Background and Objectives: Screening for and addressing food insecurity in primary care may improve associated comorbidities. The purpose of this study was to explore patient attitudes regarding screening for food insecurity and to elicit patient preferences for intervention in a primary care setting.
Methods: Patients (N=284) completed a brief, voluntary survey in a university-based clinic and two community-based clinics over a 5-month period. Respondents were classified as either food-secure or food-insecure based on their responses to a validated food insecurity screener.
Results: Participants stated that screening for food insecurity was valuable in the primary care setting (83.9%). Patients preferred having a nurse ask the screening questions (41.2%). The most popular intervention preference, regardless of food security status or clinic type, was to provide a list of food bank locations (76.4%) and local community organizations (71.6%) and to have referral to financial assistance programs (75.4%). There were no differences in preferences for screening or attitudes toward screening by food security status or clinic type (all P≥.05).
Conclusions: Screening for food insecurity is not yet standard practice, partly due to concerns over potentially alienating patients with the screening questions. Based on our surveyed patient population and their indicated preferences, screening and providing resource referrals for food insecurity is not likely to damage the clinician-patient relationship.
Food insecurity (FI) is defined as the disruption of food intake or eating patterns because of lack of money and other resources.1 FI correlates with low household income and currently has a prevalence of about 1 in 8 households in the United States.2,3 Being food insecure is associated with poorer health outcomes in routinely managed conditions including obesity, 4 hypertension and hyperlipidemia,5 diabetes,6-8 hypoglycemia,9 chronic kidney disease,10 and frailty in the elderly.11
Between 2015 and 2017, the United States Department of Agriculture (USDA) reported 17.4% of Arkansas households had food insecurity, and 6.5% of Arkansas households had very low food security.12 Arkansas ranked second for rates in food insecurity in the United States, with more than 560,000 people who are food insecure (17.2%) in 2018.12 Food insecurity rates among blacks (23.7%) are much higher than whites (7.3%) in the Delta region.13 Given the health risks associated with food insecurity and the high rates in the state of Arkansas, FI is likely to be a prominent factor influencing health.
FI can affect many patients in family medicine practice—though this may go unrecognized without screening. Further, health outcomes associated with addressing food insecurity can improve with intervention.14 Despite recognizing the benefits to screening for and addressing FI, there have not been widespread primary care efforts for FI screening.15 Barriers to routine screening include fear of reducing patient satisfaction,16 fear of damaging the patient-physician relationship (eg, shame may prompt dishonest responses),17 lack of time to conduct screening, and uncertainty with managing a positive screen.18 The aim of this project was to explore patient attitudes and intervention preferences in the primary care setting. Specifically, the study objectives were (1) to evaluate FI prevalence, (2) to examine patient attitudes towards FI screening by food security status, and (3) to identify what interventions patients with FI preferred. In so doing, the study sought to provide data to support or refute previously documented barriers to FI screening.
Setting and Study Population
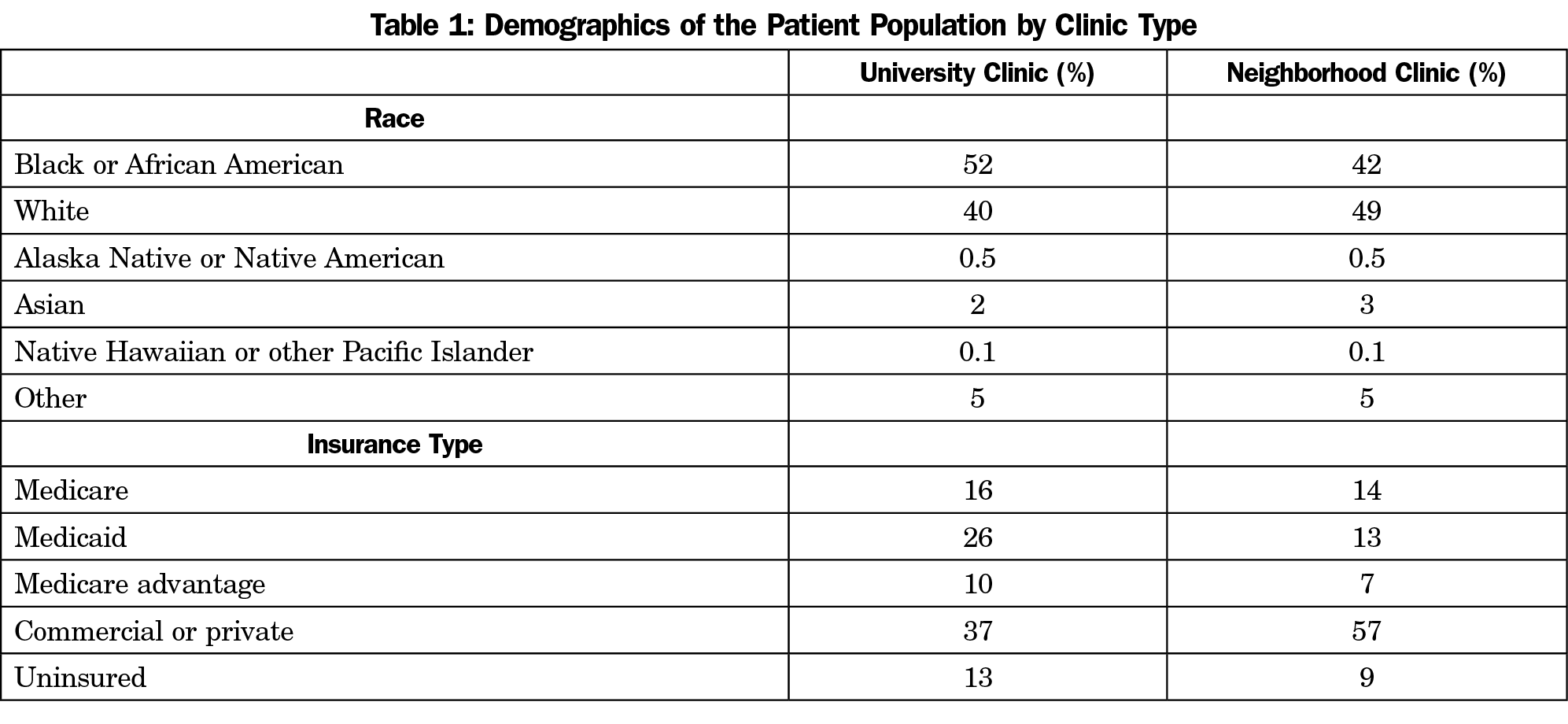
Three different primary care clinics of an academic hospital in a southern state of the United States participated. Table 1 provides information on the race and insurance of patients at the two clinic types. Combined, clinics served approximately 3,000 patients during the study period. Only patients over 18 years of age completed the survey. The institutional Institutional Reveiew Board approved this study under exempt status.
Survey Design
We designed a one-page surveyhat consisted of eight questions including an adapted, brief version of the USDA’s food security survey module to screen for food insecurity.13 The brief screener had previously demonstrated 97% sensitivity in identifying food insecurity compared to the full USDA screen.19 The survey also explored patients’ attitudes and intervention preferences regarding food insecurity.
Survey Administration
The study team conducted the survey in 2018, and all adult patients who presented to the clinics during the study period were eligible. We educated front desk staff of participating primary care clinics about this study and aided in survey distribution, explaining the survey objectives and the patients’ right to anonymity. Patients completed surveys in the waiting room lobby prior to seeing a clinician. Participants did not receive any type of incentive to take part in this study. Study staff asked participants not to complete the survey during their follow-up visits. Study staff were not available to administer the survey verbally, which may have unintentionally excluded patients with poor literacy, lack of proficiency in English, or significant visual impairment. There were no formal exclusion criteria.
Data Analysis
The survey explored patients’ attitudes and intervention preferences regarding food insecurity. Researchers assigned participants a food security status—either food secure or food insecure—during data interpretation, consistent with prior scoring recommendations. Researchers presented patient attitude questions in a Likert scale format and used one-sample t tests for assessing differences between groups on these items. Researchers used χ2 tests to assess differences between groups regarding binary options (yes/no) when asking if patients felt a specific intervention would be helpful. Significance was set at α<.05.
Respondents
A total of 284 participantscompleted the FI questionnaire. About 75% of the surveys were university campus patients (n=212), and 25% of the surveys were neighborhood clinic patients (n=72). Many patients (40.8%) indicated food insecurity with higher rates in the university clinic (42.9%) than in the neighborhood clinic (34.7%). This difference was not significant in a c2 comparison (χ2 = 1.50, P=.22).
Preference for Screening
Most patients indicated it was important to ask about food insecurity (83.9%), and there were no differences on this attitude by patient food security status (t [277]=-0.74, P=.46) or clinic type (t [277]=-1.23, P=.22). Overall, patients preferred having a nurse ask about food security (41.2%) or completing a short survey on paper (33.5%) versus having a doctor ask (18.7% preferred this option). There were no differences in preference of administration mode based on food security (c2=0.12, P=.73) status or clinic type (c2=4.32, P=.12).
Attitudes About Screening
Most agreed or strongly agreed that asking about food insecurity would show patients that the clinic cared (82.7%) and that FI assessment would improve care (73.2%). Few agreed or strongly agreed that it would waste their time (11.7%). T-test comparisons for each of these items for FI status were not significant (all P<.42), nor was the clinic type comparison for the item on showing care (P=.39) or wasting time (P=.05).
Regarding their personal experience with a food insecurity screen, few patients agreed or strongly agreed that they would be embarrassed (21.6%) or offended (12.1%). Patients did not differ by food security status on feelings of being offended (P=.11) or being embarrassed (P=.06) in t-test comparisons. Clinic types did not differ on possible feelings of embarrassment (P=.24) or offense (P=.05).
Most participants agreed or strongly agreed that they would be comfortable telling the truth (78.3%) and would feel better-understood (67.9%) when screened for food security. There were no significant differences found between food security statuses (all P>.12) or clinic types regarding these values (all P>.17). Table 2 presents means and standard deviations for each item by group as well as t-test and significance values for each comparison.
Preference for Referral
The most popular preferences for referral were a list of food bank locations (76.4%), help with signing up for financial assistance programs (75.4%), and information about local community organizations (71.6%). More than half of participants expressed an interest in farmer’s markets locations (66.4%) and referral to nutritionists (54.3%). There were no significant differences in preference for referral types by clinic type (χ2 =3.17, P=.08). While food insecure patients were more likely to indicate they would rather not discuss their personal food security status than the food secure group (χ2=4.87, P=.03; Z=1.5), a majority (70.8%) of patients with food insecurity did prefer to discuss this topic in clinic. Table 3 presents percentages of endorsement by food security status as well as χ2 and significance values.
This study provides patients’ perspectives about food insecurity in our primary care clinics. This study found a higher than average prevalence of food insecurity in our patient population (40.8%).1,2 Overall, most participants seemed to value having their clinic screen for food insecurity. The largely similar responses on preference for screening and referral between the two groups suggests that approaches to address food security could be applied equally across food security status.
The current study addresses several previously identified barriers to FI screening. First, these data suggest that addressing FI is not likely to damage the clinician-patient relationship, contrary to previous concerns.17-20 In our survey, patients received FI screening well and reported high levels of acceptability about FI screening. Second, a previously identified barrier to screening is clinician uncertainty with managing a positive screen.18 Respondents in our study favored assistance with resource acquisition. Social workers could help facilitate this by discussing nutrition assistance programs and providing a list of local resources. Third, a previously identified barrier to screening was concern for patient comfort. Most of the respondents in our study felt comfortable and would not feel embarrassed regarding FI screening. Finally, time to complete the screen is a clinician-cited barrier.18 However, in our study, participants preferred for screens to be administered either by the nursing staff or via paper survey. Either method would minimize impact on clinician encounter time.
This study has several limitations and strengths. Given the nature of convenience sampling, small sample size, restriction to English-speaking patients, and urban patient population, the generalizability of our findings may be limited.21,22 Replication of this survey at other clinical sites is recommended. Further, our study did not include the participants’ demographics on the survey. This limits our ability to conduct comparisons or draw conclusions on patient preferences by these salient characteristics.
A key strength of our study is the high rate of black/African American patients. African American households face food insecurity and hunger at higher rates than whites. 22, 23 Developing and maintaining trust with patients of color is critical to providing high-quality care to this population who suffer from health disparities.24,25 Addressing food insecurity for this population may aid in that goal.
Screening for FI is not yet standard practice due, in part, to concerns over potentially alienating patients. Based on our surveyed patient population and their indicated preferences, screening and providing resource referrals for food insecurity is not likely to damage the clinician-patient relationship. Universal FI screening, particularly with patient populations who bear the burden of health disparities, may improve patient care and health outcomes.
References
- Nord M, Andrews M, Carlson S. Household food security in the United States, 2005. Washington, DC: USDA Economic Research Service; 2005. Report No.: ERR-29. https://www.ers.usda.gov/webdocs/publications/45655/29206_err29_002.pdf?v=41334. Accessed July 25, 2019.
2.Feeding America. Foods Insecurity in The United States. 2018. http://map.feedingamerica.org. Accessed March 11, 2019.
3.Carlson SJ, Andrew MS, Bickel GW. Measuring food insecurity and hunger in the United States: development of a national benchmark measure and prevalence estimates. J Nutr. 1999;129, 2S Suppl: 510S-516S. https://doi.org/10.1093/jn/129.2.510S
- Karnik A, Foster BA, Mayer V, et al. Food insecurity and obesity in New York City primary care clinics. Med Care. 2011;49(7):658-661. https://doi.org/10.1097/MLR.0b013e31820fb967
- Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010;140(2):304-310. https://doi.org/10.3945/jn.109.112573
- Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999-2002. J Gen Intern Med. 2007;22(7):1018-1023. https://doi.org/10.1007/s11606-007-0192-6
- Berkowitz SA, Karter AJ, Corbie-Smith G, et al. Food insecurity, food "deserts," and glycemic control in patients with diabetes: a longitudinal analysis. Diabetes Care. 2018;41(6):1188–1195. https://doi.org/10.2337/dc17-1981
- Silverman J, Krieger J, Kiefer M, Hebert P, Robinson J, Nelson K. The Relationship Between Food Insecurity and Depression, Diabetes Distress and Medication Adherence Among Low-Income Patients with Poorly-Controlled Diabetes. J Gen Intern Med. 2015;30(10):1476-1480. https://doi.org/10.1007/s11606-015-3351-1
- Seligman HK, Davis TC, Schillinger D, Wolf MS. Food insecurity is associated with hypoglycemia and poor diabetes self-management in a low-income sample with diabetes. J Health Care Poor Underserved. 2010;21(4):1227-1233. https://doi.org/10.1353/hpu.2010.0921
- Banerjee T, Crews DC, Wesson DE, et al; CDC CKD Surveillance Team. Food insecurity, CKD, and subsequent ESRD in US adults. Am J Kidney Dis. 2017;70(1):38-47. https://doi.org/10.1053/j.ajkd.2016.10.035
- Wolfe WS, Olson CM, Kendall A, Frongillo EA Jr. Hunger and food insecurity in the elderly: its nature and measurement. J Aging Health. 1998;10(3):327-350. https://doi.org/10.1177/089826439801000304
- United States Department of Agriculture Economic Research Service. Fact Sheet: Arkansas. https://data.ers.usda.gov/reports.aspx?StateFIPS=05&StateName=Arkansas&ID=17854. Accessed July 25, 2019.
- Stuff JE, Horton JA, Bogle ML, et al; Lower Mississippi Delta Nutrition Intervention Research Consortium. High prevalence of food insecurity and hunger in households in the rural Lower Mississippi Delta. J Rural Health. 2004;20(2):173-180. https://doi.org/10.1111/j.1748-0361.2004.tb00025.x
- Carlson S, Keith-Jennings B. SNAP Is Linked with Improved Nutritional Outcomes and Lower Heath Care Costs. Center on Budget and Policy Priorities. Washington, DC: Center on Budget and Policy Priorities; 2018. https://www.cbpp.org/sites/default/files/atoms/files/1-17-18fa.pdf. Accessed November 20, 2019.
- Hoisington AT, Braverman MT, Hargunani DE, Adams EJ, Alto CL. Health care providers’ attention to food insecurity in households with children. Prev Med. Baltim; 2012. https://doi.org/10.1016/j.ypmed.2012.06.007
- Adams E, Hargunani D, Hoffmann L, Blaschke G, Helm J, Koehler A. Screening for food insecurity in pediatric primary care: a clinic’s positive implementation experiences. J Health Care Poor Underserved. 2017;28(1):24-29. https://doi.org/10.1353/hpu.2017.0004
- Bloch G, Rozmovits L, Giambrone B. Barriers to primary care responsiveness to poverty as a risk factor for health. BMC Fam Pract. 2011;12(1):62. https://doi.org/10.1186/1471-2296-12-62
- Barnidge E, LaBarge G, Krupsky K, Arthur J. Screening for food insecurity in pediatric clinical settings: opportunities and barriers. J Community Health. 2017;42(1):51-57. https://doi.org/10.1007/s10900-016-0229-z
- Hager ER, Quigg AM, Black MM, et al Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics (Evanston). 2010;126 (1), p. e26.
- Shih S, Holben D, Holcomb JP Jr. Self-identified knowledge and practices of family physicians in Appalachian Ohio regarding food acquisition of patients. J Am Diet Assoc. 2004;104(11):1718-1721. https://doi.org/10.1016/j.jada.2004.08.003
- Vedovato GM, Surkan PJ, Jones-Smith J, et al. Food insecurity, overweight and obesity among low-income African-American families in Baltimore City: associations with food-related perceptions. Public Health Nutr. 2016;19(8):1405-1416. https://doi.org/10.1017/S1368980015002888
- Zekeri AA, Nnedu CC, Popoola S, Diabate Y. Household food insecurity and health among African American women in black belt counties of Alabama: evidence from mixed-methods research. J Comm Pub Health Nurs. 2016;2(138):2. https://doi.org/10.4172/2471-9846.1000138
- Feeding America. Hunger in America. www.feedingamerica.org/hunger-in-america/african-american. Accessed August 9, 2019.
- Jacobs EA, Rolle I, Ferrans CE, Whitaker EE, Warnecke RB. Understanding African Americans’ views of the trustworthiness of physicians. J Gen Intern Med. 2006;21(6):642-647. https://doi.org/10.1111/j.1525-1497.2006.00485.x
- Gamble VN. (1993). A legacy of distrust: African Americans and medical research. American Journal of Preventive Medicine. 1993;9(6)Suppl.35-38.




There are no comments for this article.