Background and Objectives: Burnout impacts medical students, residents, and practicing physicians. Existing research oversimplifies characteristics associated with burnout. Our study examined relationships between burnout, depressive symptoms, and evidence-based risk factors.
Methods: Our study questions were part of a larger survey conducted by the Council of Academic Family Medicine Educational Research Alliance (CERA), from May 9-23, 2020. Three emails were used to recruit a national sample of family medicine residents (n=283; questions completed via Survey Monkey). We determined descriptive statistics (frequency, means) for demographic and work environment characteristics, UCLA Loneliness Scale items, health behaviors, burnout (emotional exhaustion, depersonalization), and depressive symptoms. Multivariate data analysis included developing three logistic regression (LR) equations (emotional exhaustion, depersonalization, depressive symptoms) based on four blocks of potential risk factors (demographics, work environment characteristics, UCLA Loneliness items, and health behaviors).
Results: Rates of psychological distress included 33.1% emotional exhaustion, 31.1% depersonalization, and 53.0% depressive symptoms. We determined stepwise forward-entry LR models for emotional exhaustion (feel isolated OR=6.89, low quality of wellness program OR=5.91, and low companionship OR=4.82); depersonalization (feel isolated OR=5.59, low quality of wellness program OR=15.11, graduate US osteopathic medical school OR=0.329, and African American OR=7.55); and depressive symptoms (feel isolated OR=5.31, inadequate time for restful sleep OR=0.383, and no dependent children OR=2.14).
Conclusions: Current findings document substantial social disconnection, substandard residency wellness programs, inadequate time for exercise, sleep, and other forms of self-care in addition to substantial levels of emotional exhaustion, depersonalization, and depressive symptoms. We explore implications for the design of future burnout prevention efforts and research.
Burnout is a stress syndrome classically defined by high emotional exhaustion, high depersonalization, and low personal accomplishment.1,2 Burnout adversely impacts health care professionals, organizations and patients.3-6 Physician burnout rates are on the rise.7,8 Family physician burnout rates of 30% to 50% are at historically-high levels.9-11
Physician burnout is an area of intense research.7,9,10,16 Elevated burnout rates begin in medical school, with peak rates during first-year studies and clinical training before residency.17 Medical students with high burnout are more likely to experience burnout during residency.18 Resident physicians who experience burnout are more likely to report burnout following residency.19 Resident-focused research has found that burnout and depression are associated with increased rates of harmful patient errors, lower-quality patient care, decreased emotional intelligence, and higher explicit and implicit racial bias.6, 20,21
The Accreditation Council for Graduate Medical Education (ACGME) recognizes the importance of resident well-being on patient care. As the risk for burnout from medical school forward has become apparent, mitigation efforts have occurred .17-19, 21-25 There is limited empiric data about the ideal focus for burnout mitigation strategies.2 Current research suggests individual and environmental factors that mitigate burnout.3, 26-30 Available research tends to oversimplify individual factors such as resilience and wellness.10, 23,24,27,28 There is research to suggest that poorly-developed social networks with associated feelings of loneliness increase burnout.31
There is also data supporting the role of individual and environmental health behaviors limiting burnout. Important health behaviors include restful sleep, regular exercise, engagement with high-quality wellness programs, and residency schedules allowing for personal self-care (eg, health appointments, quality-time with family and friends, regular sleep).32, 22-25 As mentioned, the availability and effective deployment of social resources mitigates the development of burnout.29,30,33 The purpose of our study was (1) to measure conceptually-sound, empirically-derived individual and environmental risk factors; and (2) to examine relationships between these variables and measures of psychological distress including burnout (specifically emotional exhaustion, depersonalization) and depressive symptoms.16,22-25
Survey questions were part of a larger omnibus survey conducted by the Council of Academic Family Medicine Educational Research Alliance (CERA). The methodology of the CERA Family Medicine Resident Survey has been described elsewhere.34 The sampling frame for the survey was 5,000 resident members of the American Academy of Family Physicians. Email invitations to participate were delivered with the survey utilizing the online program SurveyMonkey. Reminder emails were sent between 4 to 10 days. The response rate was 5.66% (283/5,000). The American Academy of Family Physicians Institutional Review Board approved the project in April 2020. Data were collected from May 9, 2020 through May 23, 2020.
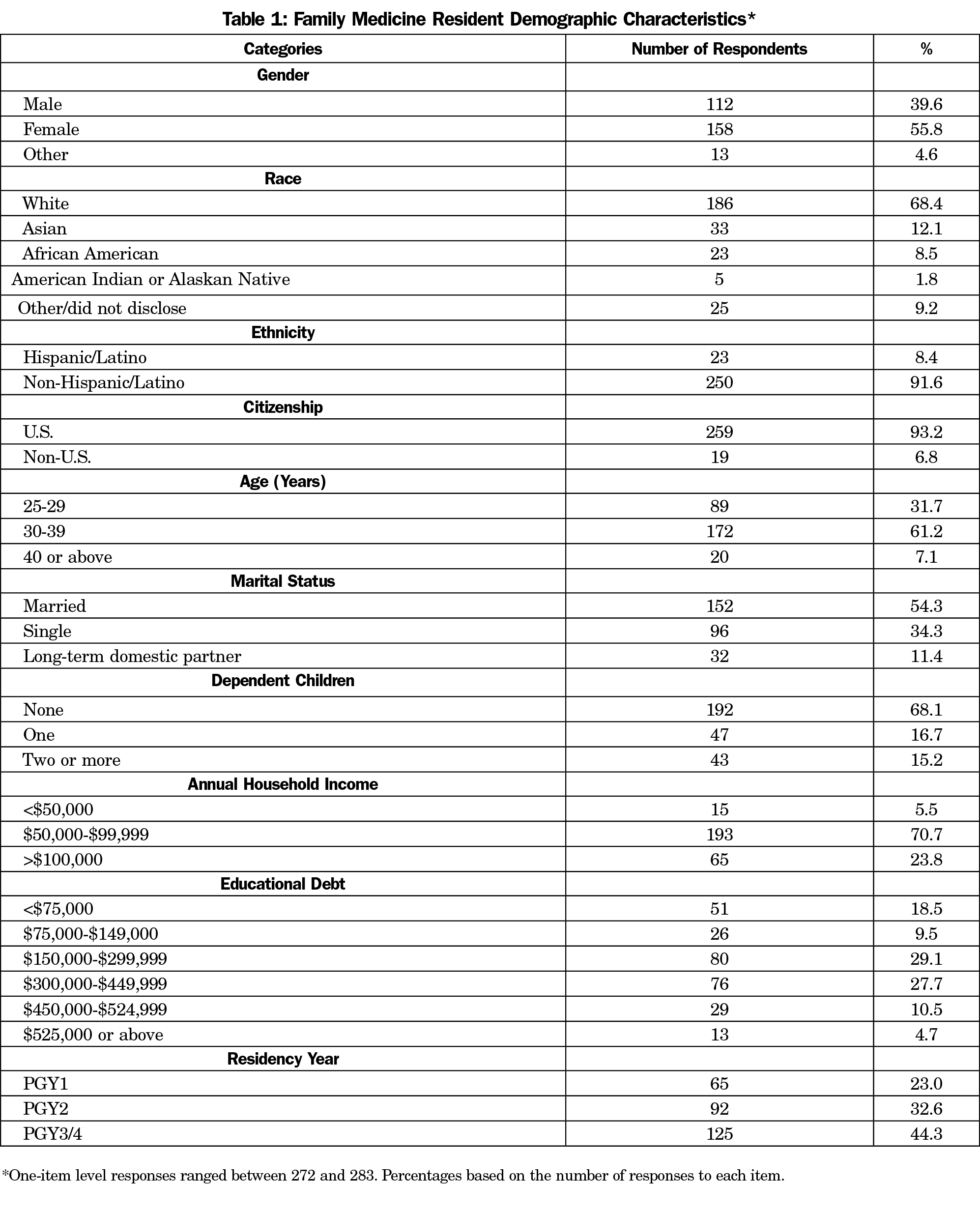
The survey response rate was disappointing. To understand potential sample bias, we entered into a data-sharing agreement with the American Board of Family Medicine to contrast sample demographic characteristics with a national sample of Family Medicine residents (n=13,556 as of May 1, 2020). Based on χ2 testing, our obtained sample was equivalent to this national sample for gender, ethnicity (Hispanic/Latino vs not), and educational debt (P<.05). Our sample was older (eg, 31.7% vs 40.5% age 29 years or below), farther in training (eg, 44.3% vs 32.0% PGY3/4), and less racially diverse (eg, 12.1% vs 23.2% Asian).
Demographic data is a portion of recurring CERA surveys. Our research team developed specific questions included on the 2020 survey related to resident physician burnout based upon prior research and established scales.
A three-item version of the UCLA Loneliness Scale has acceptable reliability data when contrasted to the 20-item parent scale (α=0.72; correlation between the 3- and 20-item scales=0.82). We used this three-item scale was used to assess a potential relationship between resident physician loneliness and burnout. We evaluated the three items, “I lack companionship,” “I feel left out,” and, “I feel isolated,” on a 4-point scale (0=never, 1=hardly ever, 2=some of the time, 3=often).35
Several health behaviors have been related to resident physician burnout, including adequate time for personal self-care (eg, health appointments, quality time with family/friends), resident wellness program quality, regular physical exercise, and restful sleep.14-16, 21,22
A two-item measure of burnout derived from the Maslach Burnout Inventory (MBI), has been developed for physicians. This measure assesses the dimensions of emotional exhaustion (“I feel burned out from my work”) and depersonalization (“I have become more callous towards people since I took this job”), with strong correlations between these single-item measures (0.76-0.83 for emotional exhaustion; 0.61-0.72 for depersonalization) and corresponding MBI scale scores.36 These single-item measures are also predictive of full MBI scale scores.37 Our study employed this 2-item burnout measure with each item assessed on a 7-point scale (0=never, 1=a few times a year, 2=once a month or less, 3=a few times a month, 4=once per week, 5=a few times a week, 6=every day).
Using Patient Health Questionnaire-2 (PHQ-2), the single question, “In the past 2 weeks, how often have you felt down, depressed, or hopeless?” was endorsed by 93% of people with clinical depression as determined by a validated clinical interview (0=not at all, 1=several days, 2=more than half the days, 3=nearly every day).38-39
Data Analysis Plan
Univariate analyses included frequency counts, means, and standard deviations of study variables (demographic characteristics, work environment characteristics, health behaviors, and UCLA Loneliness items). We developed frequency counts for psychological distress based on cut-points suggestive of functional impact (once per week or more for emotional exhaustion and depersonalization, and several days or more per week for depressive symptoms).
Multivariate data analysis began with four blocks of variables potentially related to psychological distress (emotional exhaustion, depersonalization, and depressive symptoms): demographic variables, work environment characteristics, health behaviors, and loneliness. χ2 testing determined significant associations (P<.05) between key variables and each distress measure. A significant χ2 association with resident distress was required for inclusion in subsequent logistic regression (LR) equations. We determined three binary LR equations based upon a stepwise forward-entry approach building sequentially upon a null model based on adding the variable meeting best-fit statistical criteria.40
Family Medicine Resident Demographic Characteristics
Resident demographic characteristics are shown in Table 1. The typical study resident was female (57.8%), White (68.4%), non-Hispanic/Latino (91.6%), a US citizen (93.2%), 30-39 years old (61.2%), married or in a long-term domestic partnership (65.7%), and childless (68.1%). The modal annual household income was $50,000-$99,999 (70.7%); modal education debt was $150,000-$299,999 (29.1%). Postgraduate family medicine trainees were part of this study (PGY1=23.0%, PGY2=32.6%, PGY3/4=44.3%).
Family Medicine Resident Work Environment Characteristics
The typical study participant worked at a community-based, university-affiliated residency (48.9%). Training sites from nine distinct regions of the United States were represented, the three most common being East North Central (WI, MI, OH, IN, IL; 18.4%), South Atlantic (PR, FL, GA, SC, NC, VA, DC, WV, DE, MD; 16.2%), and Pacific (WA, OR, AK, HI; 15.2%). The modal residency community size was 150,000-499,999 (28.8%). The modal residency size was 19-31 residents (42.7%). The location and accreditation of participant medical schools was US 47.6% allopathic, 29.3% US osteopathic, and 23.1% international.
Individual and Environmental Factors
Regarding social networks, nearly half of our resident sample reported feeling a lack of companionship some of the time or often (48.2%). Over half of our residents reported feeling left out some of the time or often (54.5%). Even more resident physicians reported feelings of isolation some of the time or often (61.3%).
For health behaviors, most respondents reported that formal and informal residency time expectations left only a few times monthly or less for personal self-care (eg, health appointments, quality time with family/friends, exercise, restful sleep; 62.4%). Nearly half reported the quality of their resident wellness program as fair or poor (48.6%). Over half reported regular physical exercise a few times monthly or less (60.6%). A substantial minority reported getting restful sleep a few times monthly or less (28.8%).
Family Medicine Resident Distress
Regarding psychological distress, there were no gender differences across measures, therefore, aggregate responses are provided. One-third (33.1%) reported once a week or more often feeling burned out from their work as a family medicine resident (emotional exhaustion). A similar proportion (31.3%) reported once a week or more often feeling that they had become more callous towards people since becoming a family medicine resident (depersonalization). Over half (53.0%) reported several days of the past two weeks (or more often) feeling down, depressed, or hopeless (depressive symptoms).
Logistic Regression Models
Emotional Exhaustion. Significant univariate associations (P<.05) with emotional exhaustion included age (χ2=11.13, P<.05, older), lack of companionship (χ2=16.64, P<.001, lack of), feeling left out (χ2=33.34, P<.001, more frequently), and feeling isolated (χ2=30.11, P<.001, more frequently); time for self-care (χ2=49.06, P<.001, inadequate time), quality of wellness program (χ2=36.52, P<.001, lower quality), and time for restful sleep (χ2=13.33, P<.01, inadequate time). The final stepwise forward-entry LR model (Table 2) tested the sequential best-fit association with emotional exhaustion (presented in order of model entry): feel isolated (OR=6.89, 95% CI=2.17-18.49, P<.001), lower quality of wellness program (OR=5.91, CI=0.382-91.24 P<.001), and lack of companionship (OR=4.82, CI=1.54-15.14, P<.007).
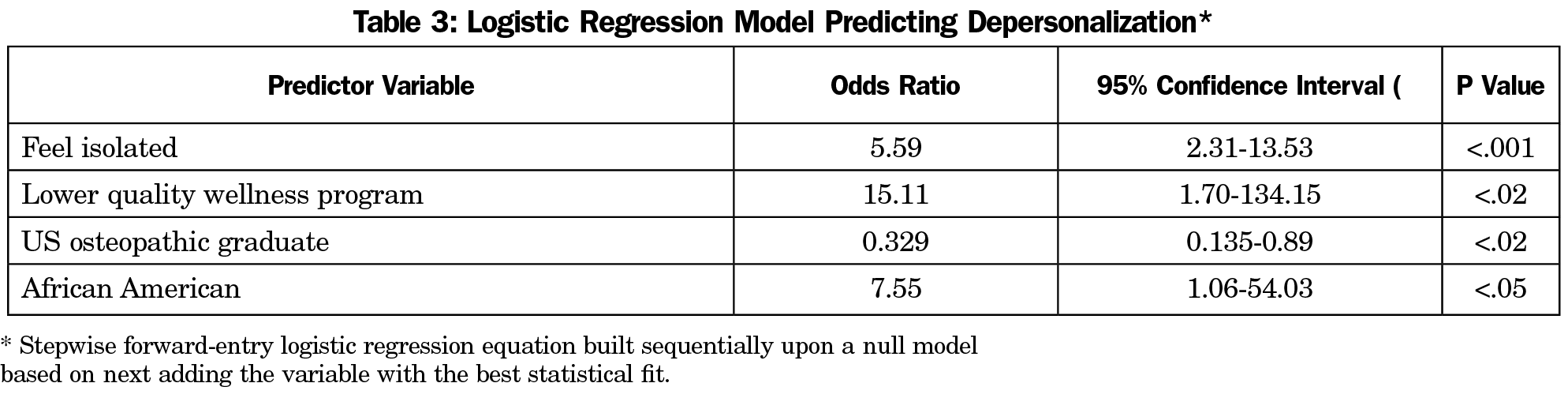
Depersonalization. Significant univariate associations (P<.05) with depersonalization included race ( χ2=55.64, P<.003, African American), location and accreditation of medical school (χ2=35.98, P<.001, osteopathic medical school), lack companionship (χ2=19.87, P<.001, lack of), feel left out (χ2=23.04, P<.001, more frequently), feel isolated ( χ2=18.87, P<.001; more frequently), time for self-care (χ2=12.07, P<.02, inadequate time), wellness program quality (χ2=21.04, P<.001, lower quality), and time for restful sleep (χ2=13.72, P<.008, inadequate time). The final stepwise forward-entry LR model (Table 3) tested the sequential best-fit association with depersonalization (presented in order of model entry), feel isolated (OR=5.59, CI=2.31-13.53, P<.001), lower quality of wellness program (OR=15.11, CI=1.70-134.15, P<.02), graduate US osteopathic medical school (OR=0.329, CI=0.135-0.89, P<.02), and African American (OR=7.55, CI=1.06-54.03, P<.05).
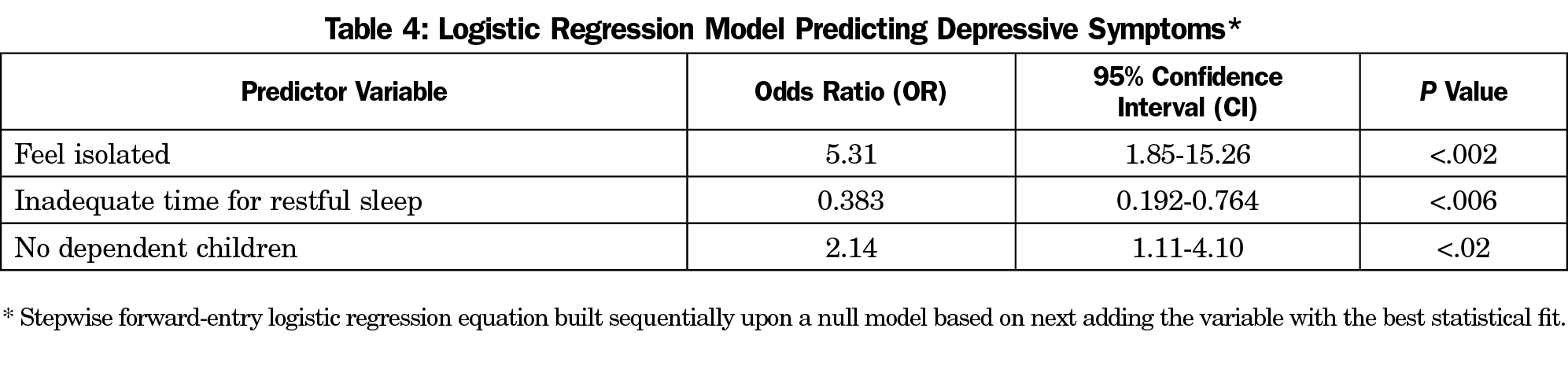
Depressive symptoms. Depressive symptoms were significantly associated with the following univariate variables: gender (χ2=12.54, P<.01, female); dependent children (χ2=5.14, P<.02, none), annual household income (χ2=10.66, P<.03, lower income); lack companionship (χ2=22.11, P<.001, lack of); feel left out (χ2=33.92, P<.001, more frequently); feel isolated (χ2=48.83, P<.001, more frequently); time for self-care (χ2=18.44, P<.001, inadequate time), wellness program quality (χ2= 15.16, P<.004, lower quality), and time for restful sleep (χ2=23.36, P<.001, inadequate time). The final stepwise forward-entry LR model (Table 4) tested the sequential best fit association with depressive symptoms (presented in order of model entry): feel isolated (OR=5.31, CI=1.85-15.26, P<.002), inadequate time for restful sleep (OR=0.383, CI=0.192-0.764, P<.006), no dependent children (OR=2.14, CI=1.11-4.10, P<.02).
Descriptive results are consistent with prior studies.2,6-9,12-14, 17,18,21,22 The confirmatory nature of our findings underscore the need for actions aimed at mitigating risk factors for resident burnout.
On a practical level, the robust LR risk factors may be proposed as burnout intervention targets. For example, LR findings for emotional exhaustion, depersonalization, and depressive symptoms all highlight the lack of social connectedness and loneliness as a major factor contributing to resident burnout. It is important to note that this study was conducted 2 months into the start of the COVID-19 pandemic, when physical isolation in both personal and professional arenas was at an all-time high. At that time, many institutions prohibited in-person gatherings, all didactics were virtual, and many even engaged in virtual patient care. While the degree of physical isolation has lessened, our professional work is one that requires us to miss important life events for the sake of patient care, engendering feelings of isolation and placing family medicine residents at substantial risk for burnout and depressive symptoms.31 Our study emphasizes the significance of residency programs promoting activities that build community and connectedness among their team.
Further, it appears that reports of mediocre resident wellness curriculum efforts are associated with increased levels of depersonalization, leading to burnout. Much has been published on examples of successful resident wellness curriculum in various programs and specialties. Many involve didactics on mindfulness and resiliency, while others focus on practical sessions on various aspects of physical care (sleep, nutrition, fitness) or personal care (financial literacy, building a support network, mental health). Resources of specific programs as well as individual needs of residents should be considered when designing an effective resident wellness curriculum.
Several additional demographic factors were of note regarding LR results. For example, being African American was associated with higher feelings of depersonalization. It is well established that physicians of color (medical students, resident physicians, practicing physicians) experience multiple incidents of racism in the context of not feeling fully supported by the institutions within which they work. Therefore, diversity, inclusion, and equity efforts aimed at producing system-level changes to support the basic humanity of physicians of color are a critical remedy.41,42
Graduating from an osteopathic (vs allopathic) medical school was also associated with higher feelings of depersonalization. In graduate medical education, there has been historical bias towards osteopathic physicians (DOs) vs allopathic physicians (MDs). Lingering experiences and negative feelings associated with osteopathic training may cause some to feel underappreciated with resultant depersonalization.43 Efforts targeting cultural change within graduate medical education must be undertaken to ensure that all qualified osteopathic residents feel fully accepted and supported in their training programs and future practice.44
Notably, the majority of our sample is female (55.8%) with two-thirds aged 30 years or above. For some of these female residents, there may be an internal conflict regarding the impact of their professional activities being balanced against their personal desires and plans resulting in depressive symptoms (eg, timing of having a child or not having a child, care responsibilities for aging family members, working within a professional culture that remains highly demanding).45
In aggregate, the multivariate findings suggest that family medicine residency programs should be actively promoting opportunities for professional and personal social connectivity amongst resident physicians (and with faculty mentors). Programs should also actively facilitate programs, policies, and procedures that consistently provide residents with needed resources for remaining healthy. These could include things such as evidence-based, resident-centered wellness programs and schedule structuring to allow sufficient time and flexibility for adequate self-care, including adequate sleep, health appointments, and assistance with facilitating regular exercise.
Finally, we would be remiss if we did not note that this study identified four subgroups with unique vulnerability to either feelings of depersonalization or depressive symptoms. In particular, residents who were either African American or trained at osteopathic medical schools self-reported higher levels of depersonalization. Female family medicine residents reported higher levels of depressive symptoms than male resident physicians. Residents without children also reported higher depressive symptoms. We recommend ongoing resident wellness efforts to address the unique needs of African American residents, osteopathic residents, female, and childless residents with quantitative and qualitative designs to assess the efficacy of such efforts.
Study results are interpreted considering study strengths and weaknesses. Strengths of our study include robust literature review to support selected variables, CERA methodology, use of standardized measures, and an a priori data analysis plan. The primary study weakness was the modest sample size, however, the contrast of demographic variables between our sample and a national sample of family medicine residents suggested equivalence regarding gender, ethnicity (Hispanic/Latino vs not), and educational debt. Modest sample bias (obtained sample was older, farther in training, and less racially diverse) should be considered when interpreting study results. Not measuring low personal accomplishment as a dimension of burnout might also limit findings. Our multivariate LR findings add to existing peer-reviewed literature and provide statistical control for sampling bias. Replication in future studies is needed.
References
- Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory. 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996.
- McCray LW, Cronholm PF, Bogner HR, Gallo JJ, Neill RA. Resident physician burnout: is there hope? Fam Med. 2008;40(9):626-632.
- Hobfoll SE, Freedy JR. Conservation of resources: A general stress theory applied to burnout. In: Schaufeli WB, Maslach C, Merek T, eds. Series in applied psychology: Social issues and questions. Professional burnout: recent developments in theory and research. Philadelphia, PA: Taylor & Francis; 1993:115-133.
- Olson KD. Physician burnout-A leading indicator of health system performance? Mayo Clin Proc. 1608-11;2017(Nov).
- Schaufeli WB, Leiter MP, Maslach C. Burnout: 35 years of research and practice. Career Dev Int. 2009;14(3):204-230. doi:10.1108/13620430910966406
- Brunsberg KA, Landrigan CP, Garcia BM, et al. Association of Pediatric Resident Physician Depression and Burnout With Harmful Medical Errors on Inpatient Services. Acad Med. 2019;94(8):1150-1156. doi:10.1097/ACM.0000000000002778
- Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377-1385. doi:10.1001/archinternmed.2012.3199
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600-1613. doi:10.1016/j.mayocp.2015.08.023
- Puffer JC, Knight HC, O’Neill TR, et al. Prevalence of burnout in board certified family physicians. J Am Board Fam Med. 2017;30(2):125-126. doi:10.3122/jabfm.2017.02.160295
- Porter M, Hagan H, Klassen R, Yang Y, Seehusen DA, Carek PJ. Burnout and resiliency among family medicine program directors. Fam Med. 2018;50(2):106-112. doi:10.22454/FamMed.2018.836595
- Buck K, Williamson M, Ogbeide S, Norberg B. Family Physician Burnout and Resilience: A Cross-Sectional Analysis. Fam Med. 2019;51(8):657-663. doi:10.22454/FamMed.2019.424025
- Dyrbye LN, Thomas MR, Massie FS, et al. Burnout and suicidal ideation among U.S. medical students. Ann Intern Med. 2008;149(5):334-341. doi:10.7326/0003-4819-149-5-200809020-00008
- Khan A, Teoh KRH, Islam S, Hassard J. Psychosocial work characteristics, burnout, psychological morbidity symptoms and early retirement intentions: a cross-sectional study of NHS consultants in the UK. BMJ Open. 2018;8(7):e018720. doi:10.1136/bmjopen-2017-018720
- Rassolian M, Peterson LE, Fang B, et al. Workplace factors associated with burnout of family physicians. JAMA Intern Med. 2017;177(7):1036-1038. doi:10.1001/jamainternmed.2017.1391
- West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516-529. doi:10.1111/joim.12752
- Psenka TM, Freedy JR, Mims LD, et al. A cross-sectional study of United States family medicine residency programme director burnout: implications for mitigation efforts and future research. Fam Pract. 2020;37(6):772-778. doi:10.1093/fampra/cmaa075
- Hansell MW, Ungerleider RM, Brooks CA, Knudson MP, Kirk JK, Ungerleider JD. Temporal trends in medical student burnout. Fam Med. 2019;51(5):399-404. doi:10.22454/FamMed.2019.270753
- Dyrbye LN, Burke SE, Hardeman RR, et al. Assocation of clinical specialty choice with symptoms of burnout and career choice regret among US resident physicians. JAMA. 2018;320(11):1114-1130. doi:10.1001/jama.2018.12615
- Raimo J, LaVine S, Spielmann K, et al. The correlation of stress in residency with future stress and burnout: A 10-year prospective cohort study. J Grad Med Educ. 2018;10(5):524-531. doi:10.4300/JGME-D-18-00273.1
- Dyrbye L, Herrin J, West CP, et al. Association of Racial Bias With Burnout Among Resident Physicians. JAMA Netw Open. 2019;2(7):e197457. doi:10.1001/jamanetworkopen.2019.7457
- Ricker M, Maizes V, Brooks AJ, Lindberg C, Cook P, Lebensohn P. A Longitudinal Study of Burnout and Well-being in Family Medicine Resident Physicians. Fam Med. 2020;52(10):716-723. doi:10.22454/FamMed.2020.179585
- Lebensohn P, Dodds S, Benn R, et al. Resident wellness behaviors: relationship to stress, depression, and burnout. Fam Med. 2013;45(8):541-549.
- Penwell-Waines L, Runyan C, Kolobova I, et al. Making sense of family medicine resident wellness curricula: a delphi study of content experts. Fam Med. 2019;51(8):670-676. doi:10.22454/FamMed.2019.899425
- Gardiner P, Filippelli AC, Lebensohn P, Bonakdar R. The incorporation of stress management programming into family medicine residencies-results of a national survey of residency directors: a CERA study. Fam Med. 2015;47(4):272-278.
- Busireddy KR, Miller JA, Ellison K, Ren V, Qayyum R, Panda M. Efficacy of interventions to reduce resident physician burnout: A systematic review. J Grad Med Educ. 2017;9(3):294-301. doi:10.4300/JGME-D-16-00372.1
- Brennan J, McGrady A. Designing and implementing a resiliency program for family medicine residents. Int J Psychiatry Med. 2015;50(1):104-114. doi:10.1177/0091217415592369
- Card AJ. Physician burnout: resilience training is only part of the solution. Ann Fam Med. 2018;16(3):267-270. doi:10.1370/afm.2223
- Nedrow A, Steckler NA, Hardman J. Physician resilience and burnout: can you make the switch? Fam Pract Manag. 2013;20(1):25-30.
- Hobfoll SE, Freedy J, Lane C, Geller P. Conservation of Social Resources: social support resource theory. J Soc Pers Relat. 1990;7(4):465-478. doi:10.1177/0265407590074004
- Halbesleben JR. Sources of social support and burnout: a meta-analytic test of the conservation of resources model. J Appl Psychol. 2006;91(5):1134-1145. doi:10.1037/0021-9010.91.5.1134
- Shapiro J, Zhang B, Warm EJ. Residency as a social network: Burnout, loneliness, and social network centrality. J Grad Med Educ. 2015;7(4):617-623. doi:10.4300/JGME-D-15-00038.1
- Ofei-Dodoo S, Callaway P, Engels K. Prevalence and etiology of burnout in a community-based graduate medical education system: A mixed-method study. Fam Med. 2019;51(9):766-771. doi:10.22454/FamMed.2019.431489
- Freedy JR, Hobfoll SE. Stress inoculation for reduction of burnout: A Conservation of Resources approach. Anxiety Stress Coping. 1994;6(4):311-325. doi:10.1080/10615809408248805
- Mainous AG III, Seehusen D, Shokar N. CAFM Educational Research Alliance (CERA) 2011 Residency Director survey: background, methods, and respondent characteristics. Fam Med. 2012;44(10):691-693.
- Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. 2004;26(6):655-672. doi:10.1177/0164027504268574
- West CP, Dyrbye LN, Satele DV, Sloan JA, Shanafelt TD. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. 2012;27(11):1445-1452. doi:10.1007/s11606-012-2015-7
- West CP, Dyrbye LN, Sloan JA, Shanafelt TD. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med. 2009;24(12):1318-1321. doi:10.1007/s11606-009-1129-z
- Kroenke K, Spitzer RL, Williams JBW. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284-1292. doi:10.1097/01.MLR.0000093487.78664.3C
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-613. doi:10.1046/j.1525-1497.2001.016009606.x
- Cohen BH. Explaining psychological statistics. 3rd ed. Hoboken, NJ: John Wiley & Sons; 2013.
- Serafini K, Coyer C, Brown Speights J, et al. Racism experience by physicians of color in health care setting. Fam Med. 2020;52(4):282-287. doi:10.22454/FamMed.2020.384384
- de Bourmont SS, Burra A, Nouri SS, et al. Resident physician experience with and response to biased patients. JAMA Netw Open. 2020;3(11):e2021769. doi:10.1001/jamanetworkopen.2020.21769
- Eckberg DL. The dilemma of osteopathic physicians and the rationalization of medical practice. Soc Sci Med. 1987;25(10):1111-1120. doi:10.1016/0277-9536(87)90352-2
- McClain EK. Changes in osteopathic medical education: the journey continues. J Am Osteopath Assoc. 2017;117(4):208-210. doi:10.7556/jaoa.2017.037
- Paurel, A. Why women leave medicine. AAMC News. Published October 1, 2019. Accessed February 23, 2021. https://www.aamc.org/news-insights/why-women-leave-medicine




There are no comments for this article.