Background and Objectives: “Forward feeding” is defined as the sharing of information regarding learner behaviors and performance outside of formal institutional committee structures. The purpose of this study was to establish baseline opinions and policies of forward feeding in family medicine residency programs.
Methods: Data for this study were obtained as part of the 2015 CERA Program Directors Fall Survey. Program directors indicated whether they felt that faculty should and do engage in forward feeding. Respondents were asked to rate the importance of various types of information about learners (academic performance, clinical performance, professionalism, physical health, and mental health), reasons for promoting, and concerns regarding forward feeding on a 5-point Likert scale.
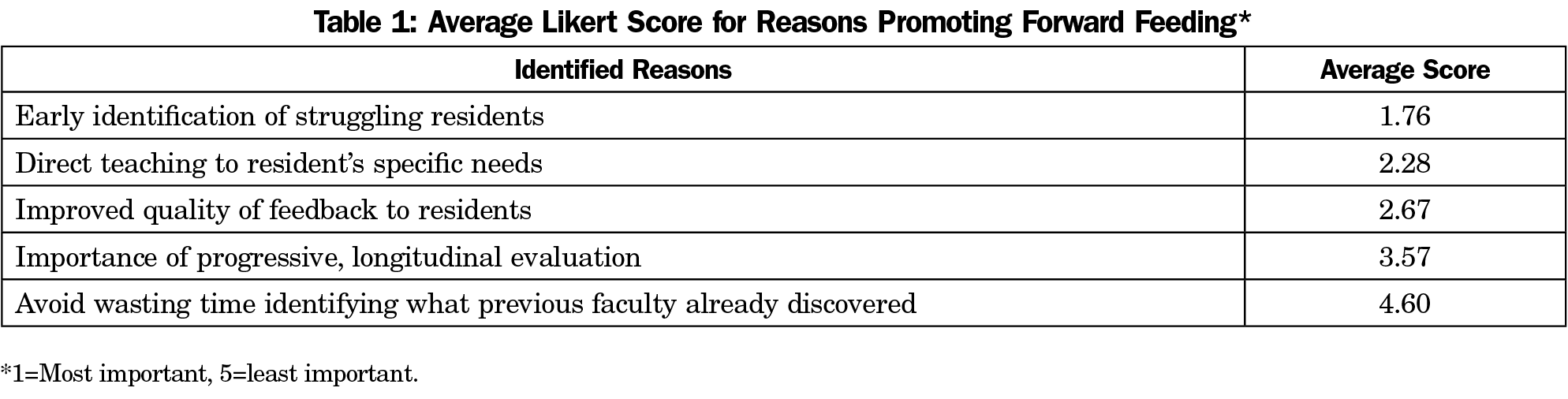
Results: The overall response rate was 49% (227/461). Most agreed that faculty should (87%) and do (83%) engage in forward feeding. Concerns regarding professionalism and clinical performance were reported as most important to share. The most important reason identified for forward feeding was the early identification of struggling residents, followed by the ability to direct teaching to the resident’s specific needs, and improving the quality of feedback. Fear of creating bias was the most commonly cited concern for engaging in forward feeding, followed by fear of violating confidentiality and difficulty maintaining confidentiality. Fear of litigation was the least common concern.
Conclusions: Despite concerns, the majority of program directors feel that faculty should and do engage in forward feeding. Our study confirms the importance of clinical performance and professionalism as two important themes of information shared by attendings about residents.
Efforts to move medical education toward competency-based outcomes have increased under the guidance of the Accreditation Council of Graduate Medical Education (ACGME).1 The ACGME Milestones are competency-based developmental outcomes (eg, knowledge, skills, attitudes, and performance) that residents demonstrate progressively from the beginning of their education through graduation to the unsupervised practice of their chosen specialties.2 However, discrete faculty assessments of resident progress, while an important source of data, do not automatically create a comprehensive narrative about any particular resident’s movement toward achieving required Milestones. “Forward feeding” is defined as the sharing of information regarding learner behaviors and performance outside of formal institutional committee structures.3-6 This has been suggested as one method to contribute to a more comprehensive view of learner competency.3
The advantages and disadvantages of forward-feeding have previously focused primarily on undergraduate medical education (UME) and clerkship performance. As early as 1979, the Association of American Medical Colleges’ Clinical Evaluation Program voiced concern regarding the absence of information shared about students between rotations and the subsequent lack of early identification of struggling students.7 A decade later, Generalists in Medical Education unanimously proposed that some degree of information should be shared under certain circumstances and encouraged that individual institutions make students central to this process to minimize arbitrary and capricious prejudice.8 However, a 1998 survey of medical school deans found that only 56% of responding institutions had written policies outlining guidelines for sharing assessment information about students. Only 35% had policies that allowed for sharing of information regarding academic performance or professional conduct.9
The two largest studies to date on the opinions and policies regarding forward feeding in UME are the 2006 annual Clerkship Directors in Internal Medicine Survey and the 2013 Council of Academic Family Medicine Educational Research Alliance (CERA) survey of family medicine clerkship directors.4,10 In these studies, 51% of internal medicine, and 57% of family medicine clerkship directors who responded indicated that they routinely share information regarding struggling students with other educators outside of formal medical school committees. Both studies revealed similar concerns regarding forward feeding, including concerns for student privacy, fear of creating bias, and fear of litigation.4,10 Three factors favored the sharing of information: the need to provide a supportive educational environment through guidance and mentorship, the need for early identification of struggling students, and the importance of viewing medical education as a continuum.10 Only one in ten responding institutions had formal written policies about forward feeding.10 A similar number specifically prohibited individuals from discussing student difficulties with other faculty.10
While opinions regarding forward-feeding in UME have been published, there is little, if any, research evaluating the opinions and policies in graduate medical education (GME). The purpose of this study was therefore to establish a baseline regarding opinions and policies of forward feeding in postgraduate family medicine training programs. Forward feeding has the potential to allow residency programs to identify subtle deficiencies in a learner’s performance that may only be visible over time with repeated observations from many observers. Additionally, use of forward feeding can provide faculty with a broader and deeper understanding of a resident’s background, performance, and learning needs to facilitate improved learning.
Data for this study were obtained as part of the 2015 CERA Program Directors Fall Survey, which is designed as an omnibus survey incorporating several distinct subprojects. CERA is a joint initiative of four major academic family medicine organizations (Society of Teachers of Family Medicine, North American Primary Care Research Group, Association of Departments of Family Medicine, and Association of Family Medicine Residency Directors [AFMRD]). The methods of CERA survey design and implementation have been described previously.11 The American Academy of Family Physicians Institutional Review Board approved this project in December 2015.
The CERA Program Director Survey is distributed twice a year to all ACGME-accredited US family medicine residency program directors as identified by the AFMRD. CERA administered the survey to 461 identified program directors from December 14, 2015 through February 1, 2016. Email invitations to participate were delivered with a link to the survey, utilizing the online program SurveyMonkey. Nonresponders were contacted up to three times via follow-up emails to encourage participation.
Survey Items
Respondents provided demographic data about themselves and their residency programs. These data included type of program (university-based, community-based, community-based, university-affiliated, or military), years of service as program director, and proportion of international medical graduates. Program directors recorded the percentage of residents who, in their experience, were identified as struggling at some point during their residency training. This definition of forward feeding was provided for standardization: “Forward feeding refers to the sharing of information about learners outside of formal committees.” Respondents indicated whether they felt that faculty should engage in forward feeding and if this practice was routine in their programs. For those who did engage in forward feeding, program directors answered questions regarding how the information was shared, whether any of this information was shared with residents, and if written policies regarding forward-feeding were in place at their institution. Respondents were asked to rate the perceived importance of various types of information about learners (academic performance, clinical performance, professionalism, physical health, and mental health) on a 5-point Likert scale (1=“not at all important” to 5=“extremely important”). They were also asked to rank reasons identified for forward feeding as well as reasons identified for concern with forward feeding. Domains for types of information shared about learners and reasons identified for forward feeding concerns were based on prior literature.6
Analysis
Program director tenure was categorically defined as 3 years or less, 4 to 6 years, or 7 years or more of service. Non-US medical school residents were categorically defined as less than 25%, 25% to 49%, or 50% or more, and percentage of residents identified as struggling was stratified as compared to the mean into categorical variables, either less than or greater than or equal to the mean. Respondent scoring of various types of information potentially shared about learners were categorized into 3 groups: not at all or slightly important, somewhat important, and moderately or extremely important. Because the number of respondents per question varied, the rankings of reasons for forward feeding and concerns regarding forward feeding were compared by average score. Scores for each response were calculated by assigning each response a point value (from one point for topmost important to six points for sixth-most important) and averaged by total number of respondents. All comparisons were run via χ2 analysis. Significance was defined as P<0.05. We performed all data analyses using SAS 9.4 (SAS Institute Inc, Cary, NC).
The overall response rate was 49% (227/461). Community-based, university-affiliated residency programs were the most common (66%, n=149/227). The average program director tenure was 6 years (±5.9 years). Just over half of the programs (54%, n=122/225) reported less than 25% of current residents as graduates of non-US medical schools; 43 programs (19%) reported 25% to 49%; and 60 programs (27%) reported 50% or more of international medical school graduates.
On average, 15% of residents were identified as struggling at some point during their training. Most respondents agreed that faculty should (87%, n=182/210) and do (83%, n=175/210) engage in forward feeding. However, less than half (40%, n=69/173) indicated that forward-fed information was accessible to residents. Programs with higher proportions of international medical school graduates were more likely to make the information available to residents (P=0.03). No other differences were noted based on type of residency program, program director tenure, proportion of non-US medical school graduates, or percentage of residents identified as struggling.
Forward-fed information was most commonly shared through informal conversations (50%, n=88/175). This was followed by formal evaluations (21%, n=36), informal written communication (17%, n=31), and faculty meetings (9%, n=16). Only 14% (n=30/210) of family medicine residency programs had a written policy regarding forward feeding. Of those, four specifically prohibited forward feeding.
Concerns regarding professionalism (88%, n=183/206) and clinical performance (87%, n=180/207) were reported as the most important elements to share. This was followed by academic performance (64%, n=103/207) and mental health (63%, n=130/207). Less than half of respondents (44%, n=90/207) felt that sharing concerns regarding physical health was either moderately or extremely important.
The most important reason identified for forward feeding was the early identification of struggling residents, followed by the ability to direct teaching to the resident’s specific needs, and improving the quality of feedback (Table 1). Fear of creating bias was the most commonly cited concern for engaging in forward feeding, followed by fear of violating confidentiality and difficulty maintaining confidentiality. Fear of litigation was the least common concern (Table 2).
Forward feeding is a method of communicating information about resident behaviors and performance. Despite concerns, the majority of program directors feel that faculty should and do engage in forward feeding. Our findings regarding the rates of struggling learners in GME (10% to 15%) are similar to identified rates in UME.12 However, our findings also suggest that the use of forward feeding occurs more often in GME as compared to UME. The primary reason for forward feeding (early identification of struggling learners) is also similar to UME.9-10 Additional objectives of forward feeding identified in our study include directing teaching to a resident’s specific needs and improving the quality of feedback.
Concerns regarding forward feeding were also noted to be consistent between UME and GME, with fear of creating bias and fear of violating confidentiality listed as two of the primary concerns. Creating bias through the establishment of a Pygmalion effect13,14 could potentially alter learner performance, either negatively or positively, where low expectations may impair performance or high expectations may enhance learner performance. However, it can also give faculty reports regarding specific behaviors of a resident, with any concerns, prior to their working with the resident with the intent to improve tracking of any professionalism issues or deficits in patient care. While fear of litigation was noted as a prominent concern for those involved in UME, it was the least notable concern for educators in GME.9,10 Fear of litigation was a larger influence on opinions of those involved in UME, likely due to the potential to violate the Family Educational Rights and Privacy Act (FERPA). This law prohibits disclosure of any identifiable information from educational records and is often the basis for institutional policies prohibiting practices such as forward feeding. As residents are considered employees of the institutional sponsor, and not students, FERPA loses its relevance in GME.
Difficulty in medical student clerkship progress has been identified particularly in the domains of medical knowledge and professionalism.4,10 Similarly, our study confirms the importance of clinical performance and professionalism as two important themes of information shared by attendings about residents. Performance shortfalls in the domains of patient care and professionalism in both medical school and residency have also been linked to subsequent disciplinary action by state boards, regardless of specialty.15,16 Prior research has identified two types of unprofessional behavior that warrant particular attention: irresponsibility (unreliable attendance, poor follow up on patient care) and diminished capacity for self-improvement (failure to accept contstructive criticism, argumentativeness, and poor attitude).17 Identification of these troubling domains of behavior in UME may also help residency program directors to stratify their concerns toward residents who demonstrate similar behaviors and warrant earlier intervention. Thus, forward feeding may help medical educators meet their responsibility both to the trainee and the public to provide learners with necessary remediation or even termination for those unable to achieve competency.
Concerns regarding professionalism and clinical performance were reported as the most important elements to share, however, only roughly half of respondents felt concerns regarding mental or physical health were important, despite the current focus on resident wellness within GME. Although only 40% of residency programs indicated that information disclosed during forward feeding is accessible to residents, we support a clear and explicit method of sharing specific feedback with the resident. Making the feedback received via forward feeding available to residents is vital for making them central to the process. Furthermore, receiving feedback that is given in a constructive tone is necessary in order to improve residents’ educational experience and increase their potential for success. By developing institutional policies about the types of information shared and with whom the information-sharing should occur, faculty will be more comfortable discussing feedback for the benefit of the resident physician.
Although this survey was distributed to all family medicine residency directors, there is a possibility of nonresponse bias. However, the effect of nonrespondents would have likely been variable and therefore unlikely to affect the study results. This study purposefully offered domains of information shared about learners that were similar to previous studies, so that we could compare and contrast our findings to previously published work. By offering these predefined domains as opposed to free-text responses, we may have missed other important domains examined by residency programs.
Despite concerns raised, the majority of program directors feel that faculty should and do engage in forward feeding. The principal goal of forward feeding is the early identification of struggling residents, followed by the ability to direct teaching to the resident’s specific needs, and improving the quality of feedback. With the ACGME’s 2013 common program requirement for a Clinical Competency Committee (CCC), residency programs are now provided a setting in which information obtained through forward feeding can be discussed, each resident’s progress can be evaluated against objective milestones, and concerns regarding clinical performance or professionalism can be addressed in an open and thoughtful manner, with the goal of producing a skilled clinician.18 Forward feeding provides individual faculty the ability to present independent and contextually varied assessments of learners without the concern of unfairly labeling a learner based on a single behavioral observation. These assessments contribute to a cumulative performance evaluation that enhances resident understanding of progression toward competency and creates an open dialogue for improvement. Future studies are necessary to evaluate the impact of forward feeding, including early intervention and progression toward competencies in the ACGME Milestones.
Acknowledgments
Presentations: Mims L, DeCastro A, Chessman A. Perspectives of Family Medicine Residency Program Directors Regarding Forward Feeding: Results of a CERA Survey. Society for Teachers of Family Medicine Annual Spring Conference. May 2017.
References
- Frank JR, Snell LS, Cate OT, et al. Competency-based medical education: theory to practice. Med Teach. 2010;32(8):638-645. https://doi.org/10.3109/0142159X.2010.501190
- 2. Edgar L, Roberts S, Holmboe E. Milestones 2.0: A Step Forward. JGIM. 2018; 10(3) 367-369. https://doi.org/10.4300/JGME-D-18-00372.1
- Cleary L. “Forward feeding” about students’ progress: the case for longitudinal, progressive, and shared assessment of medical students. Acad Med. 2008;83(9):800. https://doi.org/10.1097/ACM.0b013e318181cfbc
- Cox SM. “Forward feeding” about students’ progress: information on struggling medical students should not be shared among clerkship directors or with students’ current teachers. Acad Med. 2008;83(9):801. https://doi.org/10.1097/ACM.0b013e318181cfe6
- Pangaro L. “Forward feeding” about students’ progress: more information will enable better policy. Acad Med. 2008;83(9):802-803. https://doi.org/10.1097/ACM.0b013e318181d025
- Mims LD, DeCastro AO, Kelly AG. Perspectives of Family Medicine Clerkship Directors Regarding Forward Feeding: A CERA Study. Fam Med. 2017;49(9):699-705.
- Tonesk X, Buchanan RG. An AAMC pilot study by 10 medical schools of clinical evaluation of students. J Med Educ. 1987;62(9):707-718. https://doi.org/10.1097/00001888-198709000-00001
- Cohen GS, Blumberg P. Investigating whether teachers should be given assessments of students made by previous teachers. Acad Med. 1991;66(5):288-289. https://doi.org/10.1097/00001888-199105000-00013
- Gold WL, McArdle P, Federman DD. Should medical school faculty see assessments of students made by previous teachers? Acad Med. 2002;77(11):1096-1100. https://doi.org/10.1097/00001888-200211000-00006
- Frellsen SL, Baker EA, Papp KK, Durning SJ. Medical school policies regarding struggling medical students during the internal medicine clerkships: results of a national survey. Acad Med. 2008;83(9):876-881. https://doi.org/10.1097/ACM.0b013e318181da98
- Seehusen DA, Mainous AG III, Chessman AW. Creating a Centralized Infrastructure to Facilitate Medical Education Research. Ann Fam Med. 2018;16(3):257-260. https://doi.org/10.1370/afm.2228
- Yates J, James D. Predicting the “strugglers”: a case-control study of students at Nottingham University Medical School. BMJ. 2006;332(7548):1009-1013. https://doi.org/10.1136/bmj.38730.678310.63
- Murphy KR, Balzer WK, Lockhart MC, Eisenman EJ. Effects of previous performance on evaluations of present performance. J Appl Psychol. 1985;70(1):72-84. https://doi.org/10.1037/0021-9010.70.1.72
- Nieminen LRG, Rudolph CW, Baltes BB, Casper CM, Wynne KT, Kirby LC. The combined effect of ratee’s bodyweight and past performance information on performance judgements. J Appl Psychol. 2013;43:527-543.
- Papadakis MA, Teherani A, Banach MA, et al. Disciplinary action by medical boards and prior behavior in medical school. N Engl J Med. 2005;353(25):2673-2682. https://doi.org/10.1056/NEJMsa052596
- Papadakis MA, Arnold GK, Blank LL, Holmboe ES, Lipner RS. Performance during internal medicine residency training and subsequent disciplinary action by state licensing boards. Ann Intern Med. 2008;148(11):869-876. https://doi.org/10.7326/0003-4819-148-11-200806030-00009
- Teherani A, Hodgson CS, Banach M, Papadakis MA. Domains of unprofessional behavior during medical school associated with future disciplinary action by a state medical board. Acad Med. 2005;80(10)(suppl):S17-S20. https://doi.org/10.1097/00001888-200510001-00008
- Accreditation Council for Graduate Medical Education. ACGME Common Program Requirements. Published July 1, 2017. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/CPRs_2017-07-01.pdf. Accessed February 4, 2019.




There are no comments for this article.