As the population of the United States becomes more diverse, there is an increasing need for medical providers to be trained in collaborating with interpreters.1 The deleterious effects on patients’ health arising from language and cultural barriers are significant.2-7 While it is currently not feasible to provide all patients with limited English proficiency (LEP) a language-concordant provider, the incorporation of trained medical interpreters into their care has produced numerous benefits.8-11 Although medical schools12,13 and residency programs14 are developing training programs on provider-interpreter collaboration, no student-run free clinic (SRFC) has reported a similar effort in the literature. Our study establishes the first steps in examining a training program to teach third-year medical students (MS3s) to work effectively with in-person interpreters.
BRIEF REPORTS
Enhancing Medical Student-Interpreter Collaboration in an Urban Free Clinic
Alon Y. Mazori, BA | Maxim I. Maron, MS | Marika L. Osterbur Badhey, MS | Daniel Santos, MD | Virginia Folgado Marco, MS | Juan Lin, PhD | Amarilys Cortijo, MD | Sarah Nosal, MD | Ellie Schoenbaum, MD
Fam Med. 2019;51(7):593-597.
DOI: 10.22454/FamMed.2019.229662
Background and Objectives: Cultural barriers and patient-provider language discordance exert deleterious effects on patient care. One solution has been the integration of medical interpreters into the care of patients with limited English proficiency. While medical schools and residency programs have started developing training programs on how to work with medical interpreters, no similar endeavor has been reported by student-run free clinics.
Methods: Over 1 year, 76 third-year medical students (MS3s) were enrolled in control and intervention groups, and evaluated by in-person interpreters during interpreted real-patient encounters. MS3s in the intervention group received a lesson- and reminder-based training program on how to work with in-person interpreters.
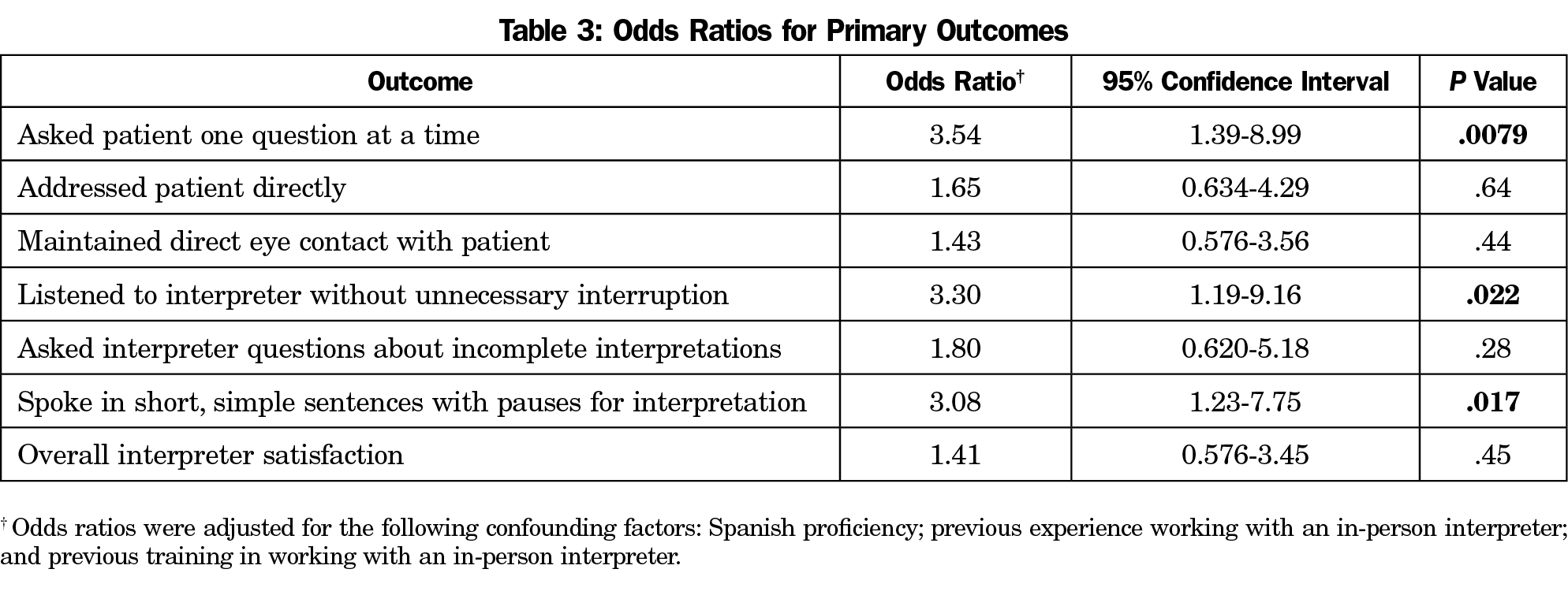
Results: MS3s who received the intervention were more likely to ask the patient one question at a time (odds ratio [OR] 3.54, P=.0079), listen to the interpreter without unnecessary interruption (OR 3.30, P=.022), and speak in short, simple sentences with pauses for interpretation (OR 3.08, P=.017).
Conclusions: Our lesson- and reminder-based training program on provider-interpreter collaboration can improve the performance of MS3s within a select skill set with minimal cost and time investment.
The Albert Einstein College of Medicine (Einstein) Institutional Review Board approved this study, which was conducted at the attending-supervised, student-run Einstein Community Health Outreach (ECHO) Free Clinic.
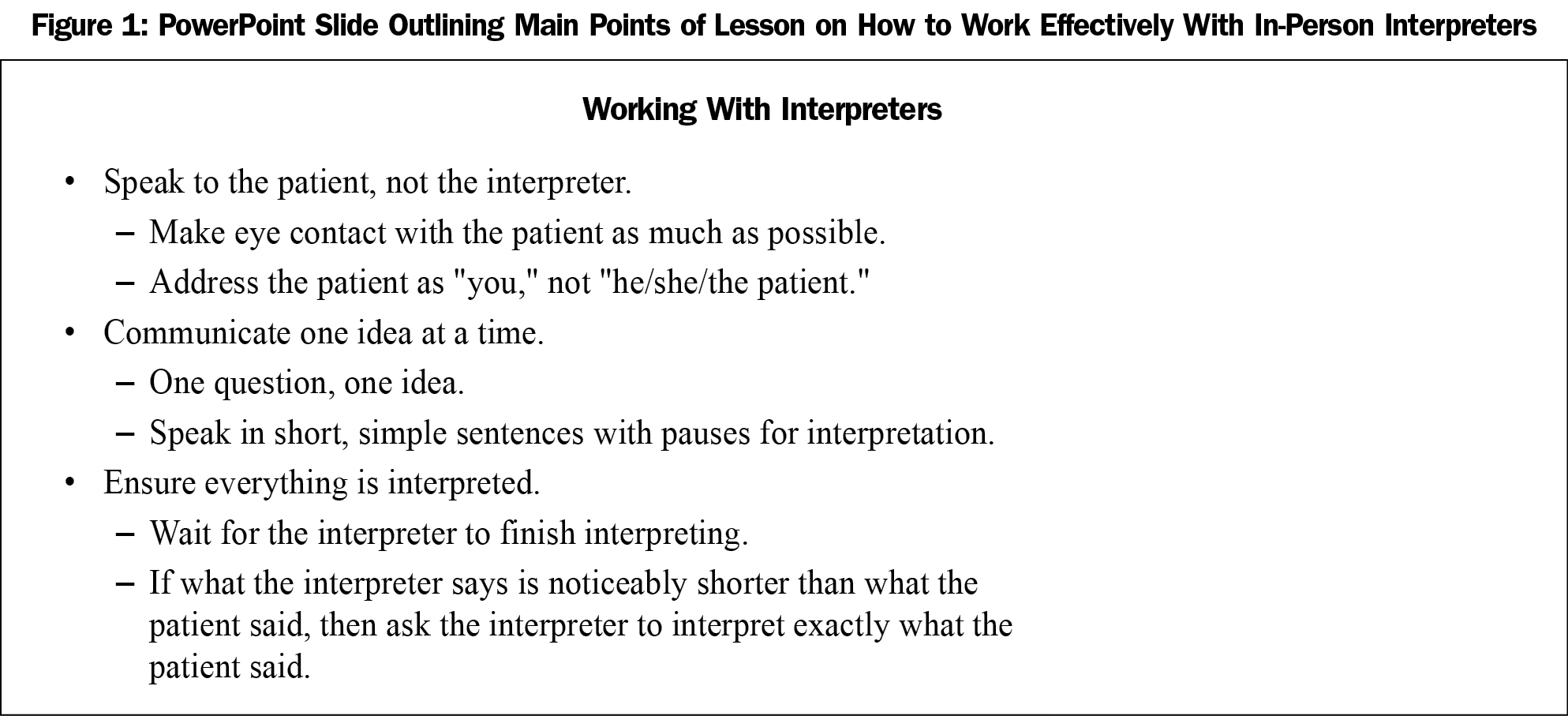
Einstein MS3s were enrolled during their month-long family-medicine clerkship between September 2016 and August 2017. MS3s were excluded if they self-rated as fluent in Spanish, did not attend ECHO, or did not work with an in-person Spanish interpreter. The study was divided into six 2-month cycles, with MS3 group assignment alternating between control group and intervention group each month. The intervention featured a PowerPoint-based lesson on how to work effectively with an in-person interpreter, and a reminder of the lesson’s main points at the start of the MS3s’ first shifts in clinic. The lesson conveyed guidelines derived from the literature (Figure 1).15-17
Data were collected through demographic surveys completed by the MS3s, and from evaluation forms filled out by the interpreters during patient encounters. Blinding of the interpreters was accomplished by restricting knowledge of MS3 group allocation status to study investigators. Interpreters were trained to use an MS3 evaluation form adapted from the Interpreter Scale,1 a validated instrument designed to enable a trained in-person interpreter to assess a medical trainee’s communication skills during an interpreted encounter. The evaluation form contained seven 5-point Likert scales. Scores of 5 were considered excellent performance; 4, moderate; and from 1 to 3, poor. Only data from the first MS3-interpreter encounter were included. Monthly spot checks were held to detect issues with the interpreters’ evaluation of the MS3s. Data were deidentified and stored in a HIPAA-compliant database.
Results were summarized as counts and compared between study groups with the χ2 test or Fisher exact test. Ordinal logistic regression analysis was performed to examine the association between the intervention and the interpreters’ scores for MS3 performance in each outcome, adjusting for baseline characteristics. Results were expressed as odds ratios (ORs) and corresponding 95% confidence intervals (CI). The ORs assessed whether MS3s in the intervention group were more likely to receive evaluations rated as (i) either moderate or excellent instead of poor, or (ii) excellent instead of either poor or moderate.
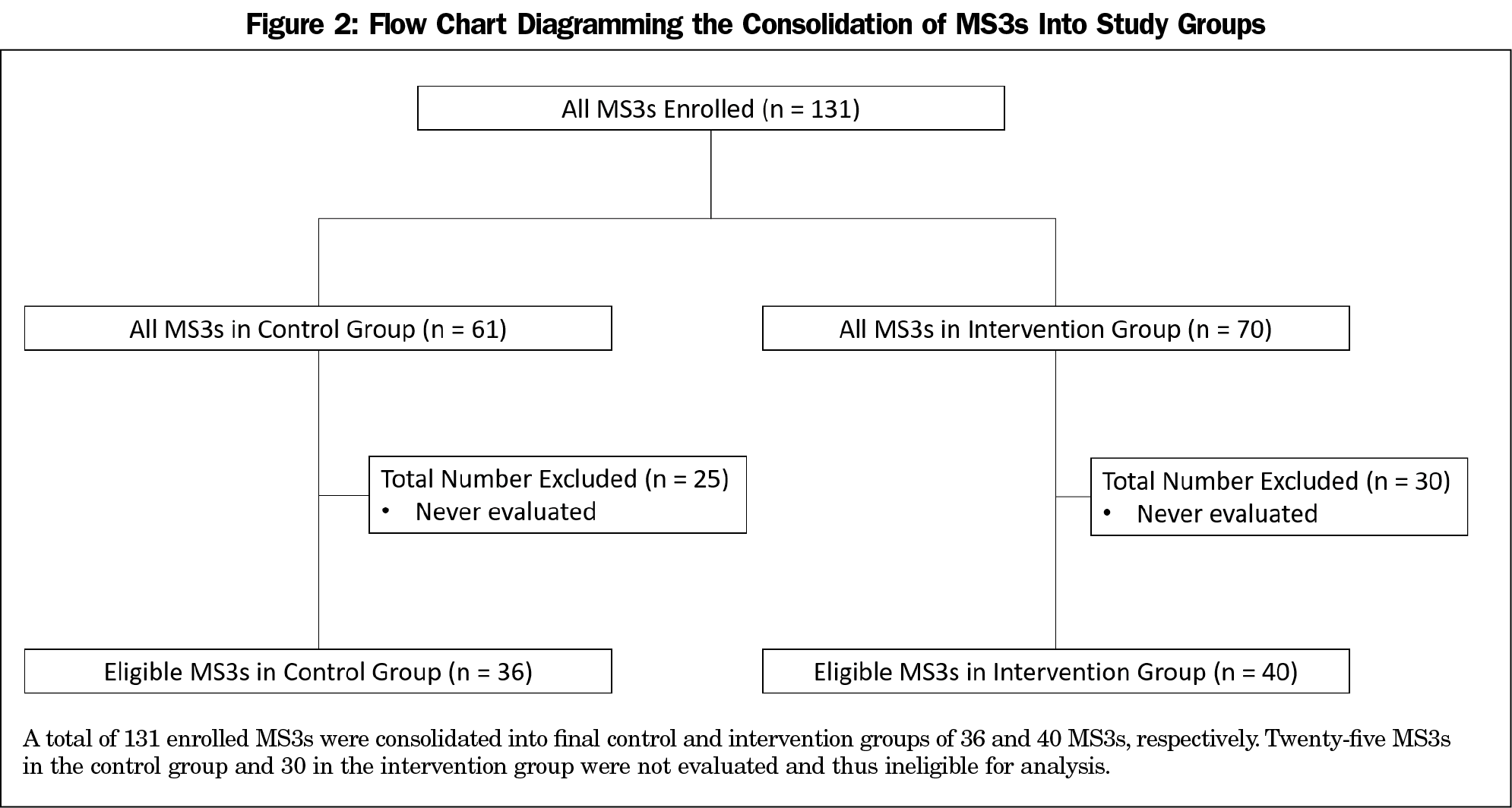
A total of 131 MS3s were enrolled and evaluation forms were completed for 76, yielding 36 in the control group and 40 in the intervention group; Figure 2 details this consolidation.
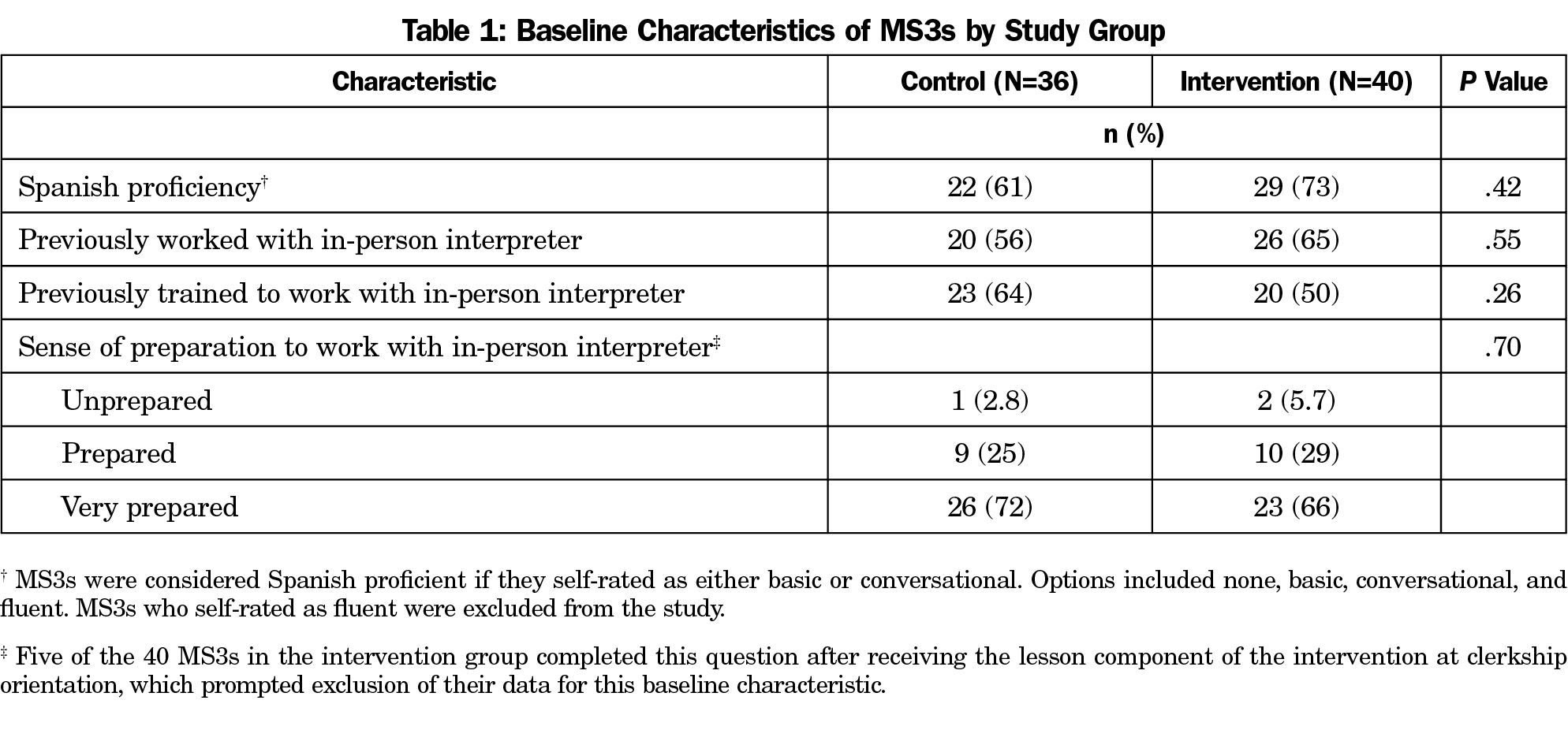
Baseline characteristics were balanced across study groups (Table 1). Most participants (i) self-rated as possessing basic or conversational Spanish proficiency, (ii) acknowledged having received training to work with an in-person interpreter, (iii) reported prior experience working with an in-person interpreter, and (iv) self-rated as very prepared to work with an in-person interpreter.
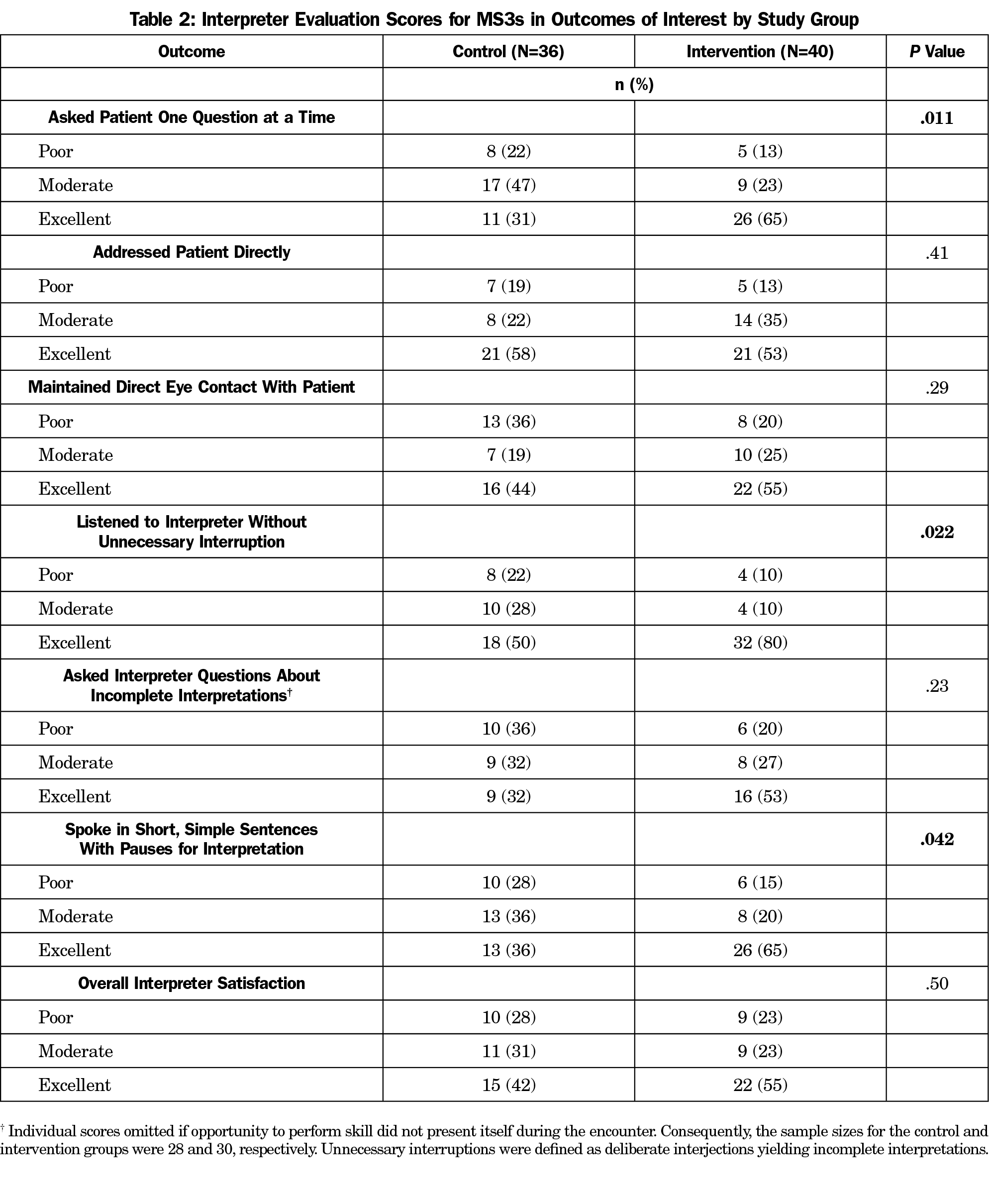
Table 2 displays the scores the interpreters assigned the MS3s; Table 3 depicts the corresponding ORs. MS3s in the intervention group exhibited higher performance in asking patients one question at a time (65% vs 31% scored excellent, P=.011; OR 3.54, P=.0079); listening to the interpreter without unnecessary interruption (80% vs 50% scored excellent, P=.022; OR 3.30, P=.022); and speaking in short, simple sentences with pauses for interpretation (65% vs. 36% scored excellent, P=.042; OR 3.08, P=.017). Statistical analysis for confounding factors demonstrated that our results were independent of Spanish proficiency, previous experience working with an in-person interpreter, and previous training in working with an in-person interpreter. Monthly interpreter spot checks uncovered no problems or inconsistencies.
Our study examined the effectiveness of a lesson- and reminder-based intervention to promote collaboration between MS3s and in-person Spanish interpreters. The results revealed that MS3s who received the intervention were more likely to ask the patient one question at a time, listen to the interpreter without unnecessary interruption, and speak in short, simple sentences with pauses for interpretation. Moreover, these results were independent of the MS3s’ self-rated Spanish proficiency and previous experience or training in working with an in-person interpreter.
Our study design enabled close query of our intervention. Delivery of the intervention and MS3 evaluation were executed in a standardized fashion. The interpreters remained blinded throughout the study. In addition, the alternating nature of the 2-month cycles allowed for better control of bias originating from clinical experience gained through other third-year clerkships.
Importantly, our study also had limitations. Our sample size was restricted because not all enrolled MS3s were evaluated, and our nonrandomized study design may have influenced our results beyond our ability to adjust. Our study was also limited by the evaluation scale we employed. As we were unable to locate a scale validated for evaluation of medical trainees by interpreters in real-patient encounters, we adapted our scale from the Interpreter Scale,1 which had been validated for this purpose within standardized-patient encounters.
Our project is particularly relevant for primary care clinics and SRFCs. Moreover, our study outcomes are derived from literature-based guidelines15-17 to promote provider-interpreter collaboration, which improves outcomes for patients with LEP.8-11,18 While further research is necessary, this intervention can help improve care for patients with LEP with minimal cost and time investment.
This study represents the first reported endeavor by an SRFC to train its medical students to work with interpreters. Our training program on provider-interpreter collaboration can improve the performance of MS3s with respect to a select set of communication skills. Further research is required to extend the training program’s impact and analyze its effect on patient-provider communication.
Acknowledgments
Preliminary results from this project were presented as a poster at the 2017 Society of Student Run Free Clinics Annual Conference, February 12, 2017, in Anaheim, CA.
References
- Lie D, Bereknyei S, Braddock CH III, Encinas J, Ahearn S, Boker JR. Assessing medical students’ skills in working with interpreters during patient encounters: a validation study of the Interpreter Scale. Acad Med. 2009;84(5):643-650. https://doi.org/10.1097/ACM.0b013e31819faec8
- Carrasquillo O, Orav EJ, Brennan TA, Burstin HR. Impact of language barriers on patient satisfaction in an emergency department. J Gen Intern Med. 1999;14(2):82-87. https://doi.org/10.1046/j.1525-1497.1999.00293.x
- Ramirez D, Engel KG, Tang TS. Language interpreter utilization in the emergency department setting: a clinical review. J Health Care Poor Underserved. 2008;19(2):352-362. https://doi.org/10.1353/hpu.0.0019
- De Alba I, Sweningson JM. English proficiency and physicians’ recommendation of Pap smears among Hispanics. Cancer Detect Prev. 2006;30(3):292-296. https://doi.org/10.1016/j.cdp.2006.05.003
- Bard MR, Goettler CE, Schenarts PJ, et al. Language barrier leads to the unnecessary intubation of trauma patients. Am Surg. 2004;70(9):783-786.
- Bernstein J, Bernstein E, Dave A, et al. Trained medical interpreters in the emergency department: effects on services, subsequent charges, and follow-up. J Immigr Health. 2002;4(4):171-176. https://doi.org/10.1023/A:1020125425820
- Waxman MA, Levitt MA. Are diagnostic testing and admission rates higher in non-English-speaking versus English-speaking patients in the emergency department? Ann Emerg Med. 2000;36(5):456-461. https://doi.org/10.1016/S0196-0644(00)02470-7
- Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev. 2005;62(3):255-299. https://doi.org/10.1177/1077558705275416
- Juckett G, Unger K. Appropriate use of medical interpreters. Am Fam Physician. 2014;90(7):476-480.
- Bagchi AD, Dale S, Verbitsky-Savitz N, Andrecheck S, Zavotsky K, Eisenstein R. Examining effectiveness of medical interpreters in emergency departments for Spanish-speaking patients with limited english proficiency: results of a randomized controlled trial. Ann Emerg Med 2011;57(3):248-56 e1-4.
- Karliner LS, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42(2):727-754. https://doi.org/10.1111/j.1475-6773.2006.00629.x
- McEvoy M, Santos MT, Marzan M, Green EH, Milan FB. Teaching medical students how to use interpreters: a three year experience. Med Educ Online. 2009;14(1):12. https://doi.org/10.3402/meo.v14i.4507
- Vela M, Fritz C, Jacobs EA. Establishing medical students’ cultural and linguistic competence for the care of Spanish-speaking limited English proficient patients. J Racial Ethn Health Disparities. 2016;3(3):484-488. https://doi.org/10.1007/s40615-015-0165-0
- Pagels P, Kindratt T, Arnold D, Brandt J, Woodfin G, Gimpel N. Training family medicine residents in effective communication skills while utilizing promotoras as standardized patients in OSCEs: a health literacy curriculum. Int J Family Med. 2015;2015:129187. https://doi.org/10.1155/2015/129187
- Herndon E, Joyce L. Getting the most from language interpreters. Fam Pract Manag. 2004;11(6):37-40.
- Hadziabdic E, Hjelm K. Working with interpreters: practical advice for use of an interpreter in healthcare. Int J Evid-Based Healthc. 2013;11(1):69-76. https://doi.org/10.1111/1744-1609.12005
- Lie D, Boker J, Bereknyei S, Ahearn S, Fesko C, Lenahan P. Validating measures of third year medical students’ use of interpreters by standardized patients and faculty observers. J Gen Intern Med. 2007;22(S2)(suppl 2):336-340. https://doi.org/10.1007/s11606-007-0349-3
- Ku L, Flores G. Pay now or pay later: providing interpreter services in health care. Health Aff (Millwood). 2005;24(2):435-444. https://doi.org/10.1377/hlthaff.24.2.435
Lead Author
Alon Y. Mazori, BA
Affiliations: Albert Einstein College of Medicine, Bronx, NY. Mr Mazori and Mr Maron contributed equally to this study.
Co-Authors
Maxim I. Maron, MS - Albert Einstein College of Medicine, Bronx, NY
Marika L. Osterbur Badhey, MS - Albert Einstein College of Medicine, Bronx, NY
Daniel Santos, MD - Albert Einstein College of Medicine, Bronx, NY
Virginia Folgado Marco, MS - Albert Einstein College of Medicine, Bronx, NY
Juan Lin, PhD - Albert Einstein College of Medicine, Bronx, NY
Amarilys Cortijo, MD - Institute for Family Health, Bronx, NY
Sarah Nosal, MD - Institute for Family Health, Bronx, NY
Ellie Schoenbaum, MD - Albert Einstein College of Medicine, Bronx, NY
Corresponding Author
Ellie Schoenbaum, MD
Correspondence: Albert Einstein College of Medicine, Jack and Pearl Resnick Campus, 1300 Morris Park Avenue, Block Building, Room 518, The Bronx, NY 10461. 718-430-2518. Fax: 718-430-2521.
Fetching other articles... 
Loading the comment form... 
Submitting your comment... 


There are no comments for this article.