Background and Objectives: Group medical visits (GMV) have been shown to improve clinical outcomes and patient satisfaction and are included as a new tool in the patient-centered medical home (PCMH). The capacity for and interest in developing GMV skills in family medicine residency have not been assessed. This study aims to describe the extent of existing training in GMV as well as attitudes toward and barriers to this training.
Methods: The Council of Academic Family Medicine Educational Research Alliance (CERA) sent a survey in the fall of 2015 to all US family medicine residency program directors (PDs) containing questions about the status of GMV training for their residents.
Results: The survey response rate was 53%. Fifty-nine percent of program director respondents report access to GMV and 61% note some form of training in this model of care. Seventy-nine percent of respondents indicate that GMV training is important for residents. Multiple barriers exist to optimizing GMV as part of current family medicine training.
Conclusions: A majority of family medicine PD respondents report both access to and curriculum for GMV. While program directors endorse this practice model as an important element in resident training, they acknowledge challenges that may limit its availability. Opportunities to better understand and overcome barriers may increase programs’ capacity to deliver GMV skills.
Group medical visits (GMV) provide a patient-centered approach to improved engagement in behavior change while increasing efficiency in the delivery of guideline-driven care.1 In a typical chronic disease model for GMV (also referred to as shared medical appointments [SMA]), eight to twelve patients with a common condition (eg, diabetes) share an appointment with a provider using facilitated interactions to foster enhanced education, the development of problem-solving skills, and peer support.2 GMV are described as part of the Patient-Centered Medical Home (PCMH). The literature on group visits in primary care supports associated benefits including improved clinical outcomes, increased patient satisfaction, increased provider satisfaction, and decreased medical costs.3-7 The incorporation of GMV into family medicine residency training is evidenced by steady growth in the number of scholarly presentations on this topic at national professional meetings.8 Additionally, residency experiences with GMV have been described in the family medicine graduate medical education (GME) literature.9,10,11,12,13
Reliable measurement of primary care practices’ use of GMV is hampered by the lack of any unique billing code for this service. Trends in the prevalence of this model of care are unclear as group visits are typically billed using standard individual procedural codes rendering the service indistinguishable from traditional care.2 The Accreditation Council for Graduate Medical Education (ACGME) neither requires nor assesses the status of GMV training as a curricular element.14 Family medicine residents’ exposure to GMV in training has not been explored. The objectives of this study were: (1) to assess family medicine residents’ exposure to GMV, (2) to report existing approaches to GMV training for family medicine residents, and (3) to describe perceived challenges to the use of GMV in residency training.
The Council of Academic Family Medicine Educational Research Alliance (CERA) conducts biannual cross-sectional surveys of all US family medicine residency program directors; its methods have been described elsewhere.15 The authors developed GMV questions for inclusion in the 2015 survey. Items were reviewed by the CERA steering committee and pretested with family medicine educators who were not part of the target population. The Wake Forest School of Medicine and the American Academy of Family Physicians (AAFP) Institutional Review Boards approved the project. Data were collected from July to August of 2015.
An invitation to complete the CERA survey, including a link to the survey itself, was distributed electronically to program directors (PDs) representing 473 unique ACGME-accredited US family medicine residency programs. Three follow-up emails were sent to nonrespondents at 2-week intervals from the original invitation in 2015.
The following definition of GMV was provided in the survey:
GMV are visits at which a group of patients [are] seen collectively in a shared space by a medical provider for a billable medical service that includes expanded support and education.
Program directors were directed to consider CenteringPregnancy, a specific model of GMV for prenatal care, as one type of GMV for the purposes of this survey.16 To fully account for resident exposure to GMV, program directors were asked to report if GMV were offered at the primary residency clinic (on site) and/or at any other training locations (off site). Separate items addressed whether CenteringPregnancy was offered either on or off site. Program director respondents who indicated that GMV were offered neither on nor off site, but whose programs offered CenteringPregnancy GMV either on or off site, were considered to have GMV access for purposes of the analysis. Two items addressed program director attitudes regarding the importance of GMV. Among programs not offering GMV, plans to develop or implement GMV were assessed. Three items examined formats programs used to train residents in GMV. The degree to which five potential barriers affected GMV capacity at the program was assessed using a Likert scale without regard to the status of GMV access for the program’s residents.
Analysis
Data were analyzed using SPSS version 24 (IBM Corp, 2016. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp). Univariate analyses provided descriptive statistics for all variables. Bivariate analysis via χ2 compared demographic and attitudinal data to presence or absence of GMV.
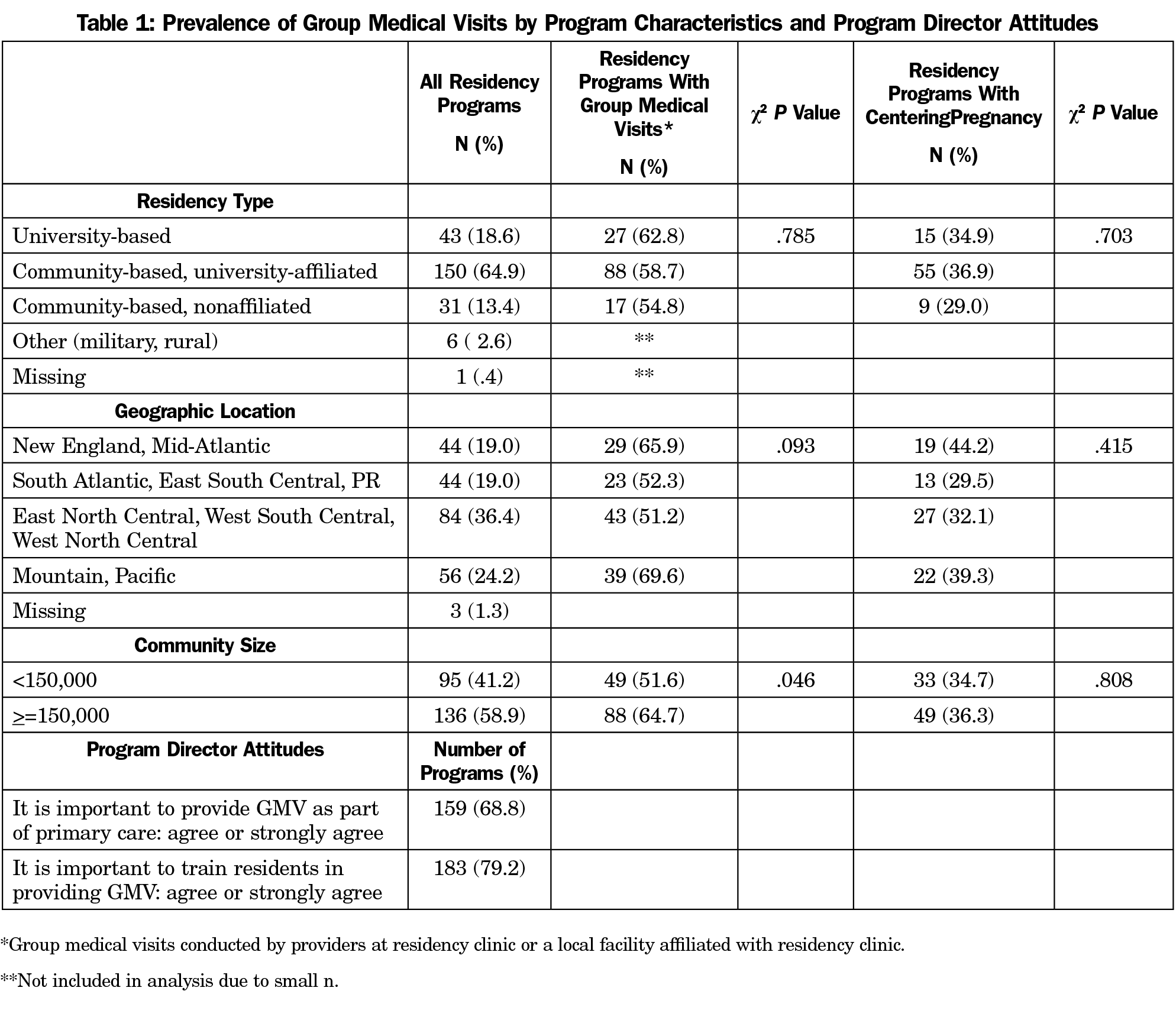
The overall response rate among family medicine program directors was 53% (252/473). Ninety-two percent of respondents (231/252) completed 10 or more of 15 GMV items. Of these 231 respondents, the majority (65%) were community based/university affiliated. All regions of the country were represented, and 59% were from communities of more than 150,000 people (Table 1).
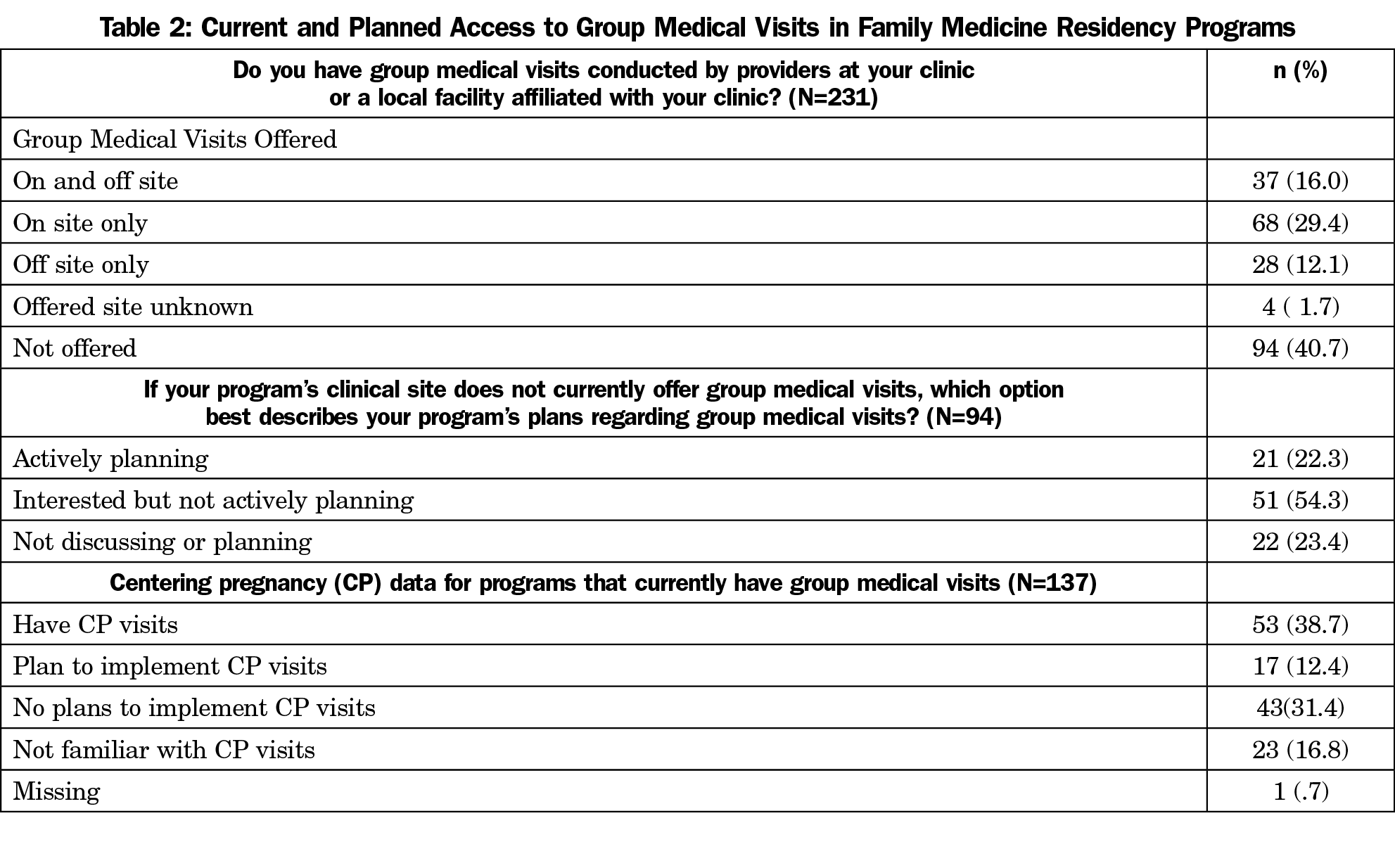
One hundred thirty-seven (59%) program directors indicated that GMV were offered on site, at one or more local facilities associated with their site or clinic, or both (Table 2). Among the 94 (41%) respondents without current access to GMV models of practice, 22% were actively planning to implement GMV, 54% were interested in developing GMV, and 23% were not planning to implement GMV. Of 137 respondents reporting GMV, 39% offered CenteringPregnancy at their site and/or a local affiliated facility, 12% had plans to implement CenteringPregnancy, and 31% had no plans to start CenteringPregnancy. Seventeen percent were not familiar with this group prenatal model of care (Table 2). Residencies from larger communities were more likely to provide GMV (Table 1).
Program Director Attitudes and Curricular Types
One hundred fifty-nine (68.8%) program director respondents agreed or strongly agreed that GMV should be provided as a component of primary care; 183 (79.2%) agreed or strongly agreed that it is important to train family medicine residents in the GMV model of care (Table 1).
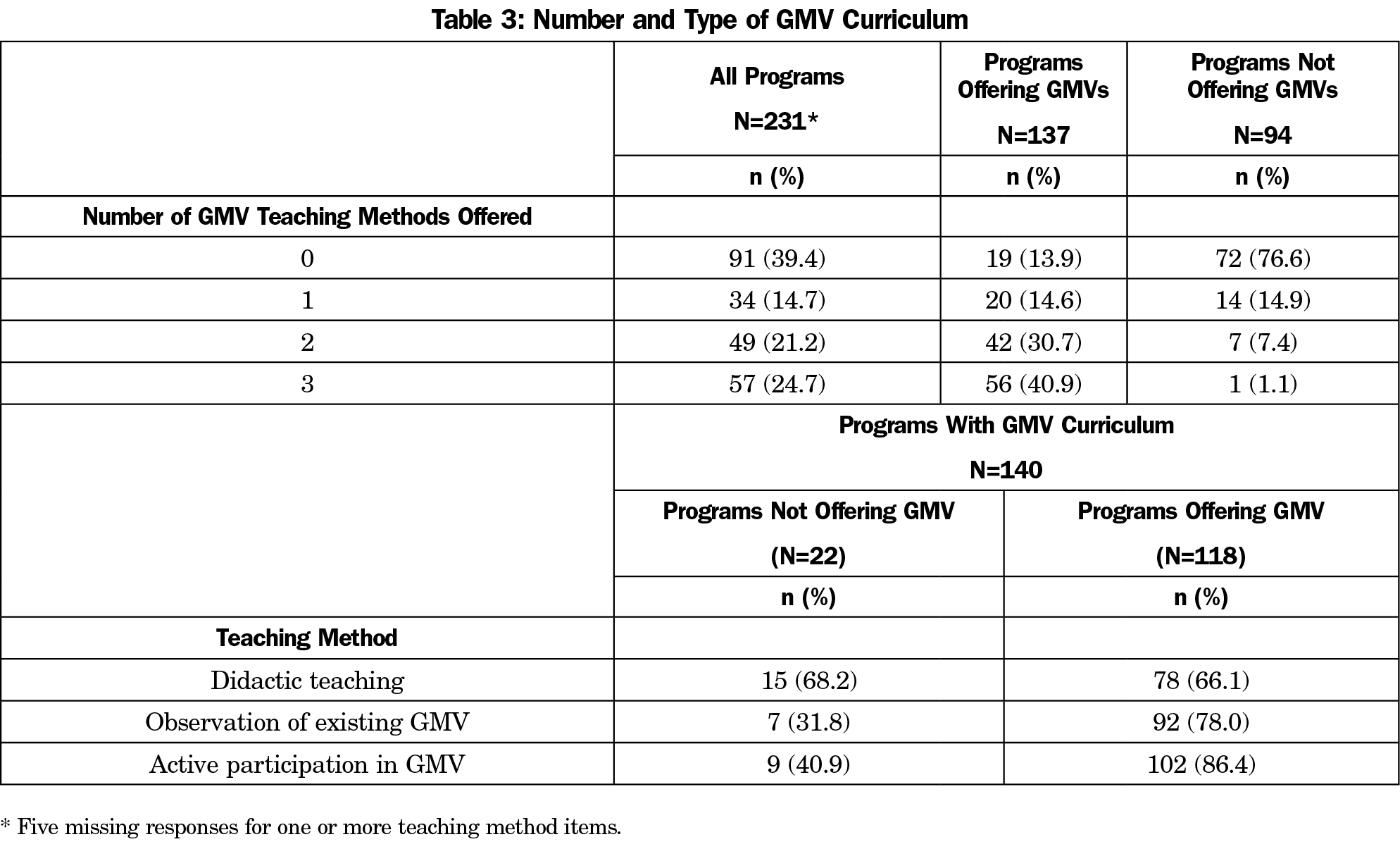
The survey assessed the availability of three different and nonmutually exclusive forms of resident curricular experience with GMV. Of 231 respondents, 91 (39.4%) reported a lack of GMV resident curriculum. Thirty-four (14.7%) PD respondents reported that their program provided one training method, and 106 (45.9%) programs provided more than one form of GMV training. Few respondents from programs with GMV access reported lacking GMV curriculum (19 [13.9%]). Among programs that both offer GMV and have GMV curriculum, respondents reported high levels of didactic (66.1%), observational (78.0%), and participatory (86.4%) curricular methods. Among programs that offer GMV curriculum but lack GMV access, fewer than half of respondents reported observation or participation as GMV curricular elements (31.8% and 40.9%, respectively; Table 3).
Barriers to GMV
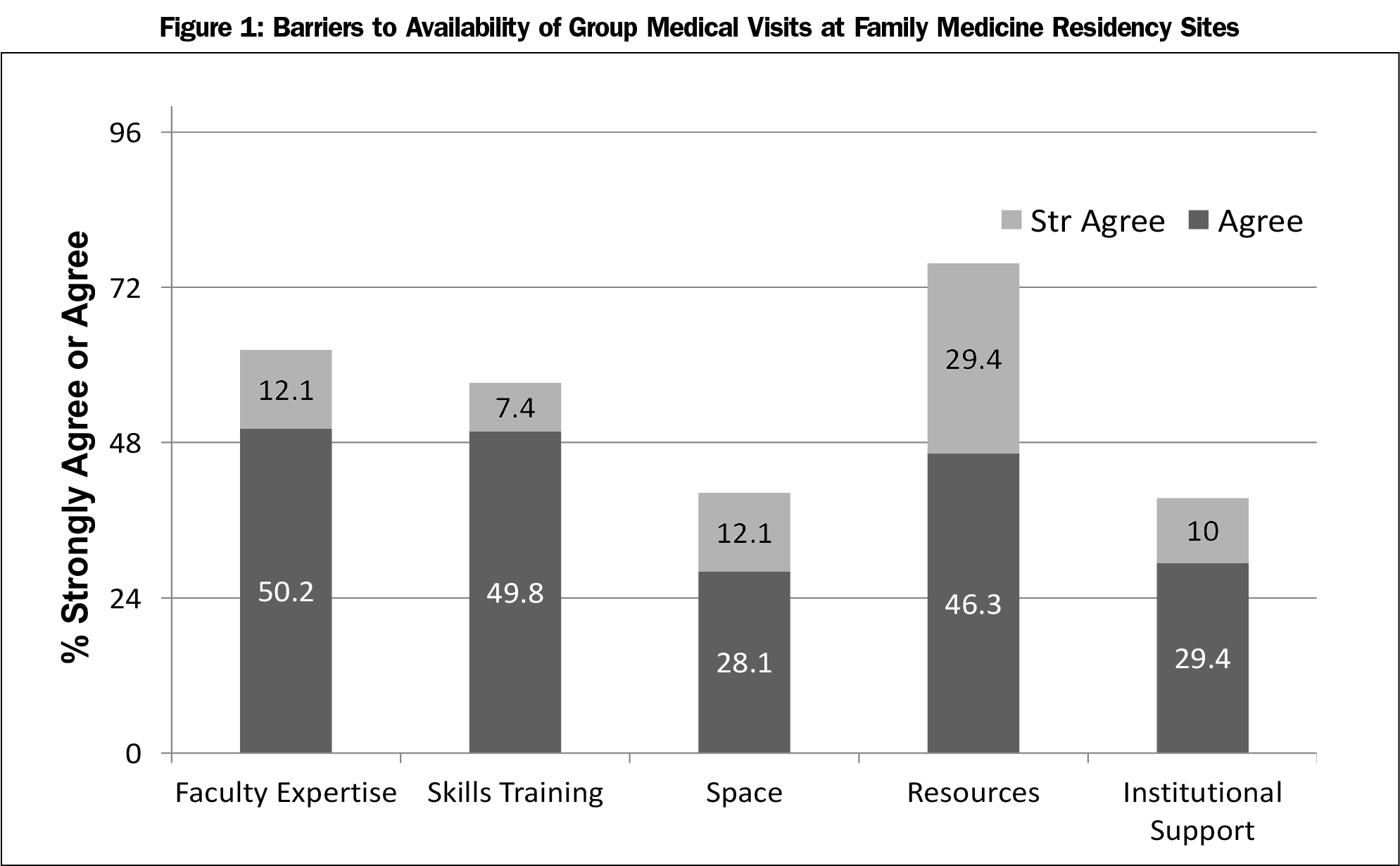
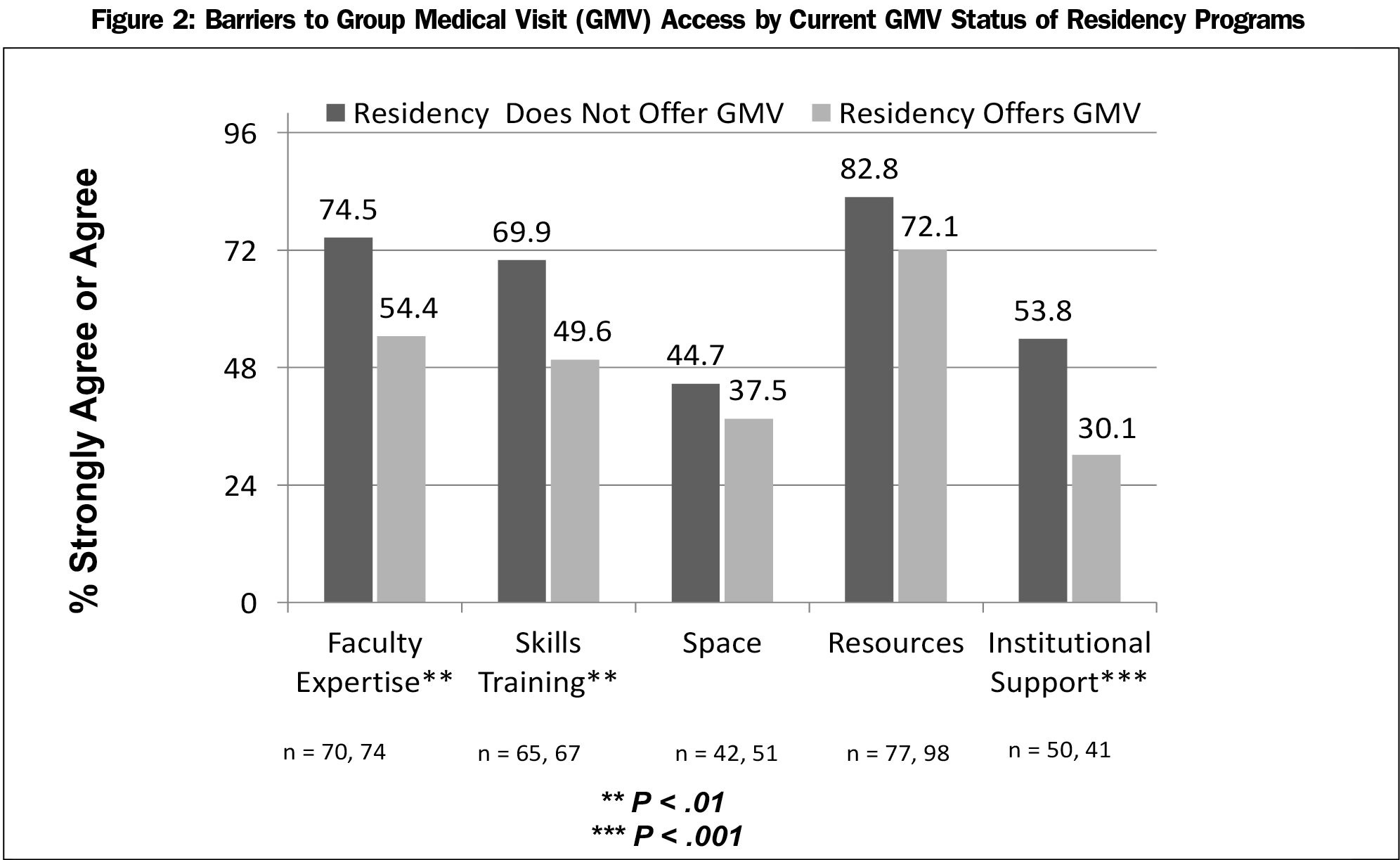
Respondents completed a set of survey items, without regard to program GMV status, rating the degree to which barriers affected GMV availability. They identified lack of resources, such as required time/funding (75.7%) to support the development and coordination of GMV, as a leading barrier. Additionally, a majority of respondents reported lack of faculty expertise to implement and run GMV (62.3%), and lack of access to specific GMV skills such as facilitation, as barriers to GMV capacity at their sites. Lack of adequate space for GMV and lack of institutional support were identified as barriers to providing GMV at respondents’ sites least frequently (Figure 1). Further analysis of barriers by GMV status reveals that respondents from programs without GMV were significantly more likely to report the lack of faculty expertise, skills training, and institutional support as barriers than those from programs with established GMV (Figure 2).
This is the first assessment of training in GMV among family medicine residency programs. Our data suggest that, while GMV are beginning to be incorporated into family medicine training, almost half of existing programs have not yet developed this capacity. Forty-one percent of programs lack GMV access in their practice locations, and 40.3% of programs have no curriculum for GMV training. Many programs are unable to provide active resident participation in GMV as part of existing curriculum. Yet, program directors endorse GMV as an important practice tool and support resident training in this model of care. Further, three-fourths of programs with no current GMV capacity for training endorse either interest in or intent to implement GMV, suggesting confidence in the potential of GMV in primary care.
Further understanding of barriers to GMV availability will be required to support effective needs assessment (Figure 2). Our data suggest that barriers limit both the development of new GMV capacity and full optimization of existing GMV opportunities. Among sites with existing GMV, it is possible that perceived barriers limit the achievement of desired scope and scale of their group visit programs. Respondents cite lack of resources (time/funding) most frequently as a barrier to developing and coordinating GMV at their sites. Instituting GMV into existing clinical sites requires investment in key process changes including (a) the identification and modification of GMV patient education tools (eg, diabetes education), (b) adjustment of scheduling systems for both providers and patients to support shared group appointments, and (c) the development of a recruiting strategy to introduce patients to a new and different clinical service. This work exists outside of established residency faculty and staff responsibilities and thus represents added effort requiring initial financial support. Understanding and quantifying the required resources for both start up and maintenance of GMV in residency will aid in the search for support strategies.
Barriers including lack of faculty expertise and insufficient group care skills outranked concerns around space and institutional support. A comparison of those programs with and without GMV suggests that the presence of institutional support, faculty GMV expertise, and GMV skills and training are favorably associated with the implementation of GMV. Notably, fully half of respondents reporting current GMV access in residency claim active or planned CenteringPregnancy as part of their GMV programming. CenteringPregnancy is unique as a trademarked group visit model characterized by clearly defined elements and curriculum, an established training and certification process, and a growing evidence base for positive outcomes.7,17-20 Programs with funding (historically from stakeholders such as March of Dimes) to support CenteringPregnancy benefit from available consultation on the process of implementation as well as training in key skills for GMV providers such as facilitation of group care.16 Given that few current family medicine residency faculty are likely to have experience with implementing and/or leading group medical visits, the availability of this support may explain the sizeable presence of this particular GMV model in family medicine training to date.
Consideration of mechanisms to expand access to this and other methods of GMV skills training and support within family medicine is warranted. Organizations committed to faculty development and practice transformation in primary care could leverage opportunities at established live forums (eg, Society of Teachers of Family Medicine (STFM) and AAFP to substantially increase access to GMV training and support. Providers could use existing continuing medical education funding to access formal GMV skills training thus reducing programs’ resource pressure. Learning collaboratives on local and regional levels may provide effective environments for determining and disseminating best practices.21-23 Primary care organizations, payers, and health system administrators can be included as partners in the development and testing of proven support strategies.
Future areas for GMV research include (a) an expanded needs assessment to better understand challenges to the development of GMV training, (b) the development and validation of new measures to assess faculty and residents’ effectiveness in providing group medical visits, (c) clinical and patient experience outcomes assessment and associated key GMV processes, and (d) impact on provider satisfaction. Trends toward value-based reimbursement schemes will allow and encourage exploration of optimal GMV applications in primary care. On a national scale, the family medicine GME community could seize opportunities for leadership in the development and deployment of GMV in primary care by convening appropriate stakeholders to (a) define and standardize optimal GMV models, (b) guide research efforts to provide meaningful outcomes data, and (c) lobby for new specific billing codes tied to enhanced reimbursement for this service.
There are several limitations to this study. The overall response rate for the survey was 53.3%, raising the possibility of bias, though responses were well distributed across residency settings and geographic regions. The lack of clear definitions in the literature regarding GMV in clinical care could lead to ambiguity in understanding of survey questions. Additionally, the CERA survey mechanism limited access to data on details such as type, scope, and duration of GMV experiences, introducing the potential for misinterpretation. Further, respondents comprise program directors as a sole source of input. Other important stakeholders in residency education including faculty and residents may have different perspectives on the role of GMV in practice and training as well as the nature of and degree to which barriers affect GMV availability.
Family medicine residencies today have a responsibility to teach next-generation providers promising new models of care. Despite a recognized role for GMV in family medicine training, our results suggest that just under half of programs lack the capacity for this training. Residency programs face the challenge of developing innovations like GMV while simultaneously transforming themselves into sustainable PCMH practices; we are building the airplane while flying it.24-25 The incorporation of GMV experience into family residency training is feasible and effective. Enhancing GMV capacity in training creates a pipeline of skilled and experienced providers prepared for PCMH practice with new care models to meet patient and system needs. Our survey results present a quantifiable snapshot of existing GMV programming and may provide a baseline from which to monitor the evolution of GMV training in residency as a promising element of the PCMH toolkit.
To join STFM CONNECT go to https://connect.stfm.org/home, for STFM members only. To join the STFM Group Medical Visits Special Project Team, update your connections by going to the “My Connections” section of your STFM profile and modify your selections.
Acknowledgments
The authors express their gratitude to Dr Kurt Kroenke, who helped refining the survey questions.
This study was presented at the 2017 STFM Annual Spring Conference in San Diego, CA, May 5-9, 2017.
References
- Burke RE, Ferrara SA, Fuller AM, Kelderhouse JM, Ferrara LR. The effectiveness of group medical visits on diabetes mellitus type 2 (dm2) specific outcomes in adults: a systematic review. JBI Library Syst Rev. 2011;9(23):833-885. https://doi.org/10.11124/01938924-201109230-00001
- Burke RE, O’Grady ET. Group visits hold great potential for improving diabetes care and outcomes, but best practices must be developed. Health Aff (Millwood). 2012;31(1):103-109. https://doi.org/10.1377/hlthaff.2011.0913
- Jaber R, Braksmajer A, Trilling JS. Group visits: a qualitative review of current research. J Am Board Fam Med. 2006;19(3):276-290. https://doi.org/10.3122/jabfm.19.3.276
- Deakin T, McShane CE, Cade JE, Williams RD. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2005;2(2):CD003417. https://doi.org/10.1002/14651858.CD003417.pub2
- Simmons C, Kapustin JF. Diabetes group visits: an alternative to managing chronic disease outcomes. J Nurse Pract. 2011;7(8):671-679. https://doi.org/10.1016/j.nurpra.2010.12.002
- Riley SB, Marshall ES. Group visits in diabetes care: a systematic review. Diabetes Educ. 2010;36(6):936-944. https://doi.org/10.1177/0145721710385013
- Ickovics JR, Kershaw TS, Westdahl C, et al. Group prenatal care and perinatal outcomes: a randomized controlled trial. Obstet Gynecol. 2007;110(2 Pt 1):330-339. https://doi.org/10.1097/01.AOG.0000275284.24298.23
- Society of Teachers of Family Medicine. 2017 Annual Spring Conference Session Search Results: “Group Medical Visits.” http://www.stfm.org/Conferences/AnnualSpringConference/PastConferences/2017AnnualSpringConference?language=en-US&m=0&s=group%2520medical%2520visits&p=0. Accessed March 22, 2018.
- Barr WB, Aslam S, Levin M. Evaluation of a group prenatal care-based curriculum in a family medicine residency. Fam Med. 2011;43(10):712-717.
- Kolb KH, Picklesimer AH, Covington-Kolb S, Hines L. Centering pregnancy electives: a case study in the shift toward student-centered learning in medical education. J S C Med Assoc. 2012;108(4):103-105.
- Page C, Reid A, Andrews L, Steiner J. Evaluation of prenatal and pediatric group visits in a residency training program. Fam Med. 2013;45(5):349-353.
- Goldberg A, Rickler KS, Sullivan G, Nothnagle M. Putting residents in the driver’s seat: a new approach to teaching group medical visits. Fam Med. 2012;44(6):431-435.
- Mittal P. Centering parenting: pilot implementation of a group model for teaching family medicine residents well-child care. Perm J. 2011;15(4):40-41. https://doi.org/10.7812/TPP/11-102
- http://www.acgme.org/What-We-Do/Accreditation/Common-Program-Requirements. Accessed March 22, 2018.
- Mainous AG III, Seehusen D, Shokar N. CAFM Educational Research Alliance (CERA) 2011 Residency Director survey: background, methods, and respondent characteristics. Fam Med. 2012;44(10):691-693.
- Centering Healthcare Institute. CenteringPregnancy. https://www.centeringhealthcare.org/what-we-do/centering-pregnancy. Accessed March 22, 2018.
- Carter EB, Temming LA, Akin J, et al. Group prenatal pare compared with traditional prenatal care: a systematic review and meta-analysis. Obstet Gynecol. 2016;128(3):551-561. https://doi.org/10.1097/AOG.0000000000001560
- Hale N, Picklesimer AH, Billings DL, Covington-Kolb S. The impact of Centering Pregnancy Group Prenatal Care on postpartum family planning. Am J Obstet Gynecol. 2014;210(1):50.e1-50.e7. https://doi.org/10.1016/j.ajog.2013.09.001
- Gareau S, Lòpez-De Fede A, Loudermilk BL, et al. Group prenatal care results in Medicaid savings with better outcomes: a propensity score analysis of CenteringPregnancy participation in South Carolina. Matern Child Health J. 2016;20(7):1384-1393. https://doi.org/10.1007/s10995-016-1935-y
- McNeil DA, Vekved M, Dolan SM, Siever J, Horn S, Tough SC. A qualitative study of the experience of CenteringPregnancy group prenatal care for physicians. BMC Pregnancy Childbirth. 2013;13(suppl 1):S6. https://doi.org/10.1186/1471-2393-13-S1-S6
- Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573-576. https://doi.org/10.1370/afm.1713
- Bodenheimer T, Gupta R, Dube K, et al. High-Functioning Primary Care Residency Clinics: Building Blocks for Providing Excellent Care and Training. Washington, DC: Association of American Medical Colleges; 2016. https://www.aamc.org/download/474510/data/aamc-ucsfprimarycareresidencyinnovationreport.pdf. Accessed March 26, 2018.
- Nutting PA, Crabtree BF, Miller WL, Stange KC, Stewart E, Jaén C. Transforming physician practices to patient-centered medical homes: lessons from the national demonstration project. Health Aff (Millwood). 2011;30(3):439-445. https://doi.org/10.1377/hlthaff.2010.0159
- Cronholm PF, Klusaritz H, Nguyen GT, et al. Resident engagement in the patient-centered medical home. Fam Med. 2016;48(8):603-612.
- Nutting PA, Crabtree BF, Stewart EE, et al. Effect of facilitation on practice outcomes in the National Demonstration Project model of the patient-centered medical home. Ann Fam Med. 2010;8(suppl 1):S33-S44, S92. https://doi.org/10.1370/afm.1119



There are no comments for this article.