Background and Objectives: With the emergence of COVID-19, telemedicine use has increased dramatically as clinicians and patients have looked for alternatives to face-to-face care. Prior research has shown high levels of patient satisfaction and comparable quality of care. Video visits have been hypothesized to be one way to reduce burnout among clinicians, but there has been minimal research on physician views of virtual care. We sought to measure family physician experience with video visits at the start of the COVID-19 pandemic.
Methods: We identified all faculty and resident physicians at a large academic department of family medicine who had conducted a video visit in the prior month and conducted an anonymous online 12-question survey about their experiences, satisfaction, and barriers with care.
Results: Most eligible physicians responded (102/109, 94%), of whom half (52%) reported this was their first month trying a video visit. There was very high satisfaction (91% very or somewhat satisfied). The majority of respondents felt that video visits were shorter (54%) or took the same amount of time (38%) as in-person visits. There was concern that many physicians had experienced a visit in which they felt video was not the appropriate platform given patient concerns.
Conclusions: This study is among the first to assess physician experience with video visits. As the visits are perceived as shorter, they may offer a unique opportunity to address clinician burnout. There was a high level of satisfaction at our institution despite multiple technical challenges.
Telemedicine has evolved over the last decade, and studies show comparable levels of patient satisfaction compared with in-person visits for general medical care, prenatal care, urgent care, and specialty care.1-5 Outcomes measures show similar quality,3,6,7 while patients report substantial reduction in travel time and expenses.5,8 While most studies have focused on patient experience, the National Quality Forum recommended that clinician experience be one of the metrics included in telehealth evaluation. Telemedicine has been hypothesized to reduce clinician burnout by increasing efficiency, reducing commuting time, and improving work/life balance.10-12 The modality might help extend care for specialties with limited workforce including psychiatry and specialty care.13,14 Among family physicians, it has already been shown to be twice as common among those working in rural settings.15
Our department began to implement video visits for a narrow scope of patient problems in 2017. Physicians anecdotally reported video visits were often shorter and provided a few extra minutes to catch up with administrative tasks during a busy clinic day. We hypothesized that these visits might have benefit as a burnout intervention and in early 2019 developed a survey about physician experience. As there were only a few video visits monthly at that time, we delayed the study while the department increased physician training around video visits. In mid-March 2020, the first COVID-19 positive patients were diagnosed in our state, and within days our institution severely restricted in-person visits and pivoted to virtual care. Our department conducted 13 video visits in February 2020, 609 in March, and 2,800 in April. Although the rapid uptake of video visits was related to the pandemic rather than a burnout intervention, we took advantage of the situation to assess physician experiences with virtual care.
No validated instruments to measure physician experience with telemedicine existed, so we developed a questionnaire based on existing literature and (with permission) a patient survey on video visits used by a large urban medical center.5 We developed the anonymous survey on Qualtrics and piloted it among physicians (Appendix 1). Domains included prior experience with video visits, satisfaction, barriers, and impact on stress, time, and documentation. We included minimal questions on demographics to ensure anonymity given the small sample size. Two questions were closed-ended, eight were 5-point Likert scale questions (ranging from strongly disagree to strongly agree), and two open-ended questions assessed “anything you didn’t like” or “anything you especially liked” about video visits. For the qualitative data, we reviewed the comments and developed a code book to identify distinct topics; two authors (K.M.H. and A.R.L.) independently coded the comments, and any disagreements were resolved by a third reviewer (K.J.G.). We performed a basic thematic analysis given the small amount of data. We used electronic health records to identify faculty and resident family medicine physicians who conducted a video visit between March 21, 2020 and April 21, 2020, and sent an email containing a survey link. Participants could register for a gift card drawing. The research was approved by the University of Michigan Institutional Review Board.
Among subjects, 102 of 109 (94%) eligible physicians participated between April 23 and May 11, 2020. All questions had less than 4% missing data except gender which was only answered by 35% of respondents and so was not utilized. For the open-ended questions, we received 28 responses from 23 different physicians.
Half of respondents (53, 52%) reported that this had been their first month conducting a video visit. Physicians indicated high satisfaction with 48 (48%) very satisfied and 43 (43%) somewhat satisfied with video visits, and most agreeing they were a good alternative to a face to face visit (42% strongly agree and 56% agree). The majority found it easy to connect (39% strongly agree, 57% agree), and would do another video visit if given the opportunity (64% strongly agree, 34% agree). Satisfaction did not differ between those doing their first month of visits and those with prior experience (P=.330). One-fifth of physicians reported that video visits increased their stress which was more common among those new to video visits, but not statistically significant (23% versus 15%, P=.279).
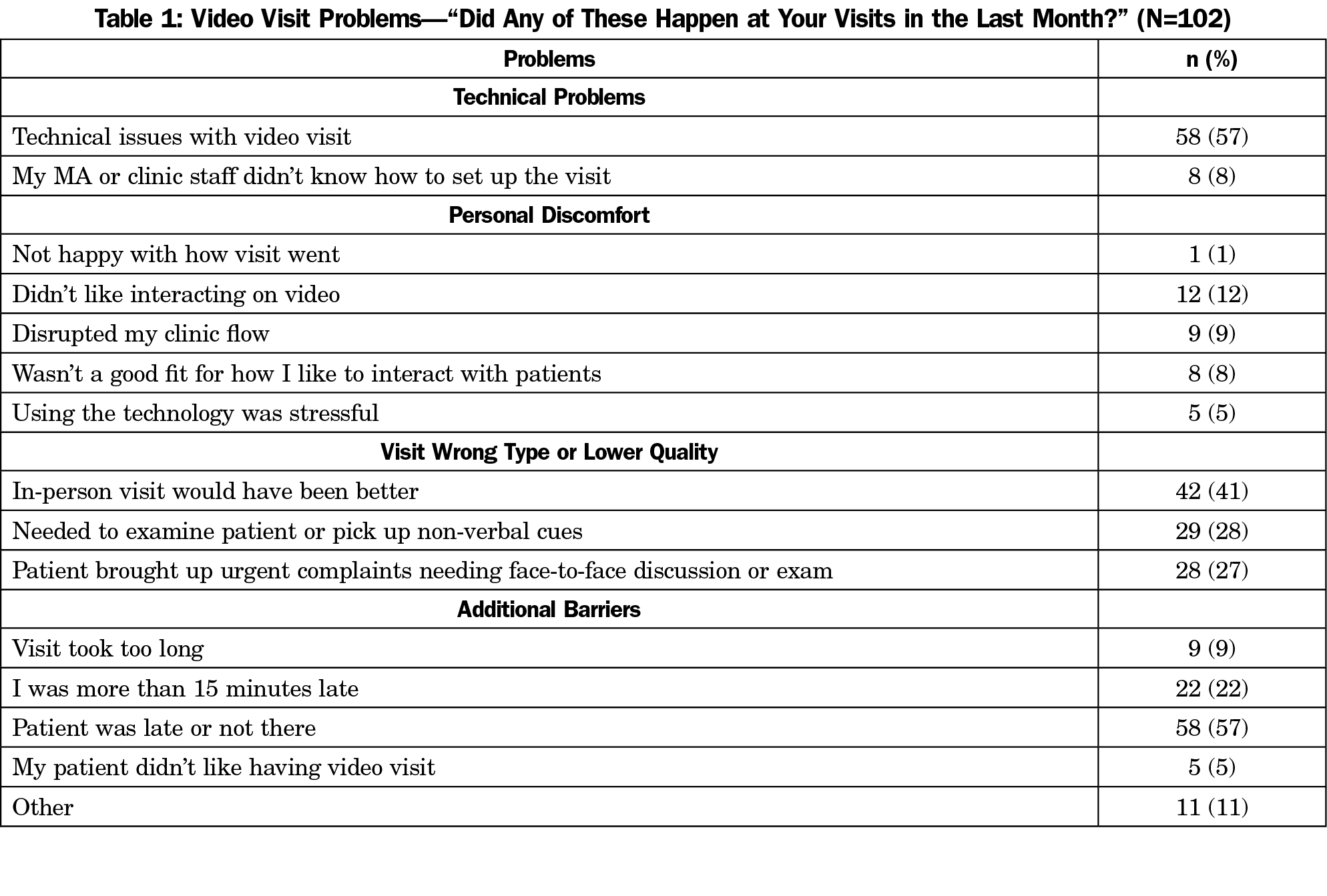
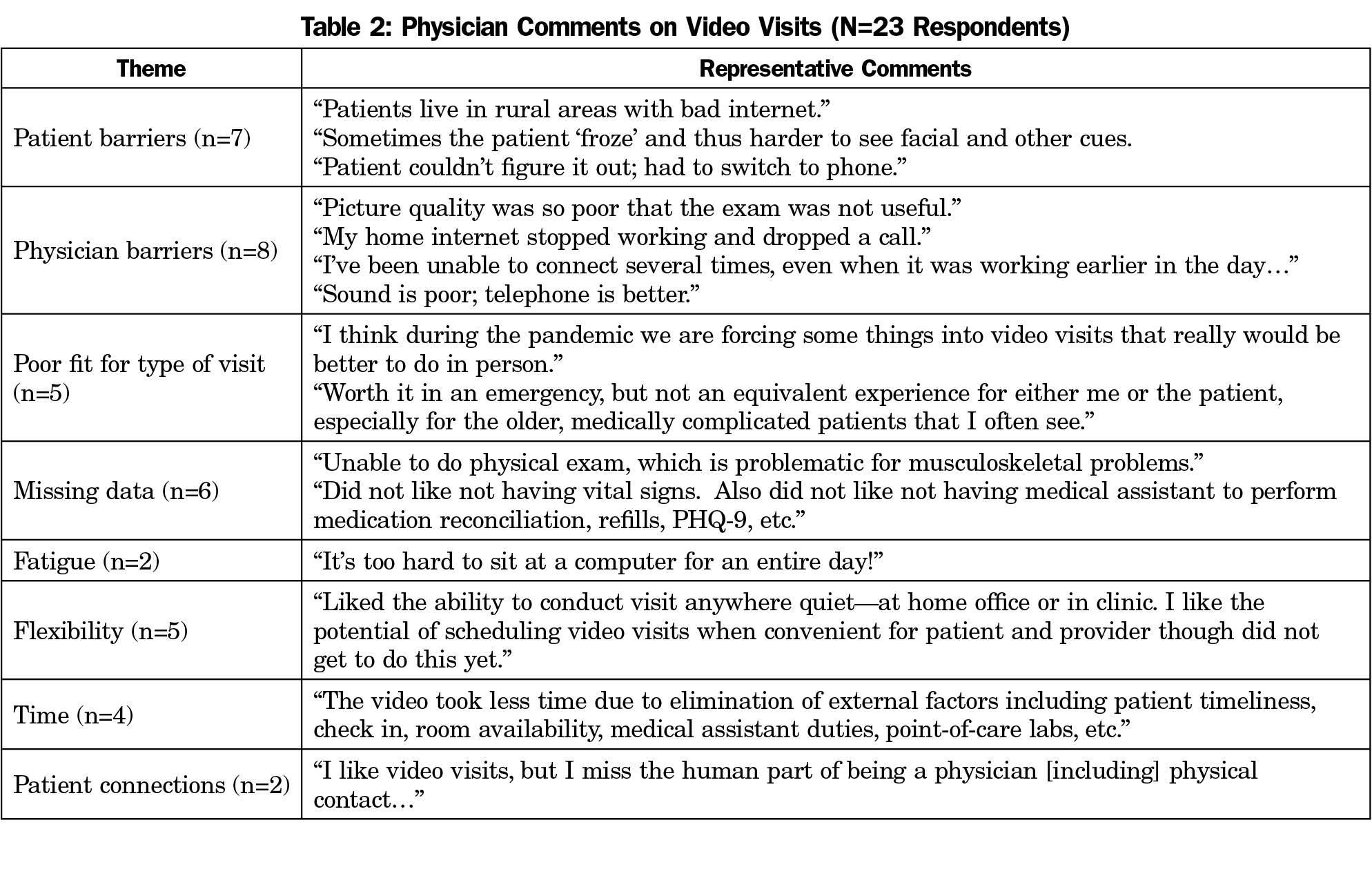
Sixty (59%) physicians identified a barrier related to technical access, 25 (25%) found visits conflicted with personal style or preferences for delivering care, and 53 (52%) identified video as inferior to a face-to-face visit for the presenting problem or issue (Table 1). Qualitative comments reinforced the technical challenges with physicians reporting problems with internet connections, patient confusion or difficulty connecting, and technical problems at the institutional level related to supporting a rapid ramp-up of virtual care. The majority of respondents (54, 54%) agreed that video visits took less time than traditional visits and these participants reported an average of 8 (+/-3) minutes less, with a range of 2-12 minutes less. Thirty-eight (38%) respondents noted the time was about the same. Only eight (8%) reported video visits took more time, with the average increase in time being 7 (+/-4) minutes and a range of 2-20 minutes more. Among the qualitative responses, the most common concerns involved patient confusion or technical barriers for both patients and physicians. Several respondents mentioned that the televisits did not seem appropriate for certain types of visits, and a number commented on missing important information during the visit. The themes are summarized in Table 2.
The sudden uptake of video visits in primary care due to the pandemic offered a natural experiment to assess family physician experiences. While video visits were new to half of the physicians in our study, results show high levels of satisfaction with minimal barriers to care. Most found the visits shorter, which mirrors time-savings reported by patients.6,8 The survey did not specifically assess satisfaction with working from home or flexibility, but these may be important components for reducing burnout. Subsequent surveys will address these topics in more depth and review acceptance and barriers as physicians become more familiar with video care over time and the institution shifts to a balance between virtual and face-to-face care. A significant number of physicians reported a video visit had been the wrong platform for care based on the need for physical exam, lack of nonverbal cues, or type of patient complaint. Learning how best to match patient concerns with visit type will be important for future research.
This is among first studies to assess the experience of family physicians using video visits in the COVID-19 era. As the survey was developed pre-COVID, some questions were less relevant given the sudden changes in primary care during the pandemic and as no validated surveys exist at this time, we relied on questions based on faculty input and a study done by another institution, so there may have been some overlap of domains.5 There were numerous institutional barriers in technology and training during the near-overnight uptake of video care; the high level of satisfaction might reflect the transient nature of the technical challenges which improved over time. Other aspects of the pandemic may have also influenced responses about stress and satisfaction but were not measured. The study was limited to a single family medicine department, has limited gender data, does not assess age, and results are cross-sectional so cannot show change over time or causality. The small sample size means that we likely did not have adequate power to show differences in some of our assessments. Institutions have had variable experiences with respect to uptake and support for video visits, so the results may not be generalizable for all family physicians. Study strengths include the focus on physician experience, a high response rate within our department, and the very early assessment of video care.
Primary care clinicians are experiencing rapid uptake of virtual care in the setting of the COVID pandemic. Our survey suggests that these visits are acceptable and well-received by family physicians, including those new to this type of care. The efficiency and flexibility of video care may offer a novel way to reduce physician burnout and increase satisfaction with practice. These issues deserve additional research given the rapid shift across the country to virtual care.
References
- Dixon RF, Stahl JE. Virtual visits in a general medicine practice: a pilot study. Telemed J E Health. 2008;14(6):525-530. doi:10.1089/tmj.2007.0101
- Pflugeisen BM, Mou J. Patient satisfaction with virtual obstetric care. Matern Child Health J. 2017;21(7):1544-1551. doi:10.1007/s10995-017-2284-1
- Desko L, Nazario M. Evaluation of a clinical video telehealth pain management clinic. J Pain Palliat Care Pharmacother. 2014;28(4):359-366. doi:10.3109/15360288.2014.969875
- Polinski JM, Barker T, Gagliano N, Sussman A, Brennan TA, Shrank WH. Patients’ Satisfaction with and Preference for Telehealth Visits. J Gen Intern Med. 2016;31(3):269-275. doi:10.1007/s11606-015-3489-x
- Powell RE, Stone D, Hollander JE. Patient and health system experience with implementation of an enterprise-wide telehealth scheduled video visit program: mixed-methods study. JMIR Med Inform. 2018;6(1):e10. doi:10.2196/medinform.8479
- Beck CA, Beran DB, Biglan KM, et al; Connect.Parkinson Investigators. National randomized controlled trial of virtual house calls for Parkinson disease. Neurology. 2017;89(11):1152-1161. doi:10.1212/WNL.0000000000004357
- Müller KI, Alstadhaug KB, Bekkelund SI. A randomized trial of telemedicine efficacy and safety for nonacute headaches. Neurology. 2017;89(2):153-162. doi:10.1212/WNL.0000000000004085
- Russo JE, McCool RR, Davies L. VA Telemedicine: an analysis of cost and time savings. Telemed J E Health. 2016;22(3):209-215. doi:10.1089/tmj.2015.0055
- National Quality Forum. Creating a Framework to Support Measure Development for Telehealth: Final Report. https://www.qualityforum.org/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=85835. Washington, DC: National Quality Forum; 2017.
- Vogt EL, Mahmoud H, Elhaj O. Telepsychiatry: implications for psychiatrist burnout and well-being. Psychiatr Serv. 2019;70(5):422-424. doi:10.1176/appi.ps.201800465
- Moazzami B, Razavi-Khorasani N, Dooghaie Moghadam A, Farokhi E, Rezaei N. COVID-19 and telemedicine: immediate action required for maintaining healthcare providers well-being. J Clin Virol. 2020;126:104345. doi:10.1016/j.jcv.2020.104345
- Reliford A, Adebanjo B. Use of Telepsychiatry in pediatric emergency room to decrease length of stay for psychiatric patients, improve resident on-call burden, and reduce factors related to physician burnout. Telemed J E Health. 2019;25(9):828-832. doi:10.1089/tmj.2018.0124
- Gardner JS, Plaven BE, Yellowlees P, Shore JH. Remote telepsychiatry workforce: a solution to psychiatry’s workforce issues. Curr Psychiatry Rep. 2020;22(2):8. doi:10.1007/s11920-020-1128-7
- Marcin JP, Rimsza ME, Moskowitz WB; COMMITTEE ON PEDIATRIC WORKFORCE. The use of telemedicine to address access and physician workforce shortages. Pediatrics. 2015;136(1):202-209. doi:10.1542/peds.2015-1253
- Jetty A, Moore MA, Coffman M, Petterson S, Bazemore A. Rural ramily physicians are twice as likely to use telehealth as urban family physicians. Telemed J E Health. 2018;24(4):268-276. doi:10.1089/tmj.2017.0161



There are no comments for this article.