Background and Objectives: Little is known about how the presence of nurse practitioners (NPs) and physician assistants (PAs) in a practice impacts family physicians’ (FPs’) scope of practice. This study sought to examine variations in FPs’ practice associated with NPs and PAs.
Methods: We obtained data from American Board of Family Medicine practice demographic questionnaires completed by FPs who registered for the Family Medicine Certification Examination during 2013-2016. Scope of practice score was calculated for each FP, ranging from 0-30 with higher numbers equating to broader scope of practice. FPs self-reported patient panel size. Primary care teams were classified into NP only, PA only, both NP and PA, or no NP or PA. We estimated variation in scope and panel size with different team configurations in regression models.
Results: Of 27,836 FPs, nearly 70% had NPs or PAs in their practice but less than half (42.5%) estimated a panel size. Accounting for physician and practice characteristics, the presence of NPs and/or PAs was associated with significant increases in panel sizes (by 410 with PA only, 259 with NP only and 245 with both; all P<0.05) and in scope score (by 0.53 with PA only, 0.10 with NP only and 0.51 with both; all P<0.05).
Conclusions: We found evidence that team-based care involving NPs and PAs was associated with higher practice capacity of FPs. Working with PAs seemed to allow FPs to see a greater number of patients and provide more services than working with NPs. Delineation of primary care team roles, responsibilities and boundaries may explain these findings.
Team-based care has increasingly become a practical strategy that family physicians (FPs) use to respond to the surging volume of patient visits nationwide and the growing shortage of primary care physicians.1,2 Over half of FPs report working with nurse practitioners (NPs) and nearly 40% with physician assistants (PAs).3-6 Evidence suggests that the quality of care and health outcomes of patients seen by NPs or PAs are comparable to those seen by physicians,7-11 although patients cared for by NPs and PAs are more likely to be younger, female, and living in rural areas.12 Team-based care models may enable physicians to see greater numbers of patients or provide a broader scope of services.13 While crucial to the transformation of the US primary care delivery system, little is known about the impact of team-based care with NPs and PAs on FPs’ patient panel size and scope of practice.
Patient panel size, commonly estimated by the number of patients seen in the prior 18-24 months,14,15 is a vital piece of practice information that provides the basis for panel management and enables FPs to assess continuity of care. Nonetheless, only a third of FPs can estimate their patient panel size.16 Although patient panel size varied with the time spent in direct patient care, only one-third of FPs’ estimates were reasonable, indicating physicians may be overpaneled and/or underresourced.16-18 While a broader scope of practice of primary care physicians is associated with lower health care costs,19 the scope of practice of FPs has been declining over the last decade.20-22 Working with an NP or PA who can partially supplement or substitute the responsibilities of a physician23,24 may enable the physician to provide more services or to simply take care of more patients. For example, an NP may take a supplementary role where, rather than managing their own panel of patients, they may provide specific services such as acute care. The FP would then be free to conduct a procedure clinic or round in the nursing home. If both the NP and FP were working as usual providers, neither may be able to provide a procedure clinic or see patients outside the office. Team-based care may also have implications for potential strategies to accommodate projected increases in the patient population resulting from expanded insurance coverage due to the Affordable Care Act. Having other clinicians in the practice may allow physicians to more efficiently triage available medical resources to patients.13
Despite the national movement toward team-based primary care models,25,26 no available literature was found on the effect of working with NPs or PAs on a physician’s practice pattern. The objective of our study was to determine whether the patient panel size and scope of practice of FPs varied with presence of an NP, a PA or both at their primary practice site.
Data Source
We pooled 4 years of data from practice demographic questionnaires completed by FPs who registered for the American Board of Family Medicine (ABFM) Family Medicine Certification Examination during 2013-2016. This questionnaire is a required component of the examination registration process for physicians seeking to continue their certification. This requirement provided us with not only a 100% response rate to the questionnaire but more importantly a sample representative of approximately 40% ABFM certified FPs. Personal demographic information collected from ABFM administrative data included date of birth, gender, and medical degree. Practice characteristics from the questionnaire included size, specialty mix, ownership, location, care delivery model, and practice team configuration. Additionally, an array of 22 questions covering the spectrum of primary care activities was asked to discern scope of practice (see Appendix Table 2 at https://journals.stfm.org/media/2222/appendixtables-dai-fm.pdf for the 22 activities). FPs who provided direct patient care were asked to estimate their own patient panel size.
Outcomes
We calculated the Scope of Practice for Primary Care (SP4PC) score, using the Individual Scope of Practice (I-SOP) Scale (range 0-30) for each FP based on the number of primary care activities they reported providing.27 Higher scores represent a broader scope of practice. Patient panel size was obtained from physicians who were able to estimate their panel size. As a result, physicians with missing panel size estimates (ie, those who were not able to provide an estimate) were excluded from panel size analyses. Both outcomes were included in the analyses as continuous variables.
Explanatory Variables
FPs were asked to select all that apply to the question “The following types of providers work in my primary practice site.” Practice team configuration was measured by mutually exclusive indicators specifying whether the FP had NP only, PA only, both PA and NP, or no PA or NP in the practice.
Covariates
To account for potential confounders, we controlled for the following physician and practice characteristics in the regression analysis. Physician age was calculated as of the midyear of the examination year. Gender, race (white vs nonwhite), and medical degree (MD vs DO) were coded as dummy variables. Practice size was categorized as solo, small (2-5 providers), medium (6-20 providers), or large (>20 providers). Specialty mix included multispecialty and single-specialty. We classified four forms of ownership: group, public (federally qualified health center or look-alike, rural health clinic), integrated (health maintenance organization, Veterans Administration), and other (ambulatory surgical center, mental health center). Using practice zip code, rural and urban practice location was determined following the Rural-Urban Commuting Area Codes (RUCA, Version 2.0) designation.28 Practices certified as Patient-Centered Medical Home (PCMH) were identified by physician self-report.
Analysis
We only included FPs who provided direct patient care. As we were interested in patient panel size, we excluded FPs who identified urgent/emergent care or hospital-affiliated practices as their primary practice (hospital outpatient department and academic health center/faculty practice) where continuity patient panels would be uncommon. If a physician registered for more than one exam during the study period, responses from the latest questionnaire were used.
In descriptive analyses, we characterized the sample and calculated the percentages of FPs with a panel size estimate by physician and practice characteristics. Since not all physicians were able to estimate their panel size, we tested the differences between FPs who were and who were not able to estimate their panel size. We also calculated mean panel sizes and SP4PC scores across physician and practice characteristics. The association of having an NP, PA, or both with panel size and SP4PC score was investigated in separate ordinary least squares regression models accounting for all the covariates, with P<0.05 being the benchmark of statistical significance. Only physicians with nonmissing panel size estimates were included in the regression model on panel size. As a sensitivity test, we reestimated the model by excluding physicians with extreme estimates (greater than two standard deviations above the mean). All analyses were conducted in SAS 9.4 (SAS Institute Inc, Cary, NC). The American Academy of Family Physicians Institutional Review Board approved this study.
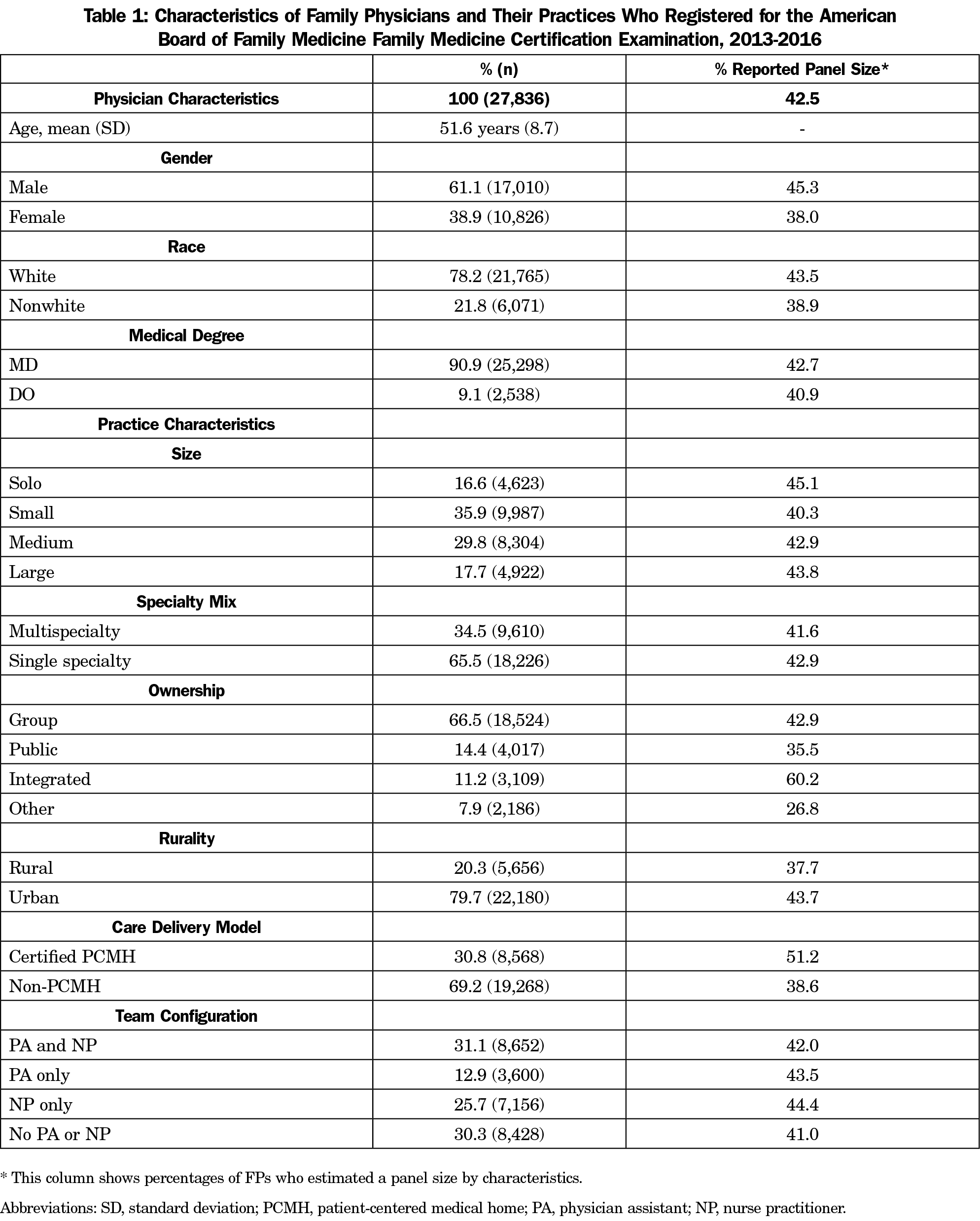
Table 1 displays the characteristics of FPs and their practices. The majority of our sample (n=27,836) were male (61.1%), white (78.2%), and MDs (90.9%). The mean age of the sample was 51.6 years. A majority of FPs were in small or solo, single-specialty, group practices. Neither a PA nor NP was present in 30.3% (n=8,428) of the practices. Of the remaining practices, 25.7% (n=7,156) had NP only, 12.9% (n=3,600) had PA only, and 31.1% (n=8,652) had both. Less than half (42.5%, n=11,830) of the physicians were able to estimate a panel size and those in integrated, urban, and PCMH-certified practices were more likely to provide a panel size estimate. FPs who were not able to estimate their panel size were more likely to work in small, multispecialty, publicly-owned, rural and non-PCMH-certified practices. FPs who identified as male and white were more likely to estimate their panel size than female FPs and FPs whose race was not white, respectively. Complete results of this comparison can be found in the Appendix Table 1.
Table 2 displays the panel size and scope of practice associated with the FP and practice characteristics in our sample. The mean panel size, for those who could estimate a panel size, was 2,263. FPs from small practices reported the largest average panel sizes, while FPs from large practices reported the smallest average panel size (2,504 and 1,888 patients, respectively; P<0.05). FPs from non-PCMH practices reported average patient panels roughly 13% larger than those from PCMHs (P<0.05). Of the various team configurations, panel sizes were the largest among FPs working with PAs only and smallest among FPs working with both PAs and NPs (2,597 and 2,049 patients, respectively; P<0.05).
The mean SP4PC score was 15.3 for all respondents (Table 2). A SP4PC score of 15 corresponds to the provision of 11 (out of 22) scope of practice items captured in the I-SOP Scale.27 A complete list of the 22 scope of practice items can be found in Appendix Table 2. While statistically significant, the degrees of variation in scope scores were small. The largest differences in scope scores by practice characteristics was in ownership type, where FPs who reported being part of group or public ownership practices had higher scope scores than those in integrated or other practices (15.6 and 15.9 vs 14.2 and 13.5, respectively; all P<0.05). FPs working in rural practices or associated with a PCMH had higher scores than their counterparts in urban or non-PCMH practices (16.8 and 15.9 vs 14.9 and 15.0, respectively; all P<0.05). Lastly, scope scores were highest among FPs working with PAs only in their practices and lowest among FPs working with neither PAs nor NPs (15.8 vs 14.8, respectively; P<0.05). The complete list of 22 scope of practice items that were accounted for when generating the scope scores can be found in Appendix Table 2.
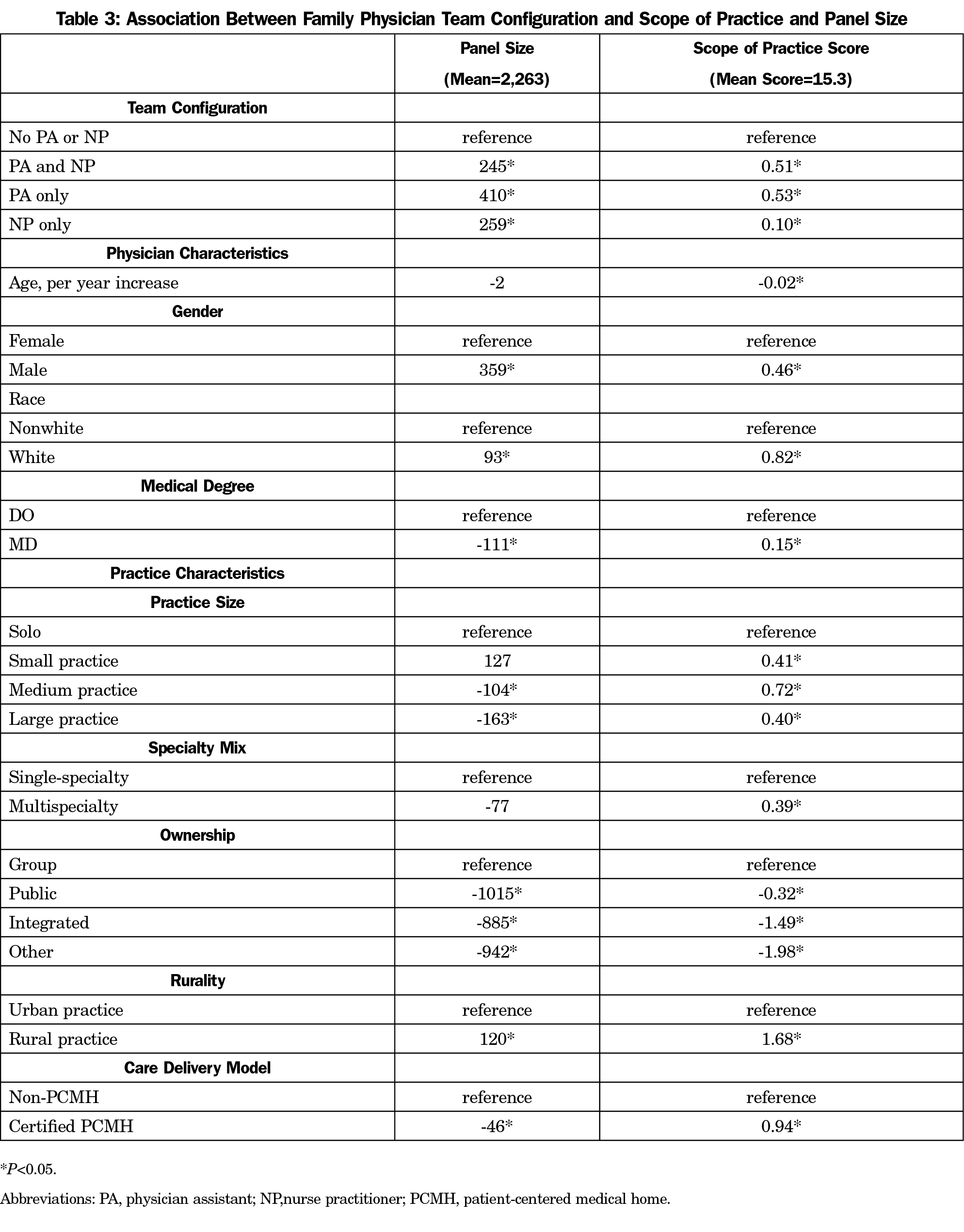
Table 3 contains the results of the ordinary least squares regression models. Accounting for physician and practice characteristics, the presence of a PA and/or NP was associated with significant increases in panel size and scope of practice. Compared to practices with no PA or NP, having PA only was associated with an increased panel size of 410 and scope score of 0.53 (both P<0.05). Having NP only or both PA and NP was associated with a significant yet smaller increase in panel size as well as scope score than having a PA only (259 and 245 for panel size; 0.10 and 0.51 for scope score respectively; all P<0.05). In the sensitivity analysis (Appendix Table 3), the presence of a PA and/or NP remained a significant factor associated with increases in panel size despite the reduced magnitude of its associations with panel size (245 vs 103 for PA and NP; 410 vs 255 for PA only; 259 vs 128 for NP only). Besides the presence of a PA or NP, being male, white, or practicing in a rural location was also consistently associated with increases in both panel size and scope of practice.
We are the first to report on the practice changes of FPs who work with NPs and PAs using a large, current, and representative sample of FPs. This study offered confirmative evidence that variations in practice team configuration were associated with FPs’ patient panel size and scope of practice, suggesting that optimized teams may enable primary care physicians to practice at higher capacity than poorly configured ones. In the context of team-based care, it is critical to make sure that the involvement of NPs and PAs frees practice capacity for otherwise overburdened physicians.29,30 However, the growing evidence base surrounding team-based care has paid little attention to the configuration of primary care teams and its impact on physician team leaders. Consistent with previous studies,3-6 we found substantial involvement of NPs and PAs in FPs’ practice during 2013-2016, suggesting that primary care practices continued to evolve toward team-based models.
This study has two main findings. First, having NPs or PAs in the practice was associated with larger patient panel sizes and a broader scope of practice of FPs than having neither. Increases in patient panel sizes and broadening of scope of practice means that FPs are able to take care of more patients and provide more services, which would be impractical without NPs or PAs sharing responsibilities for patients.18,29,30 This finding not only reassures that FPs, as leaders of primary care teams, are benefiting from working with NPs and PAs, but also that team-based care is an effective strategy to respond to the increase in patient volume as well as the undersupply of primary care physicians. Additionally, studies have shown that increased use of PAs and NPs in primary care practices were associated with lower labor cost per visit.31 This finding is important as our study validated continued trends in FPs increasingly working in team-based care models with NPs and PAs.3-5
Second, PAs seemed to have a stronger enabling effect on FPs’ practice than NPs, and even than PAs and NPs combined. While both share clinical responsibilities with FPs, a stronger association may indicate in general that PAs perform more substitutive than supplemental responsibilities,23,24 which would allow FPs to have larger patient panels and provide more services than would working with NPs. It was unexpected that having both PA and NP in the practice did not garner independent effects of having PA only and having NP only. A possible explanation could be that the delivery of team-based care demands more interaction among team members and essentially more nondirect patient care time from the physician when both PA and NP are present. While highly generalizable to FPs in the United States, these findings do not shed light on the underlying mechanism resulting in the observed differences. One study of older diabetes patients of a large academic physician group found that the level of involvement of NPs and PAs (eg, as supplemental or usual provider of care) was associated with both characteristics of the patients and utilization of services.32 More specific explanations for these differences will require in-depth examination of clinical roles and boundaries of NPs and PAs in variously configured physician-led primary care teams. Aside from the involvement of NPs and PAs in the practice, FPs’ characteristics, practice size, ownership, rurality and PCMH status were all found to influence FPs’ practice to various degrees and in different directions.
Our work advances the literature on scope of practice using a psychometrically-derived global measure instead of using individual practice measures33-36 or an ad hoc scale by simply summing the number of services performed.19,37 This psychometric scale captures the breadth of 22 clinical activities and calculates a comparable score of individual physicians’ scope of practice.27 While the largest adjusted increase in scope score associated with working with only PA (0.53) was smaller than the two-point difference in scope score previously reported between graduating residents and practicing physicians on the same scale,38 the findings are likely still meaningful. When measured by the total number of clinical services provided, increases in the scope of practice of FPs were associated with lower Medicare costs and lower odds of hospitalization.19 Although direct comparisons between the claim-based measure and our scale are difficult, these previous findings suggest that increases in scope of practice measured by our scale may be associated with lower costs of care.
However, a lack of data on whether NPs or PAs worked within the FP’s panel or had their own patient panel is a major limitation of the study, and precluded us from further causal investigations. In the exam registration questionnaire, FPs were asked to indicate whether NPs or PAs work in their primary practice site. While the responses to the question helped us differentiate team configurations, we were unable to determine the nature of the working relationships between NPs or PAs with FPs. Specifically, how clinical responsibilities and boundaries were established in the practice for NPs or PAs relative to FPs was unknown. This qualitative information would offer much-needed insight into the mechanism by which the primary care teams operate. Furthermore, knowledge of the functional roles of NPs and PAs in the practice would allow more granular examinations of the association.
Additionally, all study data were self-reported and collected during the ABFM Family Medicine Certification Examination registration process. As a result, responses to certain questions such as practice size and ownership might be subject to recall bias. Panel size analyses were limited to physicians with a patient panel size estimate, who differed from physicians who were not able to estimate their panel size in both practice and demographic characteristics—some were associated with larger panels while others smaller ones. Consequently, the lack of complete data on panel size might bias the magnitude of the associations. Future studies extracting data from EHRs may resolve this limitation by capturing every physician’s actual patient panel size. Moreover, the ability to estimate a panel size is likely associated with advanced practice features such as patient registries. To lessen the potential confounding, this study adjusted for practices’ PCMH status in the regression analysis.
This study provides the first empirical evidence demonstrating that team-based care involving NPs and PAs was associated with higher practice capacity of primary care physicians. Having NPs or PAs in the practice was associated with an increased patient panel size and a broader scope of practice for FPs, while PAs appeared to enable FPs to take care of more patients and provide more services to a greater degree than NPs. Future studies that evaluate how primary care team members delineate roles, share responsibilities, and set boundaries are needed to better understand the impact of various team configurations on FPs’ practice.
Acknowledgments
Content from this study was presented at the following conferences:
1. North American Primary Care Research Group Annual Meeting, October 24-28, 2015, Cancun, Mexico
2. Academy Health Annual Research Meeting, June 14-16, 2015, Minneapolis, MN, USA
References
- Hofer AN, Abraham JM, Moscovice I. Expansion of coverage under the Patient Protection and Affordable Care Act and primary care utilization. Milbank Q. 2011;89(1):69-89. https://doi.org/10.1111/j.1468-0009.2011.00620.x
- Petterson SM, Liaw WR, Phillips RL Jr, Rabin DL, Meyers DS, Bazemore AW. Projecting US primary care physician workforce needs: 2010-2025. Ann Fam Med. 2012;10(6):503-509. https://doi.org/10.1370/afm.1431
- Peterson LE, Blackburn B, Petterson S, Puffer JC, Bazemore A, Phillips RL. Which family physicians work routinely with nurse practitioners, physician assistants or certified nurse midwives. J Rural Health. 2014;30(3):227-234. https://doi.org/10.1111/jrh.12053
- Bazemore A, Wingrove P, Peterson L, Petterson S. The Diversity of Providers on the Family Medicine Team. J Am Board Fam Med. 2016;29(1):8-9. https://doi.org/10.3122/jabfm.2016.01.150229
- Peterson LE, Phillips RL, Puffer JC, Bazemore A, Petterson S. Most family physicians work routinely with nurse practitioners, physician assistants, or certified nurse midwives. J Am Board Fam Med. 2013;26(3):244-245. https://doi.org/10.3122/jabfm.2013.03.120312
- Peikes DN, Reid RJ, Day TJ, et al. Staffing patterns of primary care practices in the comprehensive primary care initiative. Ann Fam Med. 2014;12(2):142-149. https://doi.org/10.1370/afm.1626
- Mundinger MO, Kane RL, Lenz ER, et al. Primary care outcomes in patients treated by nurse practitioners or physicians: a randomized trial. JAMA. 2000;283(1):59-68. https://doi.org/10.1001/jama.283.1.59
- Ohman-Strickland PA, Orzano AJ, Hudson SV, et al. Quality of diabetes care in family medicine practices: influence of nurse-practitioners and physician’s assistants. Ann Fam Med. 2008;6(1):14-22. https://doi.org/10.1370/afm.758
- Lenz ER, Mundinger MO, Kane RL, Hopkins SC, Lin SX. Primary care outcomes in patients treated by nurse practitioners or physicians: two-year follow-up. Med Care Res Rev. 2004;61(3):332-351. https://doi.org/10.1177/1077558704266821
- Everett CM, Schumacher JR, Wright A, Smith MA. Physician assistants and nurse practitioners as a usual source of care. J Rural Health. 2009;25(4):407-414. https://doi.org/10.1111/j.1748-0361.2009.00252.x
- Mafi JN, Wee CC, Davis RB, Landon BE. Comparing Use of Low-Value Health Care Services Among U.S. Advanced Practice Clinicians and Physicians. Ann Intern Med. 2016;165(4):237-244. https://doi.org/10.7326/M15-2152
- Everett CM, Morgan P, Jackson GL. Patient characteristics associated with primary care PA and APRN roles. JAAPA. 2016;29(12):1-6. https://doi.org/10.1097/01.JAA.0000508217.65992.72
- Bodenheimer TS, Smith MD. Primary care: proposed solutions to the physician shortage without training more physicians. Health Aff (Millwood). 2013;32(11):1881-1886. https://doi.org/10.1377/hlthaff.2013.0234
- Murray M, Davies M, Boushon B. Panel size: how many patients can one doctor manage? Fam Pract Manag. 2007;14(4):44-51.
- Grumbach K, Olayiwola JN. Patient empanelment: the importance of understanding who is at home in the medical home. J Am Board Fam Med. 2015;28(2):170-172. https://doi.org/10.3122/jabfm.2015.02.150011
- Peterson LE, Cochrane A, Bazemore A, Baxley E, Phillips RL Jr. Only one third of family physicians can estimate their patient panel size. J Am Board Fam Med. 2015;28(2):173-174. https://doi.org/10.3122/jabfm.2015.02.140276
- Altschuler J, Margolius D, Bodenheimer T, Grumbach K. Estimating a reasonable patient panel size for primary care physicians with team-based task delegation. Ann Fam Med. 2012;10(5):396-400. https://doi.org/10.1370/afm.1400
- Raffoul M, Moore M, Kamerow D, Bazemore A. A Primary Care Panel Size of 2500 Is neither Accurate nor Reasonable. J Am Board Fam Med. 2016;29(4):496-499. https://doi.org/10.3122/jabfm.2016.04.150317
- Bazemore A, Petterson S, Peterson LE, Phillips RL Jr. More Comprehensive Care Among Family Physicians is Associated with Lower Costs and Fewer Hospitalizations. Ann Fam Med. 2015;13(3):206-213. https://doi.org/10.1370/afm.1787
- Tong ST, Makaroff LA, Xierali IM, et al. Proportion of family physicians providing maternity care continues to decline. J Am Board Fam Med. 2012;25(3):270-271. https://doi.org/10.3122/jabfm.2012.03.110256
- Bazemore AW, Makaroff LA, Puffer JC, et al. Declining numbers of family physicians are caring for children. J Am Board Fam Med. 2012;25(2):139-140. https://doi.org/10.3122/jabfm.2012.02.110203
- Petterson S, Peterson L, Phillips RL, et al. One in fifteen family physicians principally provide emergency or urgent care. J Am Board Fam Med. 2014;27(4):447-448. https://doi.org/10.3122/jabfm.2014.04.130307
- Starfield B. Roles and functions of non-physician practitioners in primary care. In: Clawson DO, M, ed. The Roles of Physician Assistants and Nurse Practitioners. Washington, DC: Association of Academic Health Centers; 1993:11-20.
- Hooker RS, McCaig LF. Use of physician assistants and nurse practitioners in primary care, 1995-1999. Health Aff (Millwood). 2001;20(4):231-238. https://doi.org/10.1377/hlthaff.20.4.231
- Green LV, Savin S, Lu Y. Primary care physician shortages could be eliminated through use of teams, nonphysicians, and electronic communication. Health Aff (Millwood). 2013;32(1):11-19. https://doi.org/10.1377/hlthaff.2012.1086
- Rittenhouse DR, Shortell SM. The patient-centered medical home: will it stand the test of health reform? JAMA. 2009;301(19):2038-2040. https://doi.org/10.1001/jama.2009.691
- O’Neill T, Peabody MR, Blackburn BE, Peterson LE. Creating the Individual Scope of Practice (I-SOP) scale. J Appl Meas. 2014;15(3):227-239.
- WWAMI Rural Health Research Center. Rural-Urban Commuting Area Codes (RUCAs). http://depts.washington.edu/uwruca/. Accessed March, 2017.
- Yarnall KS, Østbye T, Krause KM, Pollak KI, Gradison M, Michener JL. Family physicians as team leaders: “time” to share the care. Prev Chronic Dis. 2009;6(2):A59.
- Alexander GC, Kurlander J, Wynia MK. Physicians in retainer (“concierge”) practice. A national survey of physician, patient, and practice characteristics. J Gen Intern Med. 2005;20(12):1079-1083. https://doi.org/10.1111/j.1525-1497.2005.0233.x
- Everett CM, Thorpe CT, Palta M, Carayon P, Gilchrist VJ, Smith MA. Division of primary care services between physicians, physician assistants, and nurse practitioners for older patients with diabetes. Med Care Res Rev. 2013;70(5):531-541. https://doi.org/10.1177/1077558713495453
- Carek PJ, Diaz V, Dickerson LM, Peterson L, Johnson S. Preparation for practice in family medicine: before and after duty hours. Fam Med. 2012;44(8):539-544.
- Kim S, Phillips WR, Stevens NG. Family practice training over the first 26 years: a cross-sectional survey of graduates of the University of Washington Family Practice Residency Network. Acad Med. 2003;78(9):918-925. https://doi.org/10.1097/00001888-200309000-00017
- Ringdahl E, Delzell JE Jr, Kruse RL. Changing practice patterns of family medicine graduates: a comparison of alumni surveys from 1998 to 2004. J Am Board Fam Med. 2006;19(4):404-412. https://doi.org/10.3122/jabfm.19.4.404
- Chen FM, Huntington J, Kim S, Phillips WR, Stevens NG. Prepared but not practicing: declining pregnancy care among recent family medicine residency graduates. Fam Med. 2006;38(6):423-426.
- Wong E, Stewart M. Predicting the scope of practice of family physicians. Can Fam Physician. 2010;56(6):e219-e225.
- Coutinho AJ, Cochrane A, Stelter K, Phillips RL Jr, Peterson LE. Comparison of Intended Scope of Practice for Family Medicine Residents With Reported Scope of Practice Among Practicing Family Physicians. JAMA. 2015;314(22):2364-2372. https://doi.org/10.1001/jama.2015.13734




There are no comments for this article.