Background and Objectives: The proper documentation of Hierarchical Condition Category (HCC) codes is essential for risk-adjusted reimbursement, chart accuracy, and clinical communication within primary care, but represents a significant training gap in resident education. Our goal was to improve the understanding and confidence level of family medicine residents with HCC coding during outpatient primary care visits.
Methods: We developed and distributed a web-based, interactive module to family medicine residents at our academic institution. We assessed module impact through pre- and postsurveys focusing on knowledge, confidence, and experience with HCC coding.
Results: Twenty-eight of 48 preeducation surveys were returned (response rate of 58%), including 16 junior (PGY-1-2) and 12 senior (PGY-3-4) residents. A majority of residents answered each HCC knowledge question correctly. Median baseline confidence with HCC coding for all respondents was 4 (interquartile range [IQR]: 2, 6; scale 0-10; 10=most confident): senior residents 6 (IQR: 5, 7) versus junior residents 2 (IQR: 2, 4). Forty-six percent of respondents noted some previous education on HCC codes, including 75% of senior vs 25% of junior residents. Twenty-six residents completed the educational module. Posttest surveys (n=5, response rate: 19%) demonstrated median confidence of 7 (IQR: 4, 8.5).
Conclusions: Family medicine residents displayed a high degree of knowledge but low confidence with HCC coding. Posteducation surveys suggest the possibility of a positive impact of our e-module, though further intervention roll out and data collection are needed to evaluate this effect.
The Centers for Medicare and Medicaid Services (CMS) employs a risk-based reimbursement model where disease burden is captured by the documentation of International Classification of Diseases-10 (ICD-10) codes grouped into Hierarchical Condition Categories (HCC).1,2 When HCCs are inadequately captured for patients with known chronic conditions, this can be characterized as an “HCC gap,” that may have negative impacts on reimbursement, health record accuracy, and clinical communication. Our institution developed a multidisciplinary task force to effectively close the HCC Gap through quality improvement initiatives including direct patient scheduling, electronic health record workflow guides, and provider education, the latter of which led to the creation of a web-based, interactive e-module.
The creation of this e-module represents a unique effort in the landscape of educational interventions related to health care billing practices. Previous educational projects were focused either on inpatient coding practices3 or fee-for-service billing structures such as Evaluation and Management (E/M) codes.4-8 These projects and related surveys9-11 additionally identified that resident physicians serve as key foci of outpatient documentation and chronically report being underprepared in this domain. Therefore, our goal was to improve resident knowledge of and confidence in documentation of HCC diagnoses in the primary care setting though a web-based, interactive e-module.
Following approval from our institution’s family medicine residency program (4 years) and exemption from human subjects research granted by the institutional review board, we developed an e-module with three major sections: (1) review of value-based payment, (2) case-based illustration of core HCC coding concepts, and (3) description of ongoing initiatives and available resources. We presented a module draft to the institution’s department of e-learning, which created a web-based, interactive module presented on Compass.
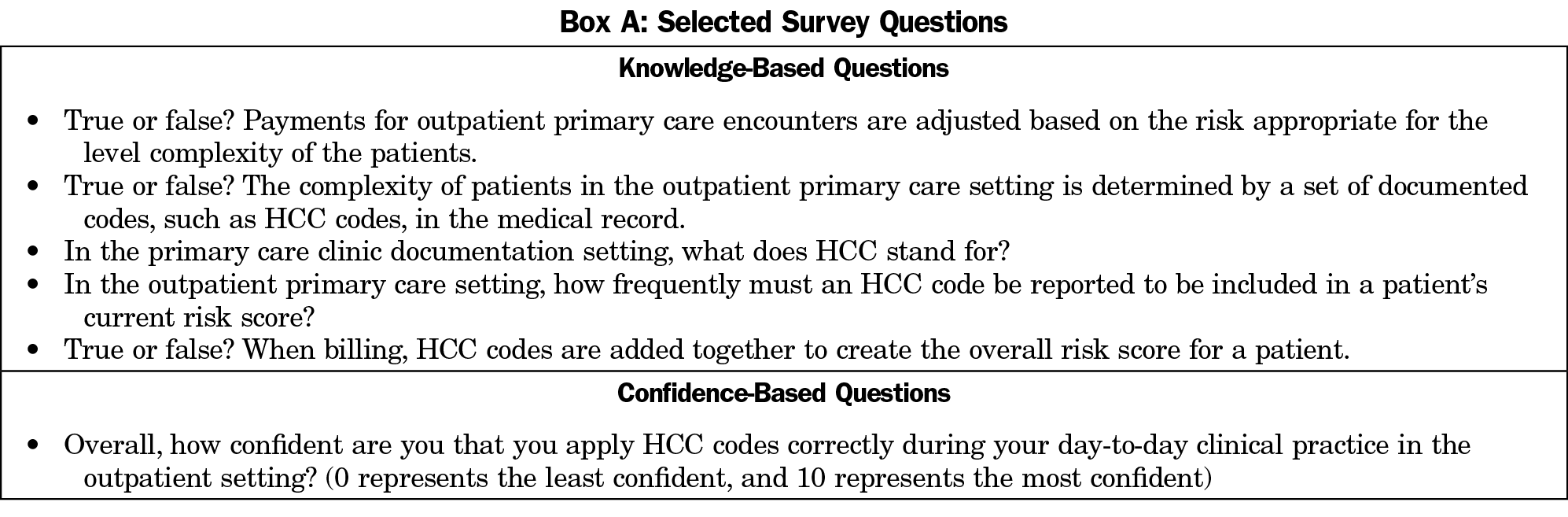
To assess the impact of the module, we created baseline and postmodule surveys. The baseline surveys (5 minutes) included 16 questions including basic demographic information (name [optional], postgraduate year, clinic site), knowledge of HCC coding principles (true/false, multiple choice), confidence with HCC coding (10-point Likert scale, 10=most confident), and previous experience with education related to HCC coding and documentation (Box A). The postmodule surveys (3 minutes) included all baseline survey questions except for questions that assessed for previous HCC education. We developed, refined, and stored the surveys on the secure, password-protected Qualtrics software. Surveys were distributed electronically to all family medicine residents with periodic email reminders for completion; no compensation was offered. We sent the postmodule survey 3 months following the initial distribution of the e-module to those who had completed the module.
As a quality improvement initiative, we collected the data for descriptive analysis and presentation to inform subsequent plan, do, study, act cycles. We deidentified and compiled survey data using the appropriate descriptive statistics. We created representative subgroups including junior residents (PGY-1-2) and senior residents (PGY-3-4). All data were stored on the Qualtrics software.
Baseline surveys were completed by 28 of the 48 residents included in the initial distribution for a response rate of 58.3%. Of the respondents, 16 were junior residents and 12 were senior residents.
Baseline knowledge (Figure 1A) assessment included true/false questions pertaining to risk adjustment in primary care, HCC use for coding complexity, and HCC additive property that were answered correctly by 82.1% (23/28), 89.3% (25/28), and 82.1% (23/28 responders) of respondents, respectively. The two other questions had lower correct response rates including HCC definition (multiple choice, 50% correctly, 14/28), and HCC documentation frequency (multiple choice, 60.7% correctly, 17/28 responders). Subgroup analysis (Figure 1B) shows the percentages of respondents answering correctly by level of training (senior vs junior resident) for each of the knowledge-based questions.
Residents noted that baseline median confidence with HCC coding and documentation was 4 (interquartile range [IQR] 25%-75%: 2, 6; max=9, min=1; scale from 0-10 with 10 as most confident). Senior resident respondents noted a median confidence of 6 (IQR: 5, 7, max=9, min=0) and junior residents noted a median confidence of 2.5 (IQR: 2, 4, max=6, min=1).
At baseline, 13 of 28 respondents (46%) indicated that they had prior education regarding HCC codes including 9 of 12 senior residents (75%) and 4 of 16 junior residents (25%). The most commonly reported education was “seminar or lecture” (6 respondents) and “required orientation material” (6 respondents).
The e-module was completed by 26 of the 48 residents, for a response rate of 54%. We distributed posteducation surveys to the 26 residents who completed the module, and five completed surveys were returned (19%). All respondents answered all knowledge-based questions correctly. Median confidence level with HCC coding and documentation was 7 (IQR: 4, 8.5, max=9, min=4).
Our project details the novel experience of creating an interactive, web-based learning module to improve the knowledge, confidence, and awareness of chronic disease coding and documentation through the use of HCC codes. Our data show that residents hold some knowledge but low confidence with the use of HCC codes in their outpatient primary care roles. Knowledge was higher with senior residents who also reported a higher percentage of previous education with HCC coding prior to our learning module. Postmodule surveys show that our educational module may be able to boost both knowledge and confidence with HCC coding, though we were limited by a low response rate, lack of HCC coding data, and potential selection bias. In future applications of this e-module we intend to further assess the impact of our module, including the impact on resident use of HCC documentation. In all, our experience can serve as a starting point for efforts to improve education of primary care physicians in the realm of coding and documentation for chronic conditions.
Acknowledgments
The authors acknowledge the many efforts of the OHSU Ambulatory Documentation Improvement team, Department of e-learning, and Family Medicine Residency program for their support, assistance, and encouragement.
Presentations: This study was presented as a poster at the following events:
Oregon Academy of Family Physicians Virtual Poster Session, Poster Presentation, April 2020.
STFM Virtual Conference on Practice and Quality Improvement, September, 2020.
References
- Yeatts JP, Sangvai D. HCC Coding, risk adjustment, and physician income: what you need to know. Fam Pract Manag. 2016;23(5):24-27.
- Pope GC, Kautter J, Ellis RP, et al. Risk adjustment of Medicare capitation payments using the CMS-HCC model. Health Care Financ Rev. 2004;25(4):119-141.
- Spellberg B, Harrington D, Black S, Sue D, Stringer W, Witt M. Capturing the diagnosis: an internal medicine education program to improve documentation. Am J Med. 2013;126(8):739-743.e1. doi:10.1016/j.amjmed.2012.11.035
- Kelley KA, Hoops HE, Palmer L, Cohen NA, Brasel KJ. Implementation of a medical coding curriculum for surgery residents. Am J Surg. 2019;217(5):834-838. doi:10.1016/j.amjsurg.2019.02.027
- Skelly KS, Bergus GR. Does structured audit and feedback improve the accuracy of residents’ CPT E&M coding of clinic visits? Fam Med. 2010;42(9):648-652.
- Benke JR, Lin SY, Ishman SL. Directed educational training improves coding and billing skills for residents. Int J Pediatr Otorhinolaryngol. 2013;77(3):399-401. doi:10.1016/j.ijporl.2012.11.039
- Ghaderi KF, Schmidt ST, Drolet BC. Coding and billing in surgical education: a systems-based practice education program. J Surg Educ. 2017;74(2):199-202. doi:10.1016/j.jsurg.2016.08.011
- Nguyen D, O’Mara H, Powell R. Improving coding accuracy in an academic practice. US Army Med Dep J. 2017;(2-17):95-98.
- Fakhry SM, Robinson L, Hendershot K, Reines HD. Surgical residents’ knowledge of documentation and coding for professional services: an opportunity for a focused educational offering. Am J Surg. 2007;194(2):263-267. doi:10.1016/j.amjsurg.2006.11.031
- Breitwieser D, Adye W, Arvidson M. Resident evaluation of current practice management training. J Fam Pract. 1981;13(7):1063-1064.
- Andreae MC, Dunham K, Freed GL. Inadequate training in billing and coding as perceived by recent pediatric graduates. Clin Pediatr (Phila). 2009;48(9):939-944. doi:10.1177/0009922809337622




There are no comments for this article.