Background and Objectives: The population surrounding an urban federally qualified health center (FQHC) in Philadelphia has poorer health than Philadelphia overall. Community residents identified aerobics and dance classes as very important services or programs that an FQHC might provide. We sought to measure the impact of participation in a resident physician-led, patient-centered fitness and nutrition class on participants’ attitudes, knowledge, and self-efficacy regarding their health.
Methods: An urban line dancing class and brief healthy eating intervention for adults was held at a YMCA adjacent to a residency-affiliated FQHC weekly for 8 weeks. Pre/postsurveys were administered to assess attitudes and confidence toward physical activity and healthy lifestyles.
Results: Participants’ self-assessment of health and levels of physical activity improved. Confidence in performing everyday activities, doing regular exercise and exercising without making symptoms worse increased. A significant decrease in participants’ physical activity gratification was observed. Participants’ confidence improved in reading food labels for health, but confidence in eating a balanced diet did not improve.
Conclusions: A resident-led fitness and nutrition class, tailored to perceived community needs, generated significant interest and sustained participation. This pilot study furthered development of community infrastructure addressing health, nutrition, and overall fitness, and the results reflect opportunities and challenges of engaging communities in physical fitness.
Racial and ethnic disparities in health persist in the United States.1-3 These disparities also exist in self-perception of health.4 African Americans (AA) were less likely to describe themselves as overweight versus whites,5 were particularly less likely to adopt healthy weight-related attitudes and behaviors, and have worse obesity outcomes.4
Health-specific self-efficacy is a strong predictor of health behaviors.6,7 Recent research has shown efficacy for targeted, community-based interventions resulting in reduced weight and cardiovascular risk factors for AA women in urban communities.8,9 Tailoring a weight-loss intervention to specific populations may be a reasonable approach to reducing chronic disease in these groups.10
The Stephen Klein Wellness Center is a family medicine residency-affiliated federally qualified health center (FQHC) in North Philadelphia serving a predominantly AA community. The FQHC’s target population was determined to have significantly poorer health than Philadelphia residents overall.11
Sociocultural factors play an important, positive role in exercise adherence12; therefore, a community needs survey was performed and identified nutrition, exercise, and physical activity (PA) as very important aspects of health and wellness to community members. Respondents desired aerobic activities, specifically indicating “urban” or “soul” (synchronized, choreographed, social dance with cultural roots in Africa and the Caribbean) line dancing classes,13,14 confirmed by additional community meetings.
This study evaluated how participation in a community-tailored, soul line dancing class with nutrition education correlates with changes in self-assessment of health, levels of PA, attitudes towards PA, and confidence to implement health promoting behavior. Additionally, we aimed to understand adherence to this type of activity.
Setting and Sampling
Participants were recruited by FQHC staff. Flyers were posted throughout the FQHC and an adjacent YMCA. Those under 18 years old and who self-identified as physically unable to participate were excluded. Individuals were consented by resident physicians to participate and signed a waiver of liability. Participants who attended two or more classes were included.
Intervention
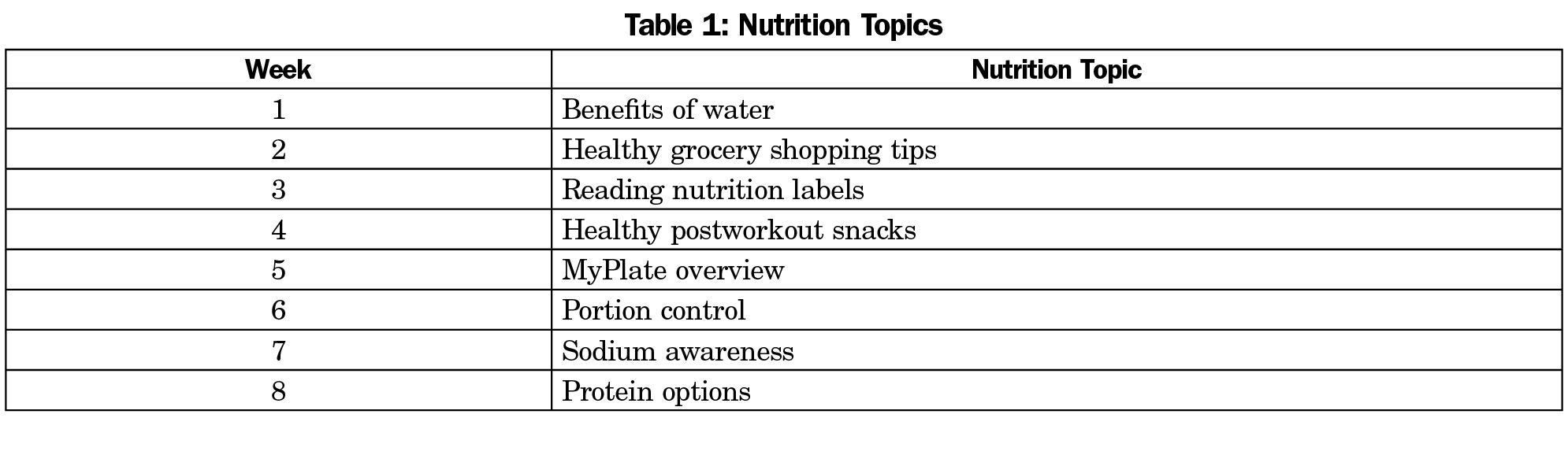
A free, weekly, 50-minute line dancing class was offered for 8 weeks with a 10-minute nutrition lesson at the end of class. A hired instructor from a North Philadelphia YMCA directed the class and physician residents observed their engagement in the class, administered surveys, and taught the nutritional component of the class. Residents were free to dance alongside participants, and often did, as a way to encourage relationship-building. The nutritional education was derived from the Academy of Nutrition and Dietetics (Table 1).15
Our budget was able to support the dance instructor and supplement the nutrition counseling sessions with food items/water. Our nutrition content was online, free, and resident delivered. The cost per participant was estimated at $10.
Measures
Participants completed a preintervention survey at the first class they attended. Postsurveys were administered at the final class; participants who did not attend the final class completed the final survey over the phone.
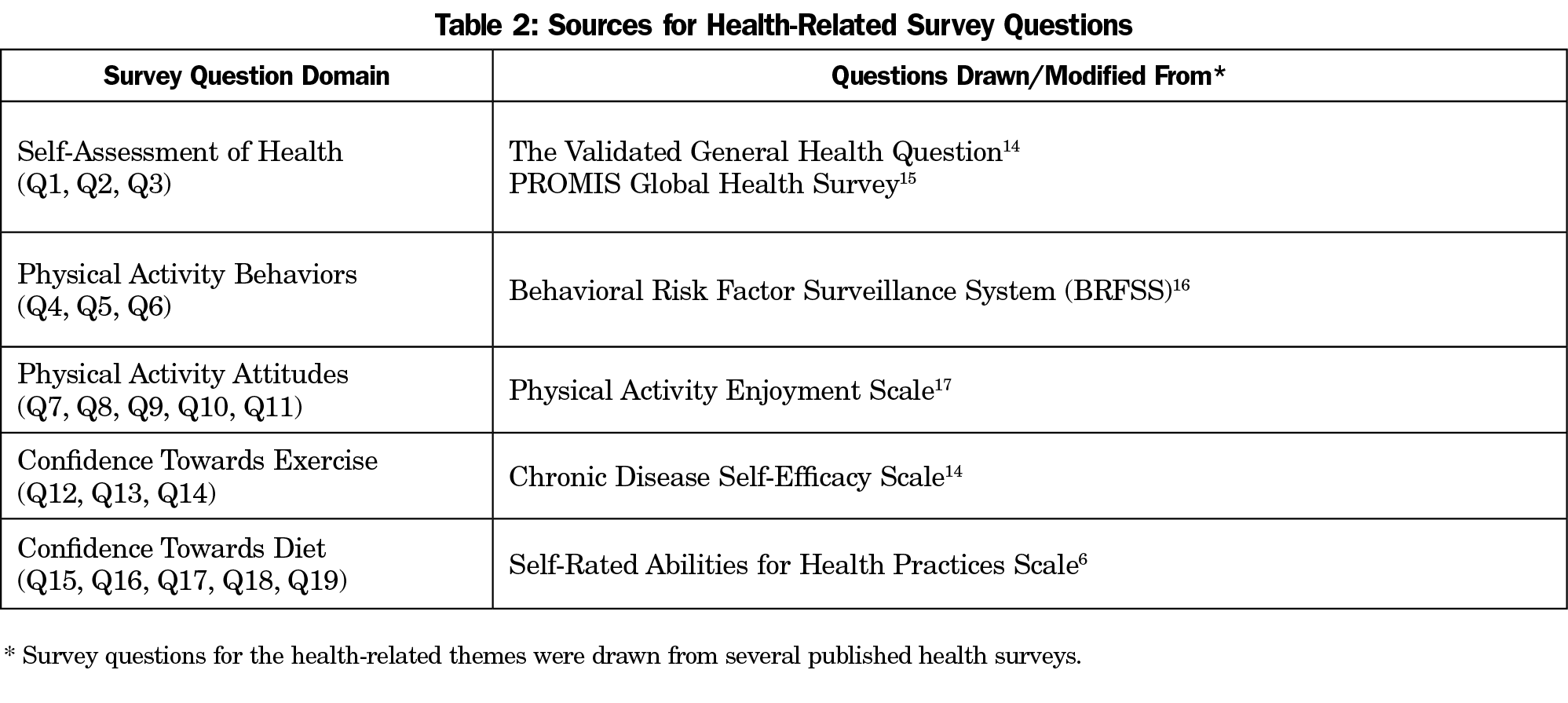
The 31-item survey collected data about participant demographics, self-assessments of health, levels of PA, attitudes toward PA, confidence to implement health promoting behavior, and several program evaluation items (Table 2).
The Institutional Review Board of Thomas Jefferson University approved this study.
Analysis
A descriptive analysis was conducted for participant demographics. For each survey section, paired samples t-tests were used to compare the means of continuous measurements pre- and postsurvey.
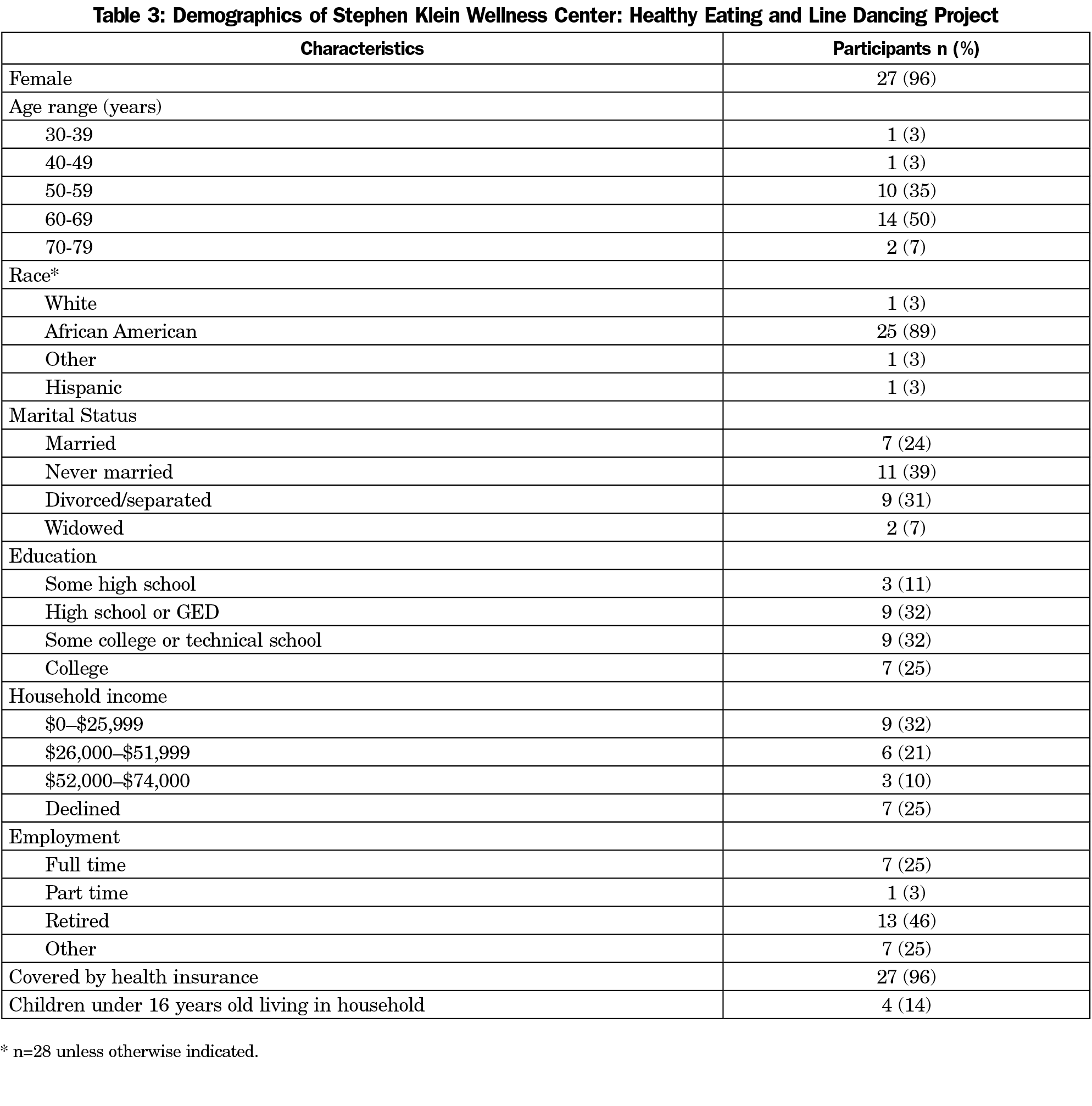
Forty-seven individuals attended at least one class. Sixty percent of participants attended six or more classes. Twenty-eight completed both pre- and postsurveys. A complete descriptive analysis is shown in Table 3.
The mean number of classes attended was 4.92 (SD=2.25). Only three participants had attended the adjacent FQHC’s nutrition class. All respondents “would recommend the class to a friend,” and all were “totally satisfied” with the class. Twenty-one wanted to learn more about nutrition. Participants’ favorite nutrition topics were healthy postworkout snacks, the benefits of water, and healthy shopping tips.
Only two participants had a primary care doctor at the FQHC prior to the class; by the end of the intervention, three additional participants had established care. Sixty percent of participants had a YMCA membership preintervention, and two joined during the study.
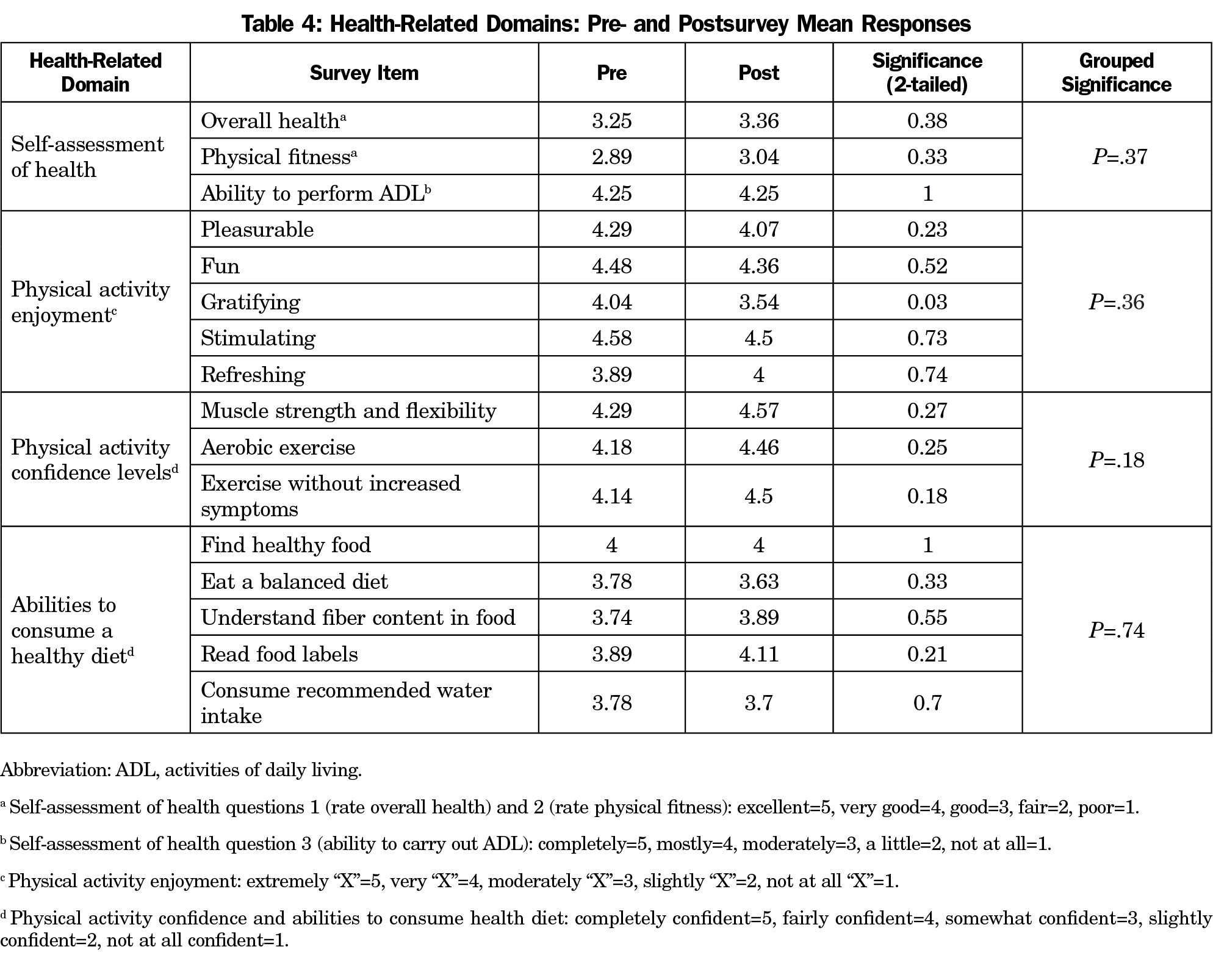
There were no significant changes in self-assessment of one’s overall health, physical fitness, ability to carry out physical activities or PA levels. A significant decrease in PA gratification from pre- to postsurvey was observed. There were no significant differences across the remaining domain questions for PA enjoyment, PA confidence levels, nor the ability to consume a healthy diet (Table 4).
A resident physician-led pilot fitness and nutrition class generated significant interest and sustained participation. Our homogeneous population consisted predominantly of AA women (96%). It has been shown in the literature that social support is a motivating factor for AA women regarding participation in group physical interventions.13 The social cohesion of our population could have contributed to the high adherence observed.
Gratification decreased significantly; this may reflect participants’ challenges with their experience of increased activity. Participation did not decrease throughout the study. Satisfaction was reported with music and the class instructor, which has been shown to correlate with exercise adherence.16 Sociocultural factors play an important role in exercise adherence,12,17 and could be why it remained strong. Our study suggests that using a culturally relevant, social model for PA may be effective at encouraging adherence.
Participants’ overall self-assessment of health and level of physical fitness trended positively. Global health self-assessments are strongly linked to mortality and other health outcomes,17 and longitudinal studies could demonstrate if a relationship exists between self-assessment of health and participation in exercise.
Nonsignificant gains were also noted in confidence towards PA. Increased confidence improves an individual’s likelihood to maintain PA, which is associated with improved quality of life and health outcomes.18,19
Inconsistent changes were noted in confidence to consume a healthy diet. Although our study addressed nutritional education, it did not address disparities that play a role in access to healthy foods and supermarkets, racial and ethnic disparities in food deserts, socioeconomic status and placement of chain grocery stores.20 These should be considered in future attempts to improve confidence in healthy eating.
The intervention’s short length and small sample size limited our findings. Our project was conducted in a single neighborhood with largely older, female, AA participants limiting generalizability. A larger, more diverse sample over a greater duration as well as determining motivational factors for participant sign up and attrition may be worth exploring. Additionally, combining questions from multiple instruments limited the validity and reliability of measurement and the ability to compare findings to other studies. Of note, the statistically significant finding of decreased gratification does not necessarily equate to meaningful clinical change in behaviors or motives for exercise participation. A qualitative approach would be an appropriate next step to determine if a decrease in gratification of physical activity was clinically meaningful and why it occurred; this approach could also uncover barriers to participation in the class. Finally, relationship development with participants and the impact of the study on resident attitudes and behaviors with underserved populations are also two important factors that could be addressed in future studies.
This project identified a community partnership with potential to improve the community’s ability to address health, nutrition, and overall fitness. The class increased YMCA memberships and the number of patients receiving primary care at the FQHC. We encourage this FQHC and YMCA partnership to be modeled by others to foster active engagement in health and well-being.
Acknowledgments
The authors thank the Women’s Board of Thomas Jefferson University for financial support of this pilot intervention, as well as the faculty and staff at the YMCA, TJUH and SKWC for support of the project, assistance with recruitment, and guidance with analysis.
This study was presented as “Development of a Community-Tailored, Resident-Led, Fitness and Healthy Eating Intervention at an Urban Federally Qualified Health Center,” at the 2017 Society of Teachers of Family Medicine Annual Spring Conference, May 5-6, 2017, San Diego, CA.
References
- Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111(10):1233-1241. https://doi.org/10.1161/01.CIR.0000158136.76824.04
- Keppel KG. Ten largest racial and ethnic health disparities in the United States based on Healthy People 2010 Objectives. Am J Epidemiol. 2007;166(1):97-103. https://doi.org/10.1093/aje/kwm044
- National Center for Health Statistics. Health, United States, 2015: with special feature on racial and ethnic health disparities. 2016:2016-1232.
- Duncan DT, Wolin KY, Scharoun-Lee M, Ding EL, Warner ET, Bennett GG. Does perception equal reality? Weight misperception in relation to weight-related attitudes and behaviors among overweight and obese US adults. Int J Behav Nutr Phys Act. 2011;8.1:20. https://doi.org/10.1186/1479-5868-8-20
- Langellier BA, Glik D, Ortega AN, Prelip ML. Trends in racial/ethnic disparities in overweight self-perception among US adults, 1988-1994 and 1999-2008. Public Health Nutr. 2015;18(12):2115-2125. https://doi.org/10.1017/S1368980014002560
- Becker H, Stuifbergen A, Oh HS, Hall S. Self-rated abilities for health practices: A health self-efficacy measure. Health Values: The Journal of Health Behavior. Education & Promotion. 1993;17(5):42-50.
- Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff (Millwood). 2013;32(2):207-214. https://doi.org/10.1377/hlthaff.2012.1061
- Rodriguez F, Christopher L, Johnson CE, Wang Y, Foody JM. Love your heart: a pilot community-based intervention to improve the cardiovascular health of African American women. Ethn Dis. 2012;22(4):416-421. PMID:23140071
- Murrock CJ, Gary FA. Culturally specific dance to reduce obesity in African American women. Health Promot Pract. 2010;11(4):465-473. https://doi.org/10.1177/1524839908323520
- Shiriki K, Whitt-Glover MC, Gary TL, Prewitt ET, Odoms-Young AM, Banks-Wallace J, Beech BM, Hughes-Halbert C, Karanja N, Lancaster KJ, Samuel-Hodge CD. Expanding the Obesity Research Paradigm to Reach African American Communities. Prev Chronic Dis 2007;4.4: A112.
- Philadelphia Health Management Corporation. An Assessment of the Need for a Wellness Center in North Philadelphia, Zip Codes 19121 and 19132. December, 2006.
- Trost SG, Owen N, Bauman AE, Sallis JF, Brown W. Correlates of adults’ participation in physical activity: review and update. Med Sci Sports Exerc. 2002;34(12):1996-2001. https://doi.org/10.1097/00005768-200212000-00020
- Jenkins F, Jenkins C, Gregoski MJ, Magwood GS. Interventions promoting physical activity in African American women: an integrative review. J Cardiovasc Nurs. 2017;32(1):22-29. https://doi.org/10.1097/JCN.0000000000000298
- Wallin BS. Building a Neighborhood Wellness Center in North Philadelphia: A Community Needs Assessment. MSPH Final Thesis. College of Graduate Studies: Thomas Jefferson University. Philadelphia, PA. Spring, 2008.
- Eat Right. Academy of Nutrition and Dietetics. https://www.eatright.org/. Accessed December 5, 2018.
- Wininger SR, Pargman D. Assessment of factors associated with exercise enjoyment. J Music Ther. 2003;40(1):57-73. https://doi.org/10.1093/jmt/40.1.57
- Eyler AA, Brownson RC, Donatelle RJ, King AC, Brown D, Sallis JF. Physical activity social support and middle- and older-aged minority women: results from a US survey. Soc Sci Med. 1999;49(6):781-789. https://doi.org/10.1016/S0277-9536(99)00137-9
- Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38(1):21-37. https://doi.org/10.2307/2955359
- Penedo FJ, Dahn JR. Exercise and well-being: a review of mental and physical health benefits associated with physical activity. Curr Opin Psychiatry. 2005;18(2):189-193. https://doi.org/10.1097/00001504-200503000-00013
- Walker RE, Keane CR, Burke JG. Disparities and access to healthy food in the United States: A review of food deserts literature. Health Place. 2010;16(5):876-884. https://doi.org/10.1016/j.healthplace.2010.04.013



There are no comments for this article.