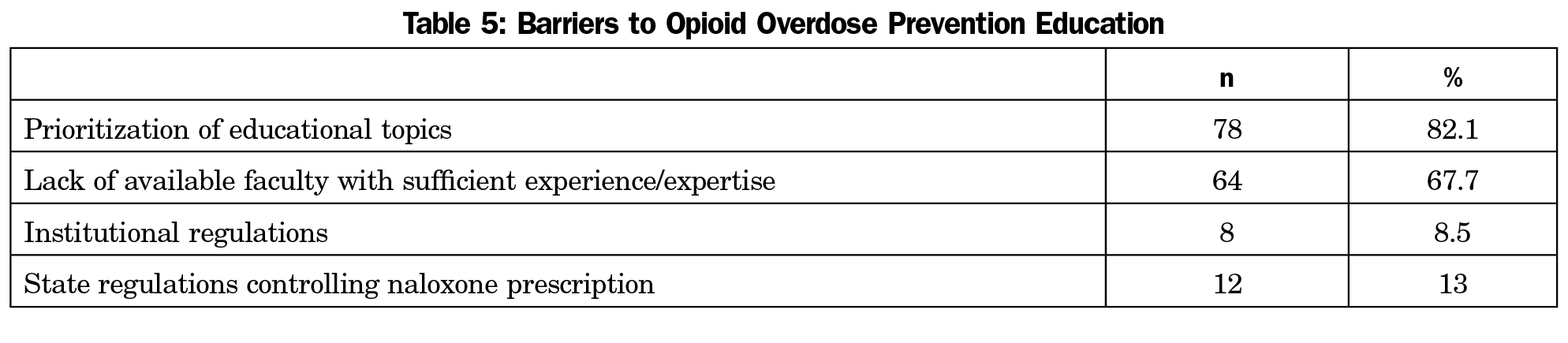
Results: A total of 99 clerkship directors (71.2% response rate) responded to the survey. A large majority (86.4%) agreed that it is important to offer opioid overdose prevention education in the clerkship, yet only 25.8% include this topic. Of these, only 50.0% address naloxone use. The most common barriers to including opioid overdose prevention education were prioritization of educational topics (82.1%) followed by lack of available faculty with sufficient experience/expertise (67.7%).
Conclusions: Findings point to a disparity between perceived importance of opioid overdose prevention education and inclusion of this topic in family medicine clerkship-level medical education. Innovative use of online education and partnering with community resources may address barriers related to curricular prioritization while supporting interprofessional education principles.
The United States is in the midst of an opioid abuse and overdose public health emergency. National data demonstrate a 2.8-fold increase in deaths attributed to opioid overdose in less than 15 years.1 Approximately 50% of opioid prescriptions are written by primary care providers (PCPs),2 many whom are family medicine physicians. Despite linkages between primary care, opioid prescriptions, and overdose, little is known about how family medicine clerkship students are trained to prevent overdose.
Although medical schools have responded to the opioid crisis by implementing pain management/addiction curricular changes, medical education literature is scarce regarding overdose prevention, including naloxone prescription.3-12 Overdose education in medical training is vital as PCPs are uniquely positioned to practice prevention and implement harm reduction.13,14 While timely naloxone administration is effective in reversing overdose, naloxone awareness remains low among PCPs,15 and physicians cite inadequate addictions education as a barrier to naloxone use.13
Given the prevalence of overdose and PCP opioid prescribing patterns, we wanted to examine overdose education in family medicine clerkships to determine curricular implementation along with instructional and evaluation approaches. Standards put forth by the Liaison Committee on Medical Education (LCME) mandate that physicians must be prepared to screen, intervene, and treat patients with substance abuse disorders.16 The Society of Teachers of Family Medicine (STFM) National Clerkship Curriculum recommendations endorse inclusion of substance use, dependence, and abuse within adult core chronic disease presentations.11 Despite these recommendations, medical education literature is deficient in describing overdose prevention curricula and corresponding evaluation strategies.17
We partnered with STFM-appointed advisors to develop a survey targeting family medicine clerkship directors using the Council of Academic Family Medicine’s (CAFM) Educational Research Alliance (CERA) national survey mechanism. Email invitations issued by CERA invited family medicine clerkship directors to participate.18 The web-based SurveyMonkey program was used to collect electronic responses. Nonrespondents received a total of five reminders. The American Academy of Family Physicians Institutional Review Board approved the study.
Survey Design
Demographic data were collected as part of the general CERA survey. The nine survey questions related to two outcome variables: (1) the importance of overdose prevention education, and (2) inclusion of overdose prevention in the curriculum. Importance of overdose prevention was measured using Likert-type scale responses (not important, slightly important, important, very important). The inclusion outcome variable was binary (yes/no). Independent variables were: (1) instructional methodology, (2) curricular content, (3) evaluation methodology, (4) barriers to overdose prevention curriculum implementation, and (5) barriers limiting naloxone education. Independent variables measured agreement using Likert-type scale responses (strongly disagree, disagree, agree, strongly agree). Branching logic was utilized to limit the number of questions. If a respondent answered “no” to inclusion of overdose prevention education, the three questions related to instructional methodology, curricular content, and evaluation methodology were automatically excluded.
Analysis
Frequencies and proportions were calculated; inferential statistical analysis included χ2 testing and Fisher’s exact test of association, with significance defined at α=0.05. All analyses were conducted using the SAS 9.4 statistical program (SAS Institute Inc, Cary, NC).
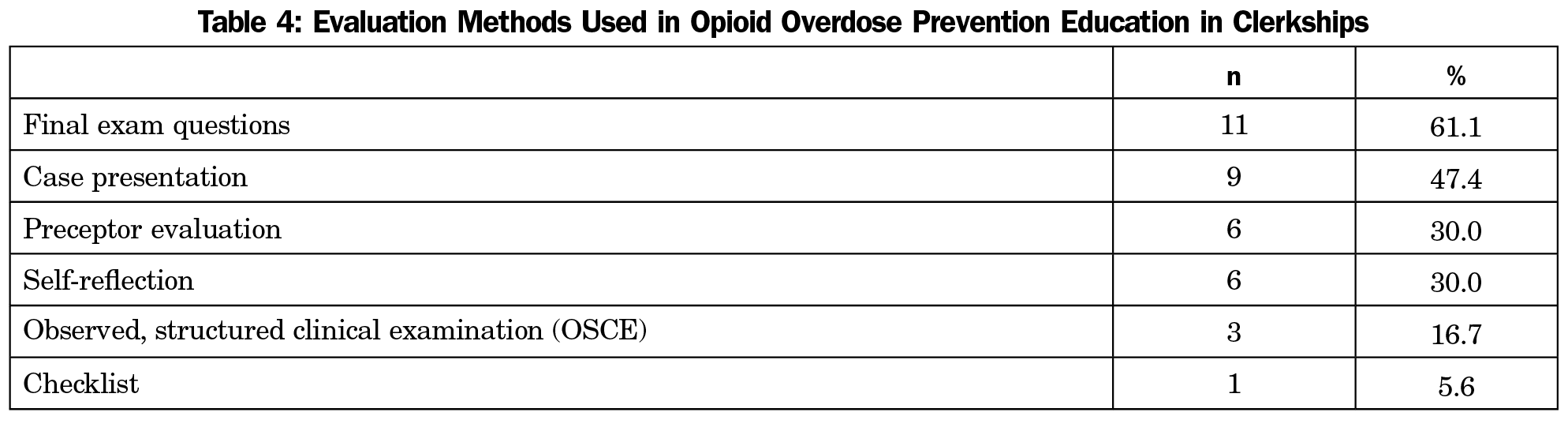
The survey was distributed to family medicine clerkship directors between June 28, 2017 and August 4, 2017. Ninety-nine of 139 clerkship directors responded (71.2% response rate). Fifty-five (56.7%) respondents reported serving between 2 and 7 years as a director. Regarding respondent characteristics, 73 (76.8%) are white and three (3.2%) reported Hispanic ethnicity; 57 (59.4%) are female. Although 83 (86.4%) reported valuing overdose education, only 25 (25.8%) included this topic within the curriculum. Clerkships including this topic overwhelmingly utilize didactics (n=22, 91.7%) and precepting (n=20, 87.0%) to deliver content related to overdose risk factors (n=23, 95.8%), clinical recognition (n=21, 87.5%) and treatment (n=18, 81.8%) with only 11 (50%) reporting naloxone prescription education. Learners are evaluated most frequently through use of final exam questions (n=11, 61.1%). The competing demands of other important topics in the curriculum were identified as the greatest barrier (n=78, 82.1%) to implementing overdose education. No statistically significant associations were found using χ2 and Fisher’s exact statistical tests. Tables 1-5 illustrate salient results.
Since directors view overdose prevention as a highly important topic, further discussion and research are required to enhance uptake of this valued curriculum. Results point to the need to reprioritize curricula to integrate this topic into existing course content. Furthermore, few clerkships are using interprofessional education in teaching overdose prevention.
Online modules are a proven method of delivering content without substantial reprioritization. Use of the virtual patient experience (VPE) model may prove especially beneficial.19 This model offers self-paced, low-risk practice opportunities and is an equivalent, cost-effective method easily adaptable to other interprofessional learners. Online learning technologies are equally effective in attaining educational goals.20 Importantly, VPE strengthens learner communication efficacy, allowing clinical approach flexibility to best meet patient needs and improve outcomes, including patient safety. The value of online methods will be assessed in the next phase of the current study, which examines fourth-year medical students’ experiences and preferences regarding opioid overdose education.
It is also necessary to train existing faculty or recruit new faculty with overdose prevention experience/expertise. It will be worthwhile to consider engaging community-allied health professionals (eg, pharmacists) to augment training resources and support interprofessional education principles. Utilizing substance abuse professionals would afford further opportunity to address appropriate use of naloxone as well.
Limitations
Branching logic was utilized to reduce the number of questions, yet the binary inclusion outcome variable limited responses to a single value. Therefore, the binary outcome variable prohibited logit model development. Social desirability bias must be considered. Electronic survey administration produces decreased control of the sample, potentially skewing sampling.
Despite increasing overdose incidence and naloxone’s clinical significance in overdose management, results demonstrate that a limited number of family medicine clerkships include this within their curricula. PCPs play a pivotal role in reducing overdose deaths, using naloxone to maintain patient-provider trust with safe, compassionate care.13 Physicians cannot provide this care without appropriate training; family medicine clerkships must provide tools for future physicians to effectively and compassionately care for patients who are prescribed opioid treatment.
Acknowledgments
The authors thank Yumin Wang, MS for his support with statistical analysis and Colin Ray for drafting the annotated bibliography which served as the foundation for this study.
References
- National Institute on Drug Abuse. Overdose death rates. https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates. Accessed February 10, 2017.
- Centers for Disease Control and Prevention. Why guidelines for primary care providers? https://www.cdc.gov/drugoverdose/pdf/guideline_infographic-a.pdf. Accessed February 10, 2017.
- Gatewood AK, Van Wert MJ, Andrada AP, Surkan PJ. Academic physicians’ and medical students’ perceived barriers toward bystander administered naloxone as an overdose prevention strategy. Addict Behav. 2016;61:40-46. https://doi.org/10.1016/j.addbeh.2016.05.013
- Klimas J, Egan M, Tobin H, Coleman N, Bury G. Development and process evaluation of an educational intervention for overdose prevention and naloxone distribution by general practice trainees. BMC Med Educ. 2015;15(15):206. https://doi.org/10.1186/s12909-015-0487-y
- Kothari D, Gourevitch MN, Lee JD, et al. Undergraduate medical education in substance abuse: a review of the quality of the literature. Acad Med. 2011;86(1):98-112. https://doi.org/10.1097/ACM.0b013e3181ff92cf
- Krisberg K. Medical schools confront opioid crisis with greater focus on pain, addiction education. AAMC News. https://www.aamc.org/newsroom/newsreleases/464576/medical_schools_confront_opioid_crisis_08042016.html. Accessed February 10, 2017.
- Matheson C, Pflanz-Sinclair C, Aucott L, et al. Reducing drug related deaths: a pre-implementation assessment of knowledge, barriers and enablers for naloxone distribution through general practice. BMC Fam Pract. 2014;15(1):12. https://doi.org/10.1186/1471-2296-15-12
- Midmer D, Kahan M, Wilson L. Medical students’ experiences with addicted patients: a web-based survey. Subst Abus. 2008;29(1):25-32. https://doi.org/10.1300/J465v29n01_04
- Neufeld KJ, Alvanzo A, King VL, et al. A collaborative approach to teaching medical students how to screen, intervene, and treat substance use disorders. Subst Abus. 2012;33(3):286-291. https://doi.org/10.1080/08897077.2011.640090
- Ram A, Chisolm MS. The time is now: improving substance abuse training in medical schools. Acad Psychiatry. 2016;40(3):454-460.
- Society of Teachers of Family Medicine. The Family Medicine Clerkship Curriculum. http://www.stfm.org/Resources/STFMNationalClerkshipCurriculum. 2015. Accessed August 6, 2018.
- Tanner TB, Wilhelm SE, Rossie KM, Metcalf MP. Web-based SBIRT skills training for health professional students and primary care providers. Subst Abus. 2012;33(3):316-320. https://doi.org/10.1080/08897077.2011.640151
- Bowman S, Eiserman J, Beletsky L, Stancliff S, Bruce RD. Reducing the health consequences of opioid addiction in primary care. Am J Med. 2013;126(7):565-571. https://doi.org/10.1016/j.amjmed.2012.11.031
- Hawk KF, Vaca FE, D’Onofrio G. Reducing Fatal Opioid Overdose: Prevention, Treatment and Harm Reduction Strategies. Yale J Biol Med. 2015;88(3):235-245.
- Behar E, Rowe C, Santos G-M, Santos N, Coffin PO. Academic detailing pilot of naxolone prescribing among primary care providers in San Francisco. Fam Med. 2017;49(2):122-126.
- Liaison Committee on Medical Education. Functions and structure of a medical school: Standards for accreditation of medical education programs leading to the MD degree. http://lcme.org/publications/#Standards. 2018. Accessed October 13, 2017.
- Bailey M. Medical students demand better training to tackle opiod crisis. STAT. https://www.statnews.com/2016/05/17/opioid-addiction-medical-schools/. Published May 17, 2016. Accessed February 12, 2017.
- Seehusen DA, Mainous AG III, Chessman AW. Creating a centralized infrastructure to facilitate medical education research. Ann Fam Med. 2018;16(3):257-260. https://doi.org/10.1370/afm.2228
- Harris S. Finding the balance: virtual patients up for debate. AAMC Reporter. 2011; October 2011.
- Triola M, Feldman H, Kalet AL, et al. A randomized trial of teaching clinical skills using virtual and live standardized patients. J Gen Intern Med. 2006;21(5):424-429. https://doi.org/10.1111/j.1525-1497.2006.00421.x



There are no comments for this article.