Background and Objectives: Fewer than 10% of US medical school graduates enter family medicine residencies each year. Little is known about the perceptions and attitudes of senior medical students as they make final decisions about specialty choice, especially those that support a decision to pursue family medicine. The American Academy of Family Physicians (AAFP) administered a national survey to US seniors in 2015 to explore these factors.
Methods: US seniors who were AAFP members (N=11,998) were invited to complete a survey exploring attitudes toward family medicine and experiences that influenced interest and choice of family medicine (FM) or other specialties. This was offered after students submitted their National Residency Matching Program rank list but before match. For those matching in family medicine, additional questions explored mentorship experience. Factors significantly predicting intent to match in family medicine, mentor attributes significantly influencing student attitudes, and family medicine interest group (FMIG) participation were identified via regression.
Results: The survey response rate was 15.1%. Student perceptions of the respect of FM (OR=0.82), the future of FM (OR=2.04), and FMIG involvement (OR=1.75) predicted choosing FM, as did AAFP student membership (OR=2.13-2.44) and AAFP National Conference of Family Medicine Residents and Students attendance (OR=9.77). For students entering FM, having supportive mentors outside of FM and being dedicated to FM positively influenced their attitudes toward FM and their FMIG participation.
Conclusion: National programs, FMIGs, mentorship, and medical school support of family medicine play a role in student selection of family medicine.
The health of people living in the United States depends on a robust primary care workforce with at least 40% of health care in primary care.1 Physicians practicing primary care are a vital part of that workforce. However, only about 14% of US medical students who match through the National Resident Matching Program (NRMP) match to residencies in a primary care field (family medicine, internal medicine-primary care, pediatrics-primary care, or internal medicine-pediatrics) and the contribution of allopathic medical schools to the family medicine workforce, although on an upward trend since 2010, has decreased dramatically since its peak in 1997.2-4 Students graduating US osteopathic medical schools enter primary care fields at a higher rate—with about 15% matching to family medicine residencies alone—but contribute smaller numbers to the workforce.5 Of the medical specialties most likely to produce physicians who practice primary care, family medicine represents the majority of residency training positions, and makes the largest contribution to the primary care physician workforce, both in raw numbers and in percentage of graduates who go on to practice primary care.6 Family medicine’s geographic distribution also more closely matches that of the US population than any other medical specialty.7-9
As a result, many entities dedicate resources toward increasing the number of US medical students who enter family medicine residency training programs to grow the US primary care workforce. Among those entities are the American Academy of Family Physicians (AAFP), the 55 constituent state and local chapters of the AAFP, and departments of family medicine at US medical schools. Eight national family medicine organizations have committed to working together toward an aim of 25% of graduating US medical students, allopathic and osteopathic, entering family medicine by the year 2030.8 The AAFP offers free membership to medical students, supports family medicine interest groups (FMIGs) at medical schools through an extensive set of interventions and resources, and hosts an annual conference for medical students and family medicine residents.
The impact of these efforts is unclear. Students’ initial interest or plan to practice in rural areas, to serve underserved populations, or to practice primary care are associated with primary care specialty choice.10 Studies of the impact of FMIGs on students entering family medicine are mixed.11,12 School culture and climate regarding primary care, and faculty mentorship can also influence student specialty choice.13-15
To better describe the potential impact of the hidden curriculum of medical school on medical student specialty choice, the AAFP designed and administered a survey that was distributed to AAFP medical student members graduating in 2015.16,17 Although student members of AAFP are more likely to be interested in family medicine, the majority ultimately choose other specialties. The goals of the survey were to capture from a sample of students entering a variety of specialities: (1) student impressions of respect for family medicine and support for family medicine career goals at their institutions, (2) the impact of those perceptions on specialty choice, and (3) the impact of mentors and role models, FMIG involvement, and the AAFP’s programs on student specialty choice. Finally, for those graduating students who reported an intention to enter family medicine, this study explored the relationship between faculty mentorship and personal career interest with intention to enter family medicine, attitudes toward family medicine, and FMIG involvement.
Participants and Sampling
Participants were eligible to complete the survey if they were a medical student member of the AAFP whose member record reported that they were graduating in 2015. Graduation dates are supplied by student members when they join the AAFP. In February 2015, the AAFP sent all 11,998 eligible fourth-year medical student members a survey constructed specifically for the purpose of this study, via mail (paper copy) and email (with a web link to respond). A follow-up mailing and email message were sent to nonresponders in March, 2015. As an incentive to participate, respondents were entered into a drawing for one of ten $100 American Express gift cards. The timing of the survey was intended to solicit responses after students had submitted their NRMP rank lists, but before they received their residency match. Novi Survey was used for electronic survey administration. The AAFP Institutional Review Board approved this study.
Instrument Construction and Piloting
In response to a call from AAFP membership in 2015 to learn more about how the hidden curriculum may be affecting student specialty choice, AAFP staff developed a purposive survey instrument. The survey did not undergo a full validation process, due to time and resource constraints. However, face validity was assessed by the AAFP Commission on Education, with members including medical school and residency faculty, residents, students, and AAFP Medical Education staff. Question construction was informed by AAFP marketing staff with survey design experience.
Instrument
The 16-question instrument (Table 1) assessed student attitudes toward family medicine and the self-reported impact of AAFP programs (AAFP membership, FMIG participation, attendance at the AAFP National Conference of Family Medicine Residents and Medical Students) on interest in family medicine and choice of specialty. Students who reported the intention to enter family medicine were asked an additional 5-part question about faculty support and mentorship.
Three questions explored attitudes regarding the importance of family medicine (not at all important, not very important, somewhat important, very important), the future of family medicine (very negative, somewhat negative, somewhat positive, very positive), and to what degree students perceived family medicine as respected at their school (strongly disagree, disagree, neutral, agree, strongly agree). One question asked about level of FMIG involvement (not at all involved, not very involved, somewhat involved, very involved).
Eight questions asked about the influence of the experiences of AAFP membership, FMIG involvement, and the AAFP National Conference of Family Medicine Residents and Medical Students on family medicine interest or specialty choice, with a dichotomous yes/no response choice.
Students who reported intention to match in family medicine were asked about their agreement (strongly disagree, disagree, neutral, agree, strongly agree) with five statements about mentorship and its impact on their specialty choice:
- My family medicine mentors and faculty were very supportive of my interest in family medicine.
- My non-family medicine mentors and faculty were very supportive of my interest in family medicine.
- I was swayed toward family medicine by strong family medicine/primary care mentors.
- I had strong family medicine/primary care mentors, but I was pretty sure I was going into family medicine anyway.
- I didn’t have any strong family medicine/primary care mentors.
The four Likert-style questions assessing student attitudes toward family medicine were standardized using z scores to be able to potentially calculate predicted probabilities from the logistic regression model. The dichotomous responses to the eight questions about the influence of experiences on family medicine interest or specialty choice were dummy coded (0=no, 1=yes). Questions about mentor experience for students who reported choosing family medicine were coded 1=strongly disagree, 2=agree, 3=neutral, 4=agree, 5=strongly agree. Reported specialty choice was dichotomized to include family medicine (1) vs any other (0).
Statistical Procedures
Using the entire available sample (N=1,530), we modeled the effects of attitudes about family medicine and the experiences reported by respondents on the outcome of student-reported plans to enter family medicine compared to students entering another specialty. To estimate the relative effects of reported attitudes and experiences, we used binary logistic regression to calculate the odds ratio (OR) for each predictor on the outcome of family medicine choice (yes/no). Standard predictor entry was used to calculate ORs and 95% confidence intervals. Predictors included the four standardized items on family medicine attitudes, the four dichotomous items on the influence of experiences on interest in family medicine, and the four dichotomous items on the influence of experiences on choosing family medicine as a specialty.
Using a subset of data for students who reported plans to enter family medicine (N=600), descriptive statistics were calculated for the five items assessing experience with faculty and mentors. To calculate the relative effect sizes of each predictor on outcomes, we employed ordinary least squares linear regression with standard predictor entry in order to identify predictors among the five faculty and mentor questions for four outcomes: (1) student perception of the future of family medicine, (2) student beliefs about importance of family medicine to the US health care system, (3) self-reported student involvement in FMIG, and (4) student perception of respect for family medicine at their school.
All analyses used an a set at <0.05 and were conducted in SPSS software, version 19.
Of the 11,998 students invited, 1,814 completed the survey (response rate 15.1%); 1,530 respondents (84.3%) reported the specialty they ranked in the match and are included in this analysis. Response rates for individual questions are listed in Table 1 and ranged between 97.2% and 100%. Six hundred students (39.2%) reported plans to enter family medicine; the remaining 930 students reported plans to enter another specialty.
The entire sample rated the future of family medicine, respect of family medicine at their school, and the importance of family medicine to the US health care systems positively (Table 1). They rated their FMIG involvement at 2.07 on the 4-point scale. The proportion of students reporting that AAFP student membership, AAFP National Conference of Family Medicine Residents and Medical Students, or FMIG involvement influenced their interest in the specialty was 33%, 15%, and 23% respectively. When asked about their final specialty choice, a smaller proportion of students reported AAFP membership (7%), National Conference attendance (6%) and FMIG involvement (8%) had an influence. More than one-quarter (26%) of students said none of these experiences influenced their interest in family medicine. In summary, while 71% reported that these experiences influenced their interest in family medicine, most (84%) reported that none of these experiences influenced their final specialty choice.
The 600 students with plans to enter family medicine reported having supportive family medicine mentors (mean 4.75 on 5-point scale) and being swayed to choose family medicine by these mentors (mean 4.12), as described in Table 1. They agreed to a lesser degree that non-family medicine mentors were supportive (mean 3.63), and 92% disagreed with the statement, “I did not have family medicine/primary care mentors” (mean 1.77).
A complete dataset for the logistic regression was available from 1,500 respondents (589 intending to match in family medicine and 911 not intending to match in family medicine; Table 2). The regression model with 12 predictors accounted for 50.7% of the variance of the sample. Eight predictors significantly and uniquely contributed to determining whether a student reported choosing family medicine versus another specialty (Table 3). Students who reported the perception that family medicine was more respected at their school had lower odds of entering family medicine (OR=.82). Viewing the future of family medicine positively was associated with higher odds of choosing the field (OR=2.04). Perceptions of the importance of family medicine to the US health care system were not predictive of entering the specialty. Involvement in FMIG (OR=1.75) and reporting that it influenced specialty choice (OR=2.35) was associated with intention to match in family medicine (OR=2.35), while reporting that FMIG influenced interest in the field was not. AAFP student membership influenced interest (OR=2.13) and choice of family medicine (OR=2.44) were each predictive of intention to match in family medicine. Students reporting the AAFP National Conference influenced their interest had an OR of 9.77 for intention to match in family medicine. Most surprising, students who reported that none of these experiences influenced their interest had an OR of 13.52 for entering family medicine. However, reporting that none of these experiences impacted their specialty choice was not predictive of intention to enter family medicine.
Mentorship experiences did not predict student attitudes regarding the importance of family medicine to the US health care system in the linear regression model (data not shown, ANOVA for model F=1.87 with df=5, P=0.09, adjusted R2=0.08.) Having non-family physician mentors supportive of family medicine, reporting strong family medicine and primary care mentors for students already intending to choose family medicine, and reporting no lack of primary care/family medicine mentors, were each significantly predictive of agreement that family medicine was respected at their school (Table 3).
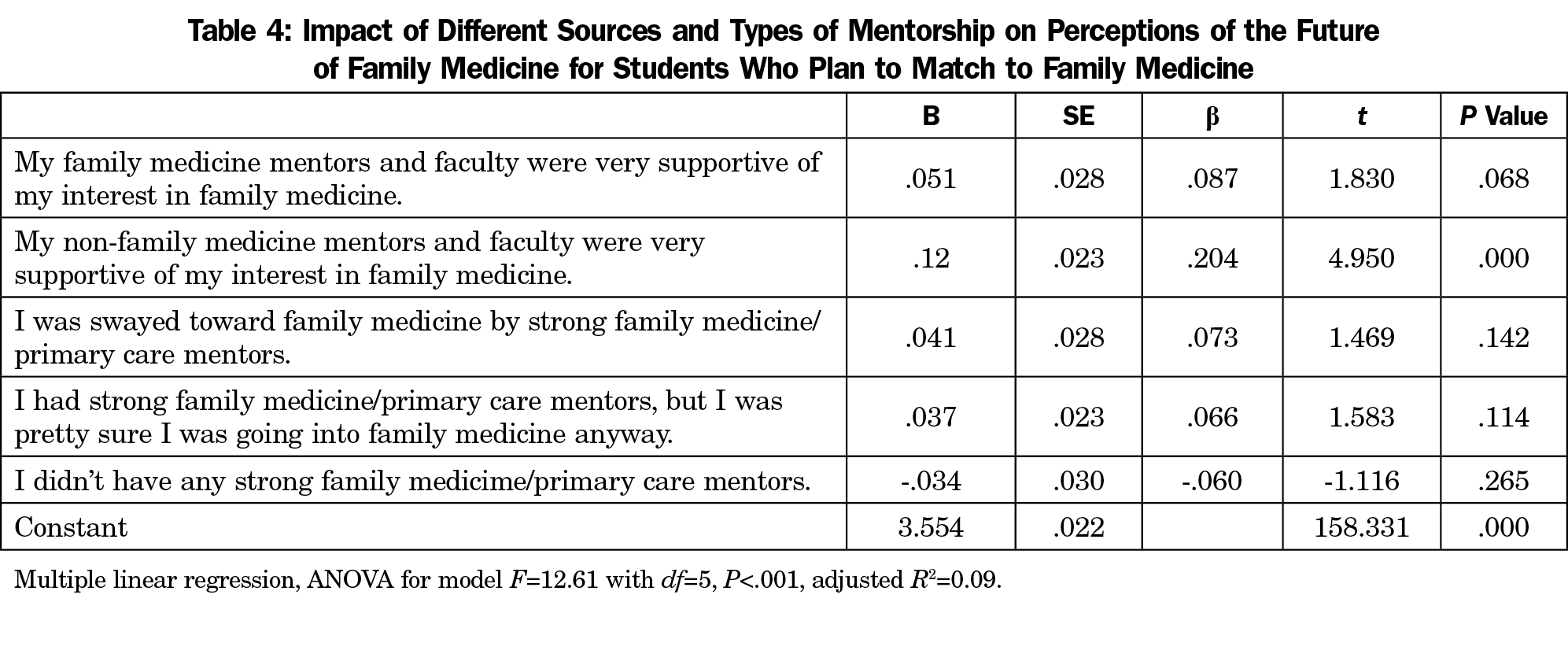
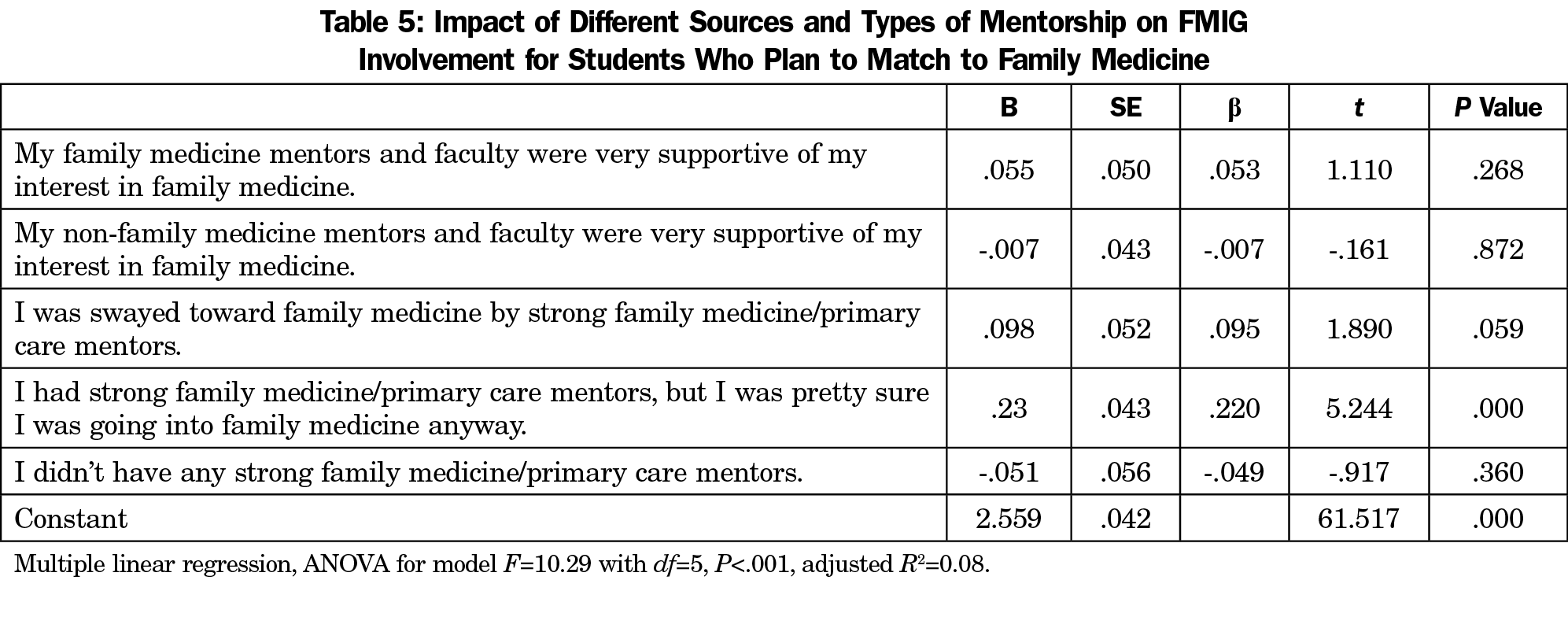
After controlling for family medicine mentorship, student experience with mentors and faculty other than family physicians who were very supportive of their interest in family medicine was the only predictor associated with positive views of the future of family medicine (Table 4). Likewise, after controlling for all mentorship experiences, the only predictor associated with FMIG involvement was being interested in the field in the first place (Table 5).
Medical student specialty choice is a dynamic decision influenced by decades of life experiences before medical school and many elements during medical school.14,18 The results of this study are consistent with previous research indicating that student interest in family medicine upon entry to medical school is strongly predictive of eventual family medicine specialty choice. This study adds to previous literature by quantitatively evaluating the impact of medical student experiences during medical school, particularly family medicine-focused extracurricular activities, which are intended to support and build student interest in family medicine. This study also examined the influence of mentorship, perceptions of respect and support for family medicine from the larger institution and those outside of family medicine, and vision for the future of the specialty. It identified that factors influencing choice of family medicine as a career are different from those that influence interest in the specialty.
These data indicate that having faculty and mentors who are supportive of family medicine significantly influences students to choose family medicine. Further, the data suggest that the support of family medicine mentors is practically necessary for family medicine specialty choice, and also insufficient for many. More than 90% of students who reported family medicine as their first specialty choice also reported that they were supported by strong mentors in family medicine. Importantly, students who chose family medicine were also more likely to report that faculty and mentors outside of family medicine were supportive of family medicine, suggesting that the perceived support for family medicine of the greater medical community has a strong influence on students. Previous research also suggests mentorship may be more important for students intending to match into family medicine than intending to match in other specialties.19-23
The support of non-family medicine mentors was particularly important for cultivating a culture of support for family medicine and for endorsing a positive future for the specialty. A student’s belief that the future of family medicine is positive is predictive of a choice of family medicine, while student perception about the importance of primary care was not. These data reflect the importance of support for family medicine from outside of the family medicine department, in order for students to view family medicine as a specialty with a promising future, and ultimately to support student intent to match in family medicine.
These results also suggest that students who choose family medicine are more likely to disagree that family medicine is a respected specialty at their medical schools. The authors believe that students who have chosen family medicine may become more sensitive to actions and situations that can be perceived as disrespectful of family medicine. Though this study did not account for this variable, it is also possible that students who choose family medicine and are open or outspoken about that choice may actually experience more microaggressions related to that choice than a student choosing another specialty or who has not openly declared their specialty preference.
Initial interest in family medicine may drive students toward involvement in a family medicine interest group, AAFP membership, and participation in the AAFP National Conference of Family Medicine Residents and Students. The education and peer support these groups provide is particularly influential for some students. The students who reported higher levels of FMIG involvement were more likely to have chosen family medicine, validating their assessments that FMIG involvement was in some way related to their interest in and choice of the specialty. Although a relatively small number of students reported that participation in AAFP-sponsored activities influenced their specialty choice, these data suggest that those experiences do contribute to student intention to enter family medicine at least for some. FMIG involvement was also associated with family medicine mentorship. Taken together, the results suggest that AAFP student support is important for maintaining and increasing student choice of family medicine but should not be the only strategy employed to do so. One possible explanation for the disparity between impact of AAFP-sponsored activities on interest in specialty and ultimate specialty choice is that some students may already be maximally interested in family medicine, so that while these experiences had a limited impact on student perceptions regarding their own interest, they were associated with supporting student specialty choice.
Strengths of this study include the use of a national sample and that respondents completed a large portion of the survey. Graduation dates were determined by student selection at the time they signed up for the AAFP, thus it is possible some students received this survey and were not in their final year of medical school if they decelerated, took a leave, or experienced another event that changed their initially reported graduation date.
This study is limited by the low overall response rate of 15.1%, however the 600 students with plans to enter family medicine represent 39.2% of survey respondents and 35.9% of the 1,669 US seniors applying to family medicine residency programs in 2015, which are comparable proportions.24 Analyses of this population of respondents (Tables 3-5), is more likely to be representative of all students intending to match into family medicine and is less influenced by the lower overall response rate. The 930 respondents applying to other specialties represent a much smaller percentage of all US seniors applying to other specialties. Because the study is a sample of AAFP student members, it should not be considered representative of all fourth-year medical students; sampled students are likely more interested in family medicine and more likely to be from allopathic medical schools. Because of these factors, results shown in the first part of Table 1 may skew toward a more favorable view of family medicine than held by all US seniors. Because of the anonymous nature of the survey, no demographic or institutional data were collected for the regression models. We can therefore only speculate on differences between respondents and nonrespondents. If respondents not intending to match into family medicine hold more favorable views than US seniors in general, it is possible that some of the nonsignificant factors in Table 2 are actually significant. Conversely, if respondents not intending to match into family medicine hold less favorable views than US seniors in general, some of the factors identified as significant in Table 2 may not actually be significant. Finally, the regression model only accounted for about 50% of the variance, limiting the value of any single factor or combination of factors. Clearly, specialty choice is complex. This study focused on AAFP activities and medical school experiences; but students are also influenced in important ways by experiences and values before medical school, by the larger health care environment, and by financial incentives.14, 25-28
In summary, this study confirms prior research findings that students entering family medicine often come to medical school with interest in and passion for the specialty. Supporting that passion through family medicine mentors and targeted experiences like FMIGs and AAFP membership and conferences is key. Yet mentors and faculty from outside of family medicine who are supportive of student interest in family medicine are especially valuable in supporting positive attitudes toward the field and student intent to match in family medicine. This suggests that generating institutional support for family medicine from mentors outside of family medicine could increase numbers of students intending to match into family medicine. It is important for students to not only learn about the importance of family medicine to the health care system, but also to see a positive future for the specialty, and be supported by their faculty and institution to picture themselves in that future.
Acknowledgments
This study was previously presented as follows:
- Kelly C, Bentley A, Phillips JP, Prunuske J, Kost A, Morley CP. Family medicine interest groups: what we know and what we want to know. Seminar at Society of Teachers of Family Medicine Medical Student Education Meeting; February, 2017; Anaheim, CA.
- Kelly CM, Bentley AE, Kost A, Morley CP, Phillips JP, Prunuske J. Student choice of family medicine – what influence do FMIGs have? Lecture-discussion at Society of Teachers of Family Medicine Annual Spring Conference; May, 2017; San Diego, CA.
- Kelly CM, Bentley AE, Kost A, Morley CP, Phillips JP, Prunuske J, Travis A. Student choice of family medicine: what impact do FMIGs have? Poster on research in progress at North American Primary Care Research Group Annual Conference, November, 2017; Montreal, QC, Canada.
- Morley CP, Kost A, Bentley AE, Kelly CM, Phillips JP, Prunuske J, Travis A. Analysis of 2015 AAFP student member survey data: principal components analysis of family medicine matchers. In-progress research project presented at Society of Teachers of Family Medicine Conference on Medical Student Education; February, 2018; Austin, TX.
References
- US Department of Health and Human Services, Health Resources and Services Administration. Advancing Primary Care: Council on Graduate Medical Education 20th Report. 2010.
- Iglehart JK. Health reform, primary care, and graduate medical education. N Engl J Med. 2010;363(6):584-590. https://doi.org/10.1056/NEJMhpr1006115
- American Academy of Family Physicians. 2018 Match Results for Family Medicine. https://www.aafp.org/medical-school-residency/program-directors/nrmp.html. Accessed November 19, 2018.
- Eberhardt MS, Ingram DD, Makuc DM, Pamuk ER. Health, United States, 2001: Urban and Rural Health Chartbook. Hyattsville, MD: National Center for Health Statistics; 2001.
- Lin S, Klink K, Wingrove P, Petterson S. A Dramatic Decrease of Graduates from US Allopathic Schools in the Family Medicine Workforce Since 2000. 2015. https://www.graham-center.org/content/dam/rgc/documents/publications-reports/presentations/DramaticeDecreaseofAllopathicSchools.pdf. Accessed March 25, 2018.
- Kozakowski SM, Travis A, Marcinek JP, Bentley A, Fetter GT Jr. Entry of Medical School Graduates Into Family Medicine Residencies: 2016-2017. Fam Med. 2017;49(9):686-692.
- Petterson SM, Phillips RL, Bazemore AW, Koinis GT. Unequal distribution of the US primary care workforce. Am Fam Physician. 2013;87(11):online. https://www.aafp.org/afp/2013/0601/od1.html. Accessed March 25, 2018.
- Kelly C, FMA Health Workforce Education and Development Team. A shared aim for student choice of family medicine: an update from ADFM and family medicine for america’s health. Ann Fam Med. 2018;16(1):90-91. https://doi.org/10.1370/afm.2191
- Agency for Healthcare Research and Quality. The Distribution of the US Primary Care Workforce. https://www.ahrq.gov/research/findings/factsheets/primary/pcwork3/index.html. Accessed June 26, 2018.
- Jeffe DB, Whelan AJ, Andriole DA. Primary care specialty choices of United States medical graduates, 1997-2006. Acad Med. 2010;85(6):947-958. https://doi.org/10.1097/ACM.0b013e3181dbe77d
- Kost A, Cawse-Lucas J, Evans DV, Overstreet F, Andrilla CHA, Dobie S. Medical student participation in family medicine department extracurricular experiences and choosing to become a family physician. Fam Med. 2015;47(10):763-769.
- Wei McIntosh E, Morley CP. Family medicine or primary care residency selection: effects of family medicine interest groups, MD/ MPH dual degrees, and rural medical education. Fam Med. 2016;48(5):385-388.
- Erikson CE, Danish S, Jones KC, Sandberg SF, Carle AC. The role of medical school culture in primary care career choice. Acad Med. 2013;88(12):1919-1926. https://doi.org/10.1097/ACM.0000000000000038. doi.
- Bennett KL, Phillips JP. Finding, recruiting, and sustaining the future primary care physician workforce: a new theoretical model of specialty choice process. Acad Med. 2010;85(10)(suppl):S81-S88. https://doi.org/10.1097/ACM.0b013e3181ed4bae
- Wendling AL, Wudyka AE, Phillips JP, et al. RU4PC? Texting to quantify feedback about primary care and its relationship with student career interest. Fam Med. 2016;48(1):21-29.
- Lawrence C, Mhlaba T, Stewart KA, Moletsane R, Gaede B, Moshabela M. The hidden curricula of medical education: a scoping review. Acad Med. 2018;93(4):648-656. https://doi.org/10.1097/ACM.0000000000002004
- Inui TS. A Flag in the Wind: Educating for Professionalism in Medicine. 2003. https://members.aamc.org/eweb/upload/AFlagintheWindReport.pdf. Accessed June 26, 2018.
- Kost A, Benedict J, Andrilla CH, Osborn J, Dobie SA. Primary care residency choice and participation in an extracurricular longitudinal medical school program to promote practice with medically underserved populations. Acad Med. 2014;89(1):162-168.
- Kutob RM, Senf JH, Campos-Outcalt D. The diverse functions of role models across primary care specialties. Fam Med. 2006;38(4):244-251.
- Kuzel AJ, Moore SS. Choosing a specialty during a generalist initiative: a focus group study. Fam Med. 1999;31(9):641-646.
- Burack JH, Irby DM, Carline JD, Ambrozy DM, Ellsbury KESF, Stritter FT. A study of medical students’ specialty-choice pathways: trying on possible selves. Acad Med. 1997;72(6):534-541. https://doi.org/10.1097/00001888-199706000-00021
- Henderson E, Berlin A, Fuller J. Attitude of medical students towards general practice and general practitioners. Br J Gen Pract. 2002;52(478):359-363.
- Wright S, Wong A, Newill C. The impact of role models on medical students. J Gen Intern Med. 1997;12(1):53-56. https://doi.org/10.1007/s11606-006-0007-1
- National Resident Matching Program. 2015 NRMP Main Match Data. http://www.nrmp.org/wp-content/uploads/2015/05/Main-Match-Results-and-Data-2015_final.pdf. Accessed September 1, 2018.
- Phillips R, Dodoo M, Petterson S, et al. Specialty and Geographic Distribution of the Physician Workforce: What Influences Medical Student and Resident Choices? Robert Graham Center. 2009. https://www.graham-center.org/dam/rgc/documents/publications-reports/monographs-books/Specialty-geography-compressed.pdf. Accessed August 28, 2018.
- Phillips JP, Petterson SM, Bazemore AW, Phillips RL. A retrospective analysis of the relationship between medical student debt and primary care practice in the United States. Ann Fam Med. 2014;12(6):542-549. https://doi.org/10.1370/afm.1697
- Phillips JP, Wilbanks DM, Salinas DF, Doberneck DM. Educational Debt in the Context of Career Planning: A Qualitative Exploration of Medical Student Perceptions. Teach Learn Med. 2016;28(3):243-251. https://doi.org/10.1080/10401334.2016.1178116
- Phillips J, Weismantel D, Gold K, Schwenk T. How do medical students view the work life of primary care and specialty physicians? Fam Med. 2012;44(1):7-13.






There are no comments for this article.